Prompt diagnosis of sternoclavicular septic arthritis, early surgical debridement with partial joint resection followed by antibiotic therapy represents an excellent treatment option.
Dr. Sara Monteiro, Department of Orthopedics and Traumatology, Hospital do Divino Espírito Santo, EPER, Ponta Delgada, Portugal. E-mail: sarawmonteiro@gmail.com
Introduction:Sternoclavicular joint (SCJ) infection is rare. Delayed diagnosis might lead to severe complications. Optimal surgical management is still under debate however extended resection of the joint requiring muscle flap coverage appears to be the favored approach nowadays in the cases with bony involvement.
Case Presentation:A 58-year-old man complained of isolated left shoulder and anterior chest pain for over a month. Careful examination revealed a mass over the SCJ. A Computed tomography scan confirmed joint effusion and adjacent bone erosion, with no retrosternal involvement, consistent with SCJ septic arthritis with significant bony involvement.
Conclusion:This case illustrates how a heightened index of suspicion is essential for diagnosis and prompt treatment, and how partial resection was effective and resulted in complete recovery of range of motion and pain resolution, despite bony involvement. There were no signs of recurrence 1 year after surgery.
Keywords: Sternoclavicular joint, septic arthritis, sternoclavicular joint infection.
Sternoclavicular joint (SCJ) infection is rare and accounts for less than 1% of all bone and joint infections [1, 2]. It mainly affects patients with poor general health status or underlying systemic diseases [2]. Bar-Natan et al. [3] found only 27 cases of SCJ septic arthritis documented in previously healthy patients. Common predisposing factors include diabetes mellitus, intravenous drug use, immunosuppression, rheumatoid arthritis, penetrating trauma, and injections [4]. Seeding from systemic bacteremia seems to play a major role amongst the potential mechanisms of SCJ septic arthritis [2].
A prompt diagnosis and treatment are essential to prevent the intra-thoracic spread of the infection [4]. Unlike other septic arthritis, SCJ infection presentation tends to be more indolent [2]. Patients often complain of insidious onset of chest or shoulder pain and fever is not mandatory [2]. Differential diagnosis of tenderness and swelling of the SCJ region includes degenerative osteoarthritis with osteophyte formation (Tietze’s syndrome), rheumatoid arthritis, rheumatic fever, gout, and tumor lesions [5]. Early diagnosis may be challenging [6]. Computed tomography (CT) or magnetic resonance imaging are extremely useful since plain radiograms only show significant findings later in the disease course and have also been used to better assess the extent of the disease and to assist surgical planning [7]. If SCJ infection is suspected, arthrocentesis or biopsy should be obtained. Staphylococcus aureus is the most common isolated microorganism, and its prevalence is increasing. This is also true for methicillin-resistant S. aureus strains (MRSA) [4]. Delayed diagnosis might lead to severe complications including mediastinitis, retrosternal abscess, phlegmon formation in the chest wall, osteomyelitis, and sepsis. Therefore, early recognition followed by immediate treatment is of uttermost importance [7].
Management of SCJ infections is still controversial [7, 8, 9]. Most authors agree that surgery plays a key role in addition to long-term antibiotics in most cases [10]. Conversely, the best surgical procedure remains unclear [4]. The surgical technique can be challenging due to the SCJ thin soft tissue covering and proximity to major vessels [7]. There is a recent tendency to more aggressive initial approaches with en bloc extensive SCJ resections and muscle flaps whenever imaging shows bony involvement [4]. Total clavicle resection has been described as a salvage procedure for cases with multiple failed surgeries [11]. Here, we aim to present a well-documented case of SCJ infection that despite bony involvement was successfully treated with a more conservative surgical procedure with a favorable outcome.
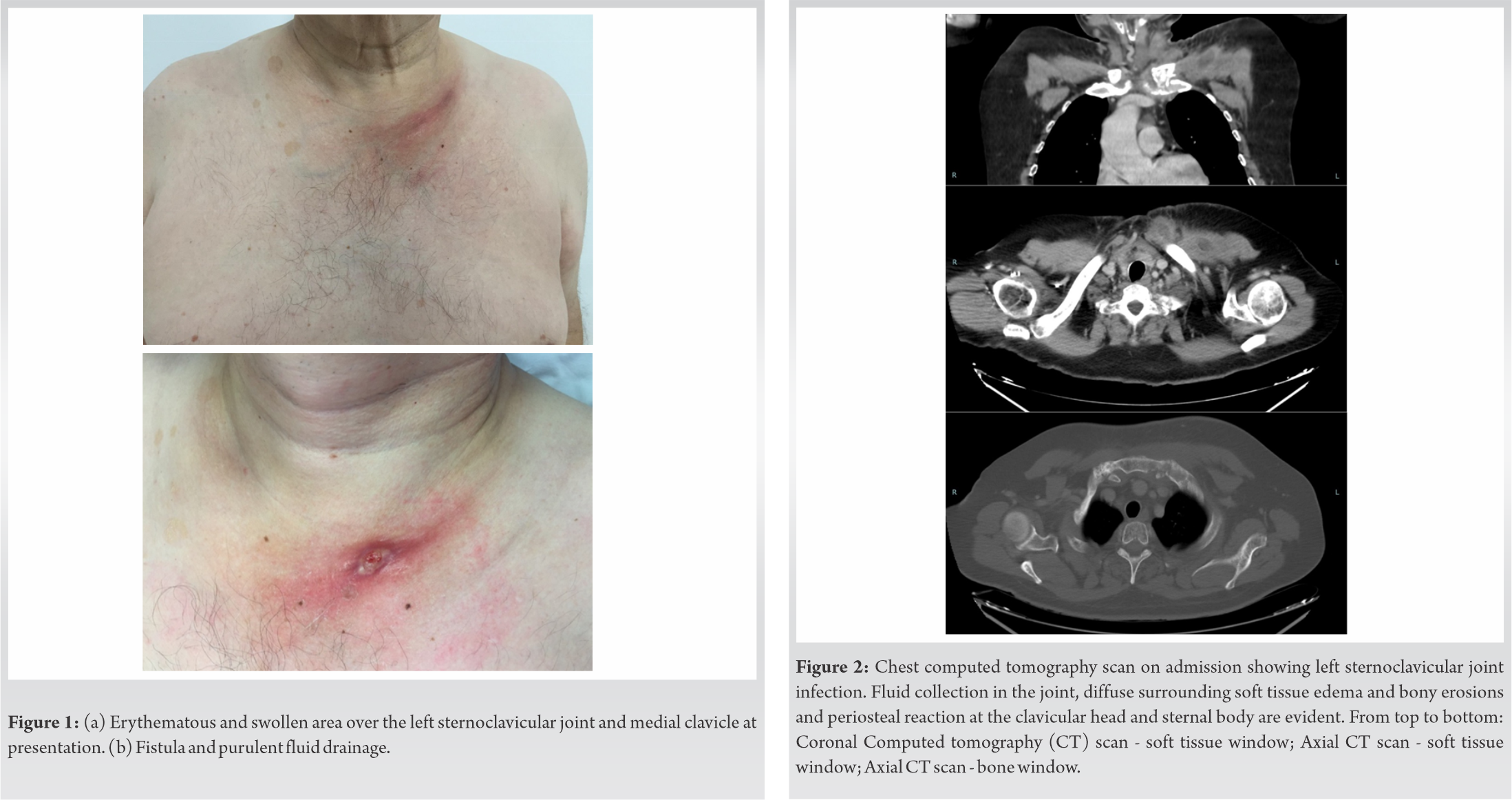
A 58-year-old man presented with a 5-week progressive left shoulder pain and functional impairment. There was no history of trauma, fever, chills, night sweats, malaise, or injections. His medical history only included multiple myeloma, currently in partial remission. A 4-week empiric antibiotic course with oral flucloxacillin and then ciprofloxacin had been previously prescribed with no improvement. Physical examination showed an afebrile, well-nourished man with an erythematous, swollen and tender area over the left SCJ and medial clavicle (Fig. 1a). At the beginning no skin wound or fistulae were present. A fluctuating mass was palpable and left shoulder motion was painful. Despite the full passive range of motion, painful restriction of active movement was present: 120° of forward flexion, 90° of abduction, 20° of external rotation and limited internal rotation to the level of the 5th lumbar vertebra. 2 weeks later, a fistula with a purulent discharge was documented (Fig. 1b).
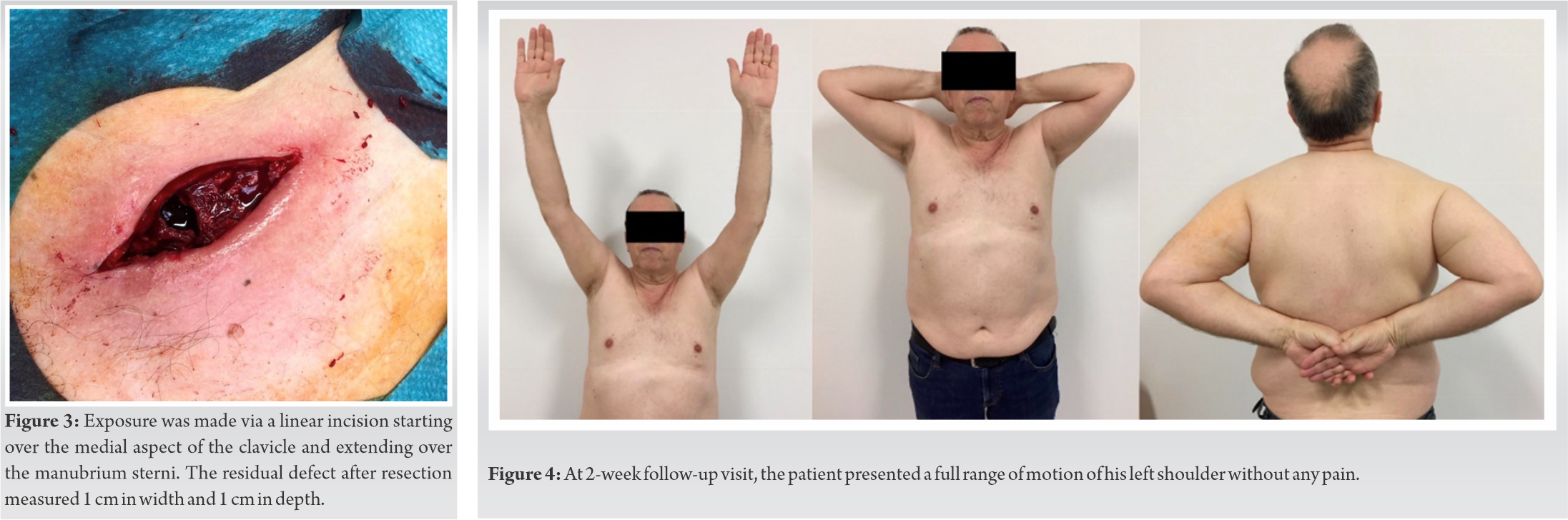
Laboratory findings included increased white blood cell count and erythrocyte sedimentation rate of 78 mm/1st h and C-reactive protein of 18.8 mg/dL. Blood culture was positive for methicillin-susceptible S. aureus. CT scan revealed a fluid collection in the left SCJ and bony erosions and a periosteal reaction of the clavicular head and sternal body (Fig. 2). Retrosternal spread of infection was excluded from the study.
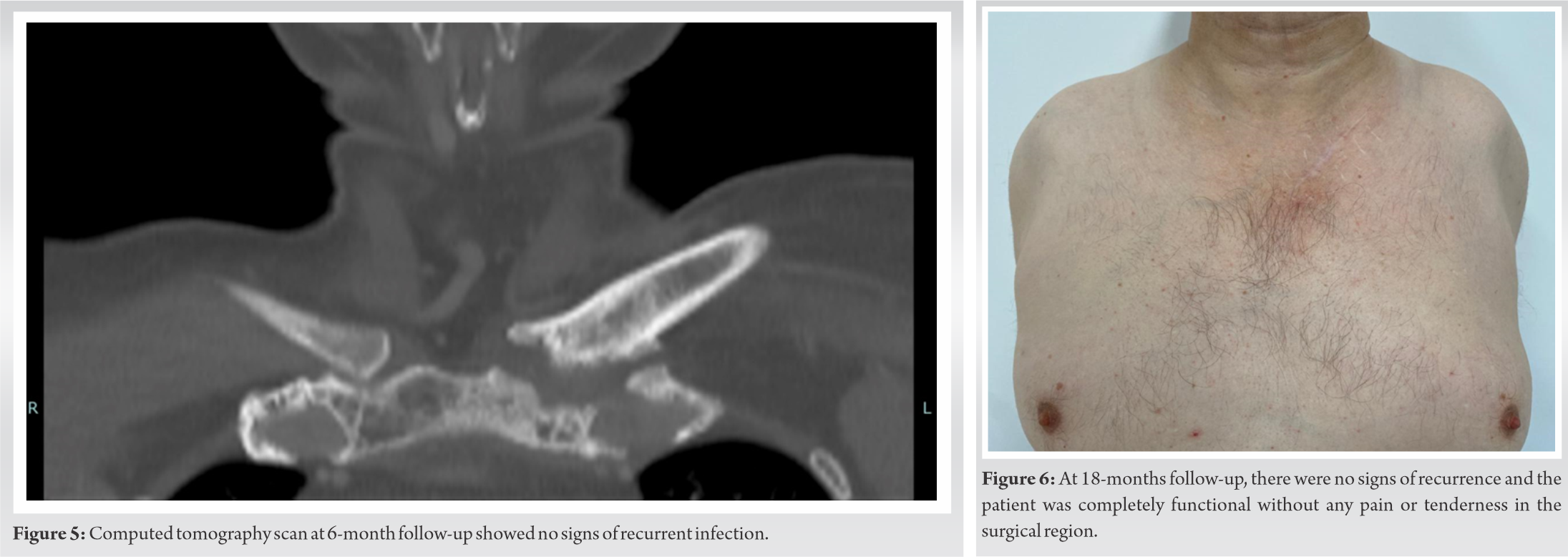
Surgical debridement of the septic left SCJ under general anesthesia was performed. Exposure was made through a linear incision of about 11 cm in length, starting over the medial aspect of the clavicle and extending over the sternal body, over the anterior region of the left SCJ. Fistulectomy, drainage of the abscess and thorough irrigation were undertaken. Resection of the intra-articular disc, debridement of all devitalized tissue and curettage of both the clavicle head and lateral sternal body to healthy bone were performed. At the end of the procedure, the residual bone defect was measured approximately 1 cm in width and 1 cm in depth (Fig. 3). Resected tissue cultures were positive for MRSA. Postoperatively, antibacterial therapy with intravenous linezolid (600 mg every 12 h) was administered for 14 days and was continued orally with levofloxacin (500 mg every 12 h) for 12 weeks, due to linezolid-induced myelosuppression.
The surgical wounds healed completely. 2 weeks postoperatively, the patient was pain-free with full active range of motion of the shoulder (Fig. 4). CT scan performed at 6-month follow-up showed no signs of recurrent infection (Fig. 5). At 18-months follow-up, the patient maintained a full range of motion with symmetrical strength in his left upper limb with no pain or tenderness in the surgical site (Fig. 6).
Sternoclavicular septic arthritis is a rare condition associated with high morbidity thus warranting cautious management [7]. Due to its rarity, current practice is based on small case series and expert opinion [12]. Optimal treatment remains controversial despite some published attempts of management algorithms in which a trend to a more aggressive surgical approach is favored [12]. Our case describes a rare occurrence of SCJ infection with bony involvement that was successfully managed with partial resection of the SCJ – a simpler and safer surgical procedure than the more invasive techniques with radical resections requiring muscle flap for closure.
Although SCJ infection is rare, its incidence is increasing in line with general population ageing and the increased number of immunosuppressed patients [2]. This was the case of our patient whose identifiable predisposing factor for the development of SCJ infection was a multiple myeloma. Several case reports have demonstrated the association between multiple myeloma and the occurrence of septic arthritis [13, 14, 15]. Gram-positive are the most frequent pathogens involved in these patients [15]. Other frequent predisposing conditions such as intravenous drug use, infection at a distant site, diabetes mellitus, trauma, infected central venous access, rheumatoid arthritis, chronic renal failure, alcoholism, HIV infection, and cirrhosis were excluded [2, 4]. Penetrating trauma, injections, and other possible causes of bacteremia were also denied.
SCJ septic arthritis is prone to quickly spread beyond the joint due to the inability of its capsule to distend. Therefore, most cases result in abscess formation [3]. Our patient was no exception.
Guidelines for managing SCJ infections are lacking [7, 9, 10]. Treatment ranges from conservative antibiotic therapy to radical surgery including extended resection of the SCJ requiring muscle flap coverage [7].
It is generally accepted that the great majority of the cases require surgery [16]. Conservative treatment may still be an option in immunocompetent patients with less advanced disease or for those whose surgical procedure must be avoided [5, 16]. Antibiotic therapy alone or in conjunction with isolated aspiration or needle lavage has been suggested but lacks significant literature to prove its reliability [16]. Accordingly, our patient had already been under prolonged oral antibiotics with no improvement.
Murga et al. [7] emphasized the importance of prompt debridement of the joint to early diagnosis from cultures and adequate treatment to prevent a worsening infection. Several surgical approaches have been described. Choosing the appropriate one depends on the extent of the infection to the surrounding bone and soft tissue based on CT/MRI images and also intraoperative findings. Nusselt et al. [4] concluded that if there is no bony involvement, simple incision, debridement and drainage with antibiotic therapy is curative. On the other hand, if osteomyelitis is present, resection of the involved bone is mandatory [4].
The extent of the resection is also subject of debate. Some authors defend primary extended resections to avoid further surgery if the surgical field is not completely debrided [8, 12]. Song et al. [8] reported failure of simple incision, debridement, and antibiotic therapy in five out of six patients. Subsequent surgical resection of their SCJ with advancement flap from the ipsilateral pectoralis major muscle was then performed with good functional results and no complications [8]. In a larger series of 40 patients, Kachala et al. [12] demonstrated excellent outcomes with primary muscle flap closure. A muscle flap is indicated when the residual defect’s size makes it impossible for the wound to close by secondary intention [7]. Therefore, this trendy approach implies a longer and more demanding procedure with significantly higher morbidity.
As in the presented case, simpler procedures with limited resection of all visible infected bone might be curative, thus sparing the patient from more aggressive measures with a longer and more painful postoperative recovery. Besides, further debridement is always an option if the first limited resection fails to control the infection [7].
Carlos et al. [17] described complete healing with no apparent functional limitations in 8 patients with SCJ septic arthritis-half were treated with open drainage and debridement and the other half underwent en bloc resection of the SCJ and the ipsilateral pectoralis major muscle flap. Further studies to help establish which patients will benefit from each approach are needed.
We present an illustrative case of how surgical debridement and partial SCJ resection limited to the infected bone followed by adequate antibiotics represents an excellent option for the treatment of SCJ infection without the morbidity associated to more aggressive resection requiring flap muscle coverage.
SCJ septic arthritis is rare. Prompt diagnosis is a key to early treatment and avoidance of serious complications. Most cases require surgery. The surgical procedure is dictated by the extent of surrounding soft tissue and bone involved. The current trend for SCJ infections with bone involvement is a radical SCJ resection and muscle flap coverage. We present an illustrative case of how surgical debridement and partial SCJ resection limited to the infected bone followed by adequate antibiotics represents an excellent option for the treatment of SCJ infection without the morbidity associated to more aggressive resection requiring flap muscle coverage.
Sternoclavicular septic arthritis is rare but must be considered in the differential diagnosis of painful shoulder or chest. Prompt diagnosis is key to prevent life-threatening complications. Most cases require surgery. The current trend for treatment of sternoclavicular septic arthritis with bone involvement is radical joint resection and muscle flap coverage but simpler procedures might be adequate and avoid the potential iatrogenic risks associated with this technique.
References
- 1.Yood RA, Goldenberg DL. Sternoclavicular joint arthritis. Arthritis Rheum 1980;23:232-9. [Google Scholar]
- 2.Ross JJ, Shamsuddin H. Sternoclavicular septic arthritis: Review of 180 cases. Medicine 2004;83:139-48. [Google Scholar]
- 3.Bar-Natan M, Salai M, Sidi Y, Gur H. Sternoclavicular infectious arthritis in previously healthy adults. Semin Arthritis Rheum 2002;32:189-95. [Google Scholar]
- 4.Nusselt T, Klinger HM, Freche S, Schultz W, Baums MH. Surgical management of sternoclavicular septic arthritis. Arch Orthop Trauma Surg 2011;131:319-23. [Google Scholar]
- 5.Mikroulis DA, Verettas DA, Xarchas KC, Lawal LA, Kazakos KJ, Bougioukas GJ. Sternoclavicular joint septic arthritis and mediastinitis. A case report and review of the literature. Arch Orthop Trauma Surg 2008;128:185-7. [Google Scholar]
- 6.Hiramuro-Shoji F, Wirth MA, Rockwood CA. Atraumatic conditions of the sternoclavicular joint. J Shoulder Elbow Surg 2003;12:79-88. [Google Scholar]
- 7.Murga A, Copeland H, Hargrove R, Wallen JM, Zaheer S. Treatment for sternoclavicular joint infections: A multi-institutional study. J Thorac Dis 2017;9:1503-8. [Google Scholar]
- 8.Song HK, Guy TS, Kaiser LR, Shrager JB. Current presentation and optimal surgical management of sternoclavicular joint infections. Ann Thorac Surg 2002;73:427-31. [Google Scholar]
- 9.Tasnim S, Shirafkan A, Okereke I. Diagnosis and management of sternoclavicular joint infections: A literature review. J Thorac Dis 2020;12:4418-26. [Google Scholar]
- 10.Ali B, Barlas V, Shetty AK, Demas C, Schwartz JD. The preferred treatment of sternoclavicular joint infections: A systematic review. Cureus 2020;12:e9963. [Google Scholar]
- 11.Oheim R, Schulz AP, Schoop R, Grimme CH, Gille J, Gerlach UJ. Medium-term results after total clavicle resection in cases of osteitis: A consecutive case series of five patients. Int Orthop 2012;36:775-81. [Google Scholar]
- 12.Kachala SS, D’Souza DM, Teixeira-Johnson L, Murthy SC, Raja S, Blackstone EH, et al. Surgical management of sternoclavicular joint infections. Ann Thorac Surg 2016;101:2155-60. [Google Scholar]
- 13.Silawy A, Lavie G, Perek S, Zisman D, Weber G, Preis M, et al. Septic arthritis and smoldering myeloma. QJM 2015;108:969-70. [Google Scholar]
- 14.Atiénzar PE, Rico PR, Escandell SB, González CM, Sánchez JM. Osteomielitis esternoclavicular por Klebsiella peumoniae en un paciente cirrótico. Rev Clin Espanola 2012;212:323-4. [Google Scholar]
- 15.Romero Fernández E, Hernández-Maraver D, Canales MÁ, de la Rúa AR. Artritis séptica por Escherichia coli en paciente con mieloma múltiple y dolor en la rodilla izquierda. Reumatol Clin 2011;7:149-50. [Google Scholar]
- 16.Edwin J, Ahmed S, Verma S, Tytherleigh-Strong G, Karuppaiah K. Swellings of the sternoclavicular joint: Review of traumatic and non-traumatic pathologies. EFORT Open Rev 2018;3:471-84. [Google Scholar]
- 17.Carlos GN, Kesler KA, Coleman JJ, Broderick L, Turrentine MW, Brown JW. Aggressive surgical management of sternoclavicular joint infections. J Thorac Cardiovasc Surg 1997;113:242-7. [Google Scholar]