Although it is a case by case basis, with careful diagnosis and treatment, patients with septic large joints may have optimal outcomes.
Dr. Jesse A. Raszewski, Department of Orthopaedics, Kettering Health Network, Grandview Medical Center, 155 Delano Drive, Pittsburgh, PA 15236, United States. E-mail: jesse.raszewski@gmail.com
Introduction: Identifying and determining appropriate treatment of adult hip septic arthritis (SA) can be quite challenging. Although rare, the annual incidence of this diagnosis is approximately 8 cases per 100,000 patients. The timing of patient symptoms is wide spread. The presentation may be acute, subacute, or even chronic, and moreover, the disease process may be masked by an underlying etiology. Once diagnosed, SA requires rapid and aggressive treatment.
Case Report:A 67-year-old patient presented with left hip pain. Physical examination shifted the differential diagnosis from osteoarthritis to a possible septic joint. Elevated inflammatory markers were revealed. Joint aspiration was obtained, which demonstrated rare Group G streptococcus. Two-stage hip arthroplasty was performed. Intra-operative cultures still reveal no growth of bacteria, and the patient is progressing well.
Conclusion: Adult septic hip arthritis is a rare diagnosis. Hence, a proper history, physical examination, infectious laboratory workup is important. The treatment of the condition is based on the duration of symptoms and the physician’s clinical gestalt.
Keywords: Hip joint, septic arthritis, arthroplasty, two-stage revision.
The diagnosis and treatment of the adult hip septic arthritis (SA) can be quite challenging [1]. SA in adults within the United States is approximately 8 cases/100,00 patients annually [1]. Although rare, each case and treatment can accumulate a total cost of upwards of 10,000 dollars [2].
Symptoms may present at different times in the presentation, moreover, the disease process may be masked by a underlying etiology that can delay diagnosis [1]. Risk factors for SA are rheumatologic disease, skin infections, trauma, immunosuppressed state, corticosteroid joint injection, or joint procedure [1]. Once diagnosed, SA requires rapid and aggressive treatment. The infection may seed the hip by hematogenous spread or by direct inoculation [1]. An inflammatory response is triggered once the hip becomes colonized and the bacteria proliferate.
An increase in inflammatory modulators, such as reactive oxygen species, is a product of the immune response, which ultimately leads to joint destruction [1]. The bacteria most commonly responsible for this pathology also contribute to the pathogenesis of the disease. Staphylococcus aureus can express virulence that induces further tissue damage [1]. Patient presentation will exemplify severe hip or groin pain, with an inability to bear weight [1]. The absence of fever does not rule out SA, since only 30-60% of cases have a fever upon initial presentation [3]. On physical examination, the lower extremity of the patient could present as flexed and externally rotated, and exhibit pain with internal rotation of the hip joint [1]. To confirm diagnosis and pre-operatively plan, one must obtain the necessary laboratory investigations and diagnostic imaging [4]. The white blood cell count may be elevated, but it is usually normal in the adult population with SA [1]. This is why inflammatory markers are essential. The C-Reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are usually elevated. After laboratory studies are drawn, an aspiration should be attempted. Computed tomography guided joint aspirations demonstrate an accuracy of close to 90% in the hip joint [5]. The synovial fluid may present as turbid fluid and is commonly associated with leukocyte counts greater than 50,000/mm [1]. Radiographic studies may rule out a differential diagnosis such as trauma and or fracture, arthritic exacerbations, and osteonecrosis. Practitioners may use an ultrasound, which can be useful to visualize a joint effusion. Radiographs will demonstrate a progression of joint space narrowing, and eventual joint destruction [6]. If an ultrasound is not diagnostic, an magnetic resonance imaging (MRI) can further evaluate for a damage within the joint or increased levels of fluid [1]. After clinical exam and diagnostics confirm suspicion, the provider can then discuss treatment options with the patient. Physicians typically have two goals when treating primary SA of the hip: infection control and reconstruction of the joint [7]. The present case report describes a diagnosed septic hip joint with surgical intervention.
A 67-year-old female presented to the emergency department with complaints of left hip pain. Patient has a pertinent past medical history of atrial fibrillation, carcinoid tumor of the stomach, coronary artery disease, diverticulitis, hyperlipidemia, hypertension, mitral valve prolapse, osteoarthritis, osteoporosis, pancreatitis, restless leg syndrome, and hypothyroidism. Patient has a pertinent past surgical history of appendectomy, carpal tunnel release, left total knee arthroplasty, and hysterectomy. The patient was recently discharged from a different hospital 1-month prior after being treated for sepsis and pneumonia. At that time, she still remained bacteremic. She was unable to ambulate upon discharge, so she was sent to a rehab facility. She had been using a wheelchair for assistance. Patient was admitted for pain control, after her presentation to the emergency department. The orthopedic surgery team was consulted to assess her left hip pain. Her prior imaging from 1-month prior was reviewed before her physical examination, which demonstrated a preserved joint space as seen in (Fig. 1-4). 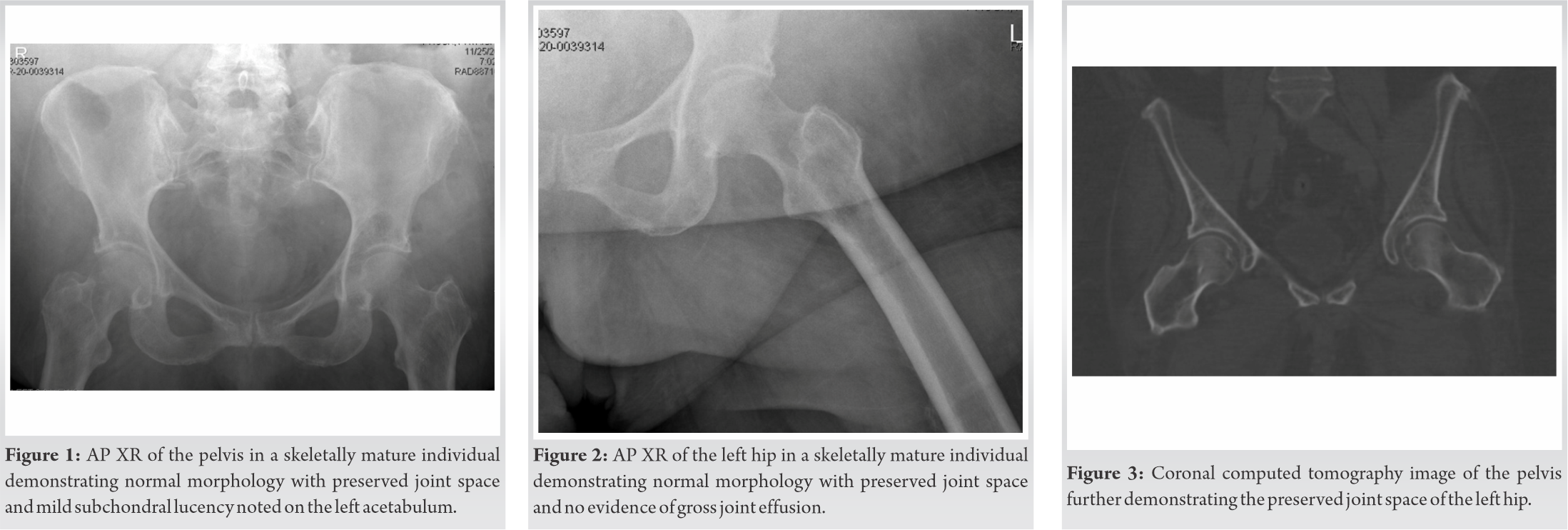

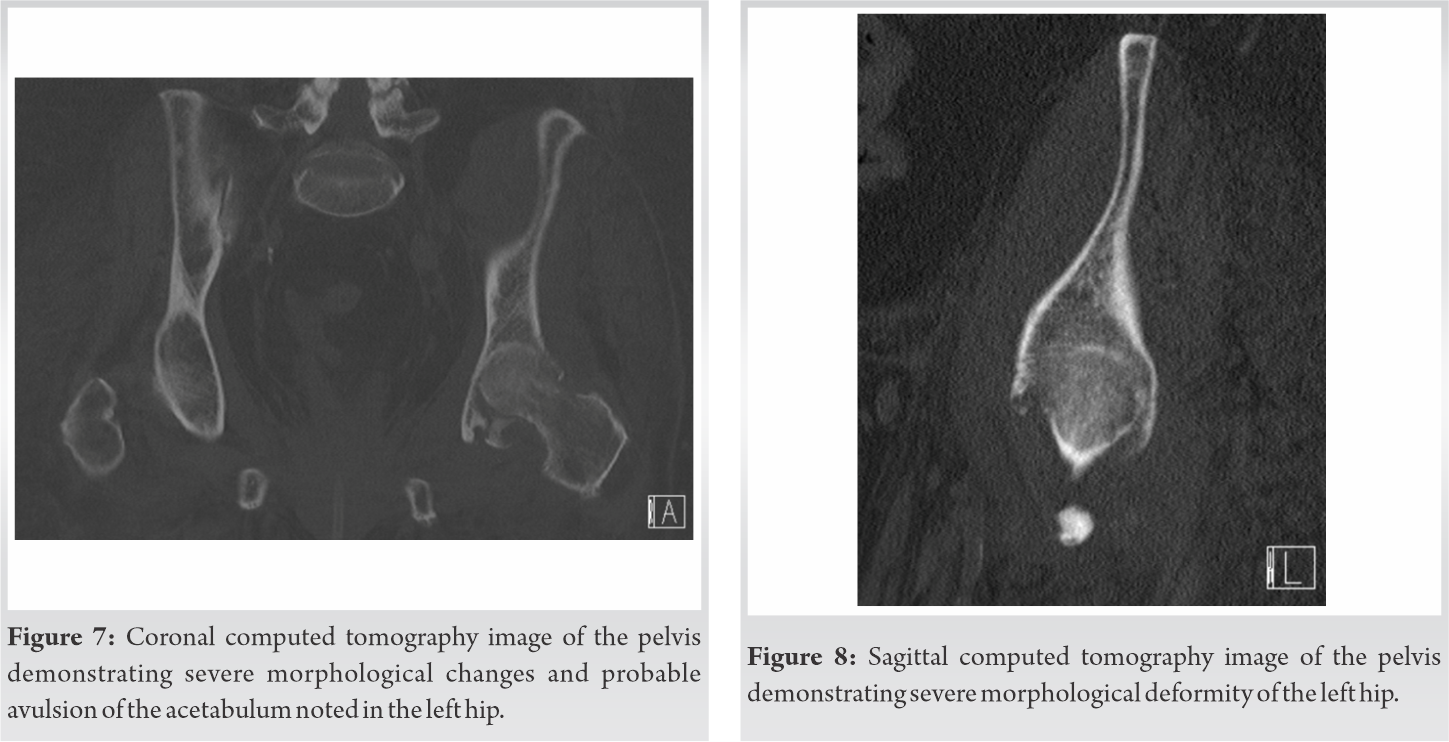
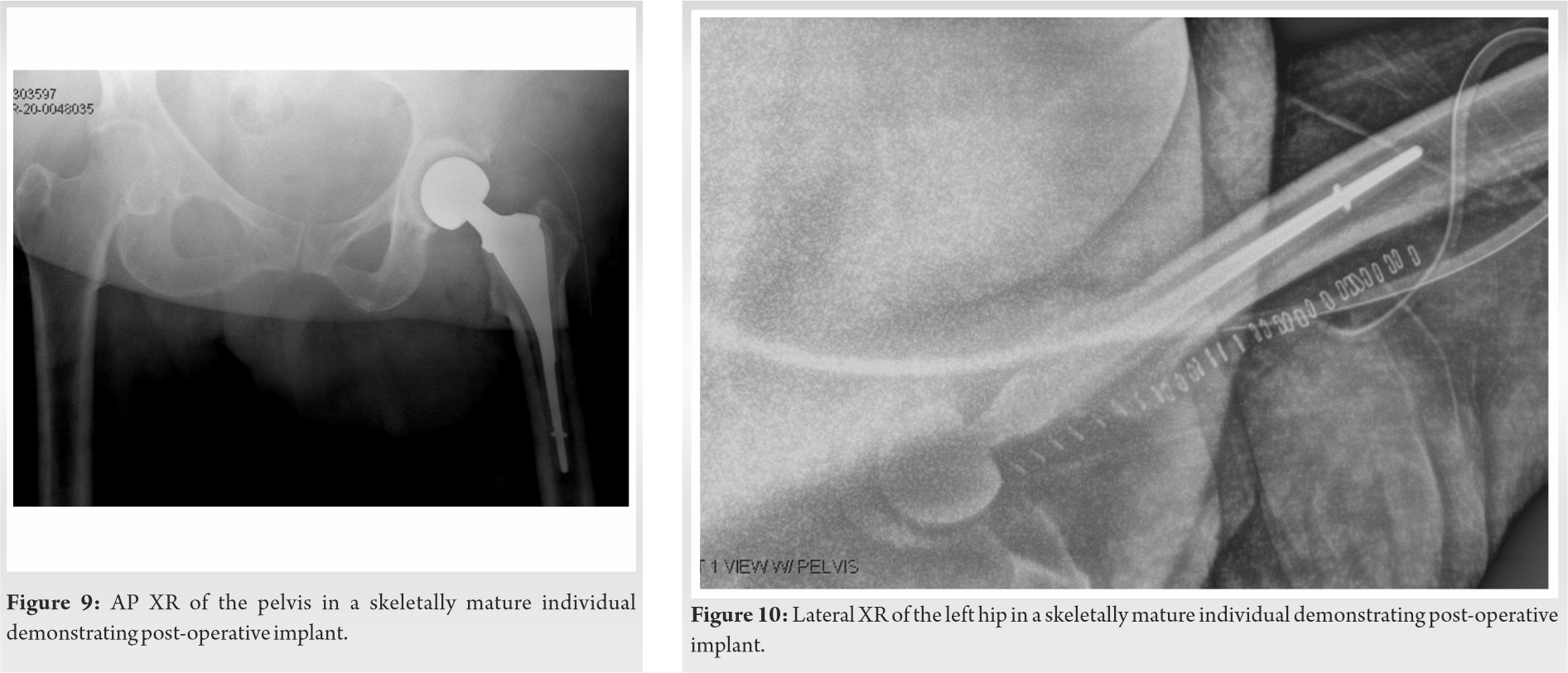
There are many components to appropriate diagnosis of SA, and it is often challenging. Due to the high level of associated morbidity, there is a clear need to rapidly and accurately diagnose SA [3]. Our first step was to obtain imaging of the joint. Since the sensitivity of detecting SA has been reported as 30%, imaging modalities and techniques may not reliably distinguish SA from other inflammatory joint conditions [3]. Even with advanced imaging, it was too difficult to rule out SA, so we proceeded with laboratory findings. The patient had a CRP that was 195.00, and an ESR of 70.0 upon admission. Despite the specificity being low, literature reports that a sensitivity of 83% for CRP >100.00 and a sensitivity up to 97% for ESR >30.0 have been correlated to SA. After the elective procedure, the patient’s inflammatory markers did decrease. Next, we consulted interventional radiology to assist with aspiration of the joint. Cultures of the synovial fluid remain the gold standard for the diagnosis of SA [3]. A synovial fluid aspirate was obtained, which demonstrated a rare Group G beta-hemolytic Streptococcus bacterium within the joint. Intra-operative cultures were taken, and do not demonstrate any isolated bacteria to this day. The ideal treatment choice for an infected hip joint depends on the duration of symptoms. In the instance of early onset, it may be treated arthroscopically or open debridement. In the native hip, arthroscopic irrigation and debridement may comprise a safe and effective treatment option, but only in select patients [8]. In case of prolonged onset, resection hip arthroplasty helps to eradicate the infection [9]. An ideal outcome can be defined when a patient survives and the joint is completely eradicated of infection, all while maintaining the function of the extremity [10]. When assessing outcomes for a one-stage revision, it has been shown to decrease the length of hospital stay, incur a shorter duration of antibiotic treatment, decrease economic costs, lower rate of surgical complications, with higher patient satisfaction and lower mortality rates. The benefit to a two-stage approach that has been shown in literature is a slightly higher success rate in infection control, especially in the case of resistant causative organisms and the presence of a draining sinus [10]. We elected to proceed with the 2-stage approach due to its higher success rates in literature.
Adult septic hip arthritis is a rare diagnosis. So, a proper history, physical examination, infectious laboratory workup is important. The treatment of the condition is based on the duration of symptoms and the physician’s clinical gestalt. Most importantly it is imperative to counsel the patient with the regard to the risk of surgical treatment. More research is needed to definitely determine who may benefit from the different modes of treatment for SA in the adult hip.
Diagnosing a true septic joint, moreover, a native hip can be challenging. Although the diagnose is rare, the potential outcome if missed can be severe. A thorough workup is crucial, to properly evaluate these patients.
References
- 1.Lum ZC, Shieh AK, Meehan JP. Native adult hip with bacterial septic arthritis. JBJS Rev 2018;6:e2. [Google Scholar]
- 2.Kasch R, Assmann G, Merk S, Barz T, Melloh M, Hofer A, et al. Economic analysis of two-stage septic revision after total hip arthroplasty: What are the relevant costs for the hospital’s orthopedic department? BMC Musculoskelet Disord 2016;17:112. [Google Scholar]
- 3.Costales C, Butler-Wu SM. A real pain: Diagnostic quandaries and septic arthritis. J Clin Microbiol 2018;56:e01358-17. [Google Scholar]
- 4.Kumar R, Kumar R, Kumar V, Malhotra R. Comparative analysis of dual-phase 18F-fluoride PET/CT and three phase bone scintigraphy in the evaluation of septic (or painful) hip prostheses: A prospective study. J Orthop Sci 2016;21:205-10. [Google Scholar]
- 5.Isern-Kebschull J, Tomas X, García-Díez AI, Morata L, Ríos J, Soriano A. Accuracy of computed tomography-guided joint aspiration and computed tomography findings for prediction of infected hip prosthesis. J Arthroplasty 2019;34:1776-82. [Google Scholar]
- 6.Ellanti P, Moriarity A, Barry S, McCarthy T. Radiographic progression of septic arthritis of the hip. BMJ Case Rep 2015;2015:bcr2015212079. [Google Scholar]
- 7.Kao FC, Hsu YC, Liu PH, Tu YK, Jou IM, Wane D. High 2-year mortality and recurrent infection rates after surgical treatment for primary septic arthritis of the hip in adult patients: An observational study. Medicine (Baltimore)2019;98:e16765. [Google Scholar]
- 8.de Sa D, Cargnelli S, Catapano M, Peterson D, Simunovic N, Larson CM, et al. Efficacy of hip arthroscopy for the management of septic arthritis: A systematic review. Arthroscopy 2015;31:1358-70. [Google Scholar]
- 9.Anagnostakos K, Duchow L, Koch K. Two-stage protocol and spacer implantation in the treatment of destructive septic arthritis of the hip joint. Arch Orthop Trauma Surg 2016;136:899-906. [Google Scholar]
- 10.Zahar A, Klaber I, Gerken AM, Gehrke T, Gebauer M, Lausmann C, et al. Ten-year results following one-stage septic hip exchange in the management of periprosthetic joint infection. J Arthroplasty 2019;34:1221-6. [Google Scholar]





