This case report highlights both the clinical and surgical management of hereditary multiple exostoses with concomitant Trevor’s disease.
Dr. John Scott Doyle, Department of Orthopedic Surgery, University of Alabama at Birmingham, ACC Suite 316, Children’s Hospital, 1600 7th Avenue South, Birmingham, Alabama - 35233, United States of America. E-mail: jsdoyle@uabmc.edu
Introduction: Hereditary multiple exostoses (HME) disease is hallmarked by cartilaginous osteochondromas secondary to an autosomal dominant mutation within the exostosin gene family. These outgrowths predominantly occur around the long bone physis. An associated disease is dysplasia epiphysealis hemimelica also known as Trevor’s disease. Trevor’s disease is hallmarked by intra-articular osteochondromas. While the two diseases are similar, they are not genetically related and often have differing patient presentations.
Case Report:We report on a case of a 7-year-old female with a familial history significant for HME that presented with an isolated chief complaint of elbow extension block secondary to osteochondromas found both intra-articular and at the olecranon fossa. We present what could be one of the first cases of coexisting HME and Trevor’s disease of the upper extremity.
Conclusion:Our patient’s unique presentation of an intra-articular osteochondroma speculated to be a result of Trevor’s disease, in the presence of an established HME diagnosis. Management for this patient did not deviate heavily from the established approach for HME which entails conservative observation until symptomatic. Due to the substantial loss of range of motion (ROM), surgical intervention took place in the form of exostoses removal and necessary reconstruction of the fossa. The patient’s ROM subsequently was restored to near normal.
Keywords: Osteochondromas, hereditary multiple exostosis, dysplasia epiphysealis hemimelica, Trevors disease.
Hereditary multiple exostoses (HME) are an autosomal dominant musculoskeletal condition hallmarked by cartilaginous osteochondromas [1]. HME is associated with a loss of function mutation within the exostosin gene family, specifically EXT1 or EXT [2, 3]. Classic clinical presentation of HME includes cartilage capped outgrowths found co-extending along the physis. HME has an incidence of one in 50,000 and 90% of cases are positive for familial history [4]. Long bones are most frequently affected; however, the pelvis, ribs, and vertebrae have also been documented. The distal femur is involved 90% of the time, proximal tibia 84%, proximal fibula 76%, and the proximal humerus 72%, while the distal humerus is only involved in 5% of reported cases [5]. A similar in presentation is dysplasia epiphysealis hemimelica also referred to as Trevor’s disease. Trevor’s disease is histologically similar to HME but the two are not genetically related. At present, there is no known genetic driver for Trevor’s disease [6]. Unlike osteochondromas arising from HME, Trevor’s disease commonly affects the joints of the upper limb and lower limbs [6].
Osteochondromas can manifest skeletal complications such as shortened or bowed limbs, coxa valga, or genu valgum [1, 7, 8]. These osteochondromas lead to secondary symptoms such as nerve compression, radial head dislocation, scoliosis, and pain [6, 9, 10, 11, 12]. HME is conservatively managed until exostoses become symptomatic [13]. Due to the varying location, size, and secondary symptoms of exostoses, surgical options range from simple excision to reconstructive and lengthening procedures [14]. For patients who receive surgical management of exostoses, the average amount of operations the patient will undergo is two [4]. Long-term follow-up of HME patients is indicated for recurrence and potential malignant transformation [15]. Comparatively, the patients with Trevor’s disease will eventually necessitate surgical excision. Surgical excision in Trevor’s disease is associated with better prognosis in comparison to HME as there is less of a chance of recurrence and no cases of malignant transformation have been reported [6].
Chief complaint
A 7-year- and 9-month-old female presented to our clinic as a new patient with an isolated complaint of reduced elbow range of motion (ROM) particularly in extension. She has a known diagnosis HME (Fig. 1).
Physical exam revealed a well appearing child with multiple palpable osteochondromas over various osseous anatomy sites consistent with HME. Concurrent with the patient’s chief complaint, a large osteochondroma in the posterior aspect of the left supracondylar region of the humerus was noted. ROM examination of the left elbow revealed full flexion as well as pronation and supination at the elbow and wrist. In extension however, there was a hard stop at 70°. She exhibits full strength in all upper and lower extremity muscle groups. In addition, the patient had no peripheral neurological deficits or abnormal circulatory findings.
Plain radiographs of the left elbow demonstrated large (3.2 × 1.7 cm), sessile, and exophytic mass over the posterior aspect of the supracondylar humerus extending distally the distal aspect of the capitellum on lateral radiograph (Fig. 2). Distal to this, there were coarse calcifications involving the posterior aspect of the radiocapitellar joint. A normal coronal plane alignment was observed with a Baumann’s angle of 74°. No subluxation of the radiocapitellar or radiohumeral joints was appreciated. Computed tomography scan of the elbow revealed the osteochondroma to be contiguous with the posterior lateral cortex of the humerus and further revealed stippled calcification in the ulnohumeral joint (Fig. 3).
Intra-operative technique
The patient was placed in a lateral position and a pneumatic tourniquet was inflated. A posterior incision curving radially around the olecranon was made and full thickness skin flaps were developed. The ulnar nerve was first localized and protected. The triceps was then elevated both medially and laterally affording excellent visualization of the posterior distal humerus. Adventitial bursa over the osteochondroma was incised and elevated medially and laterally such that base could be visualized grossly. A free intra-articular osteochondroma was then retrieved from the joint along with several other small and calcified fragments. The joint was irrigated copiously then probed to ensure all loose bodies and debris had been evacuated from the joint space.
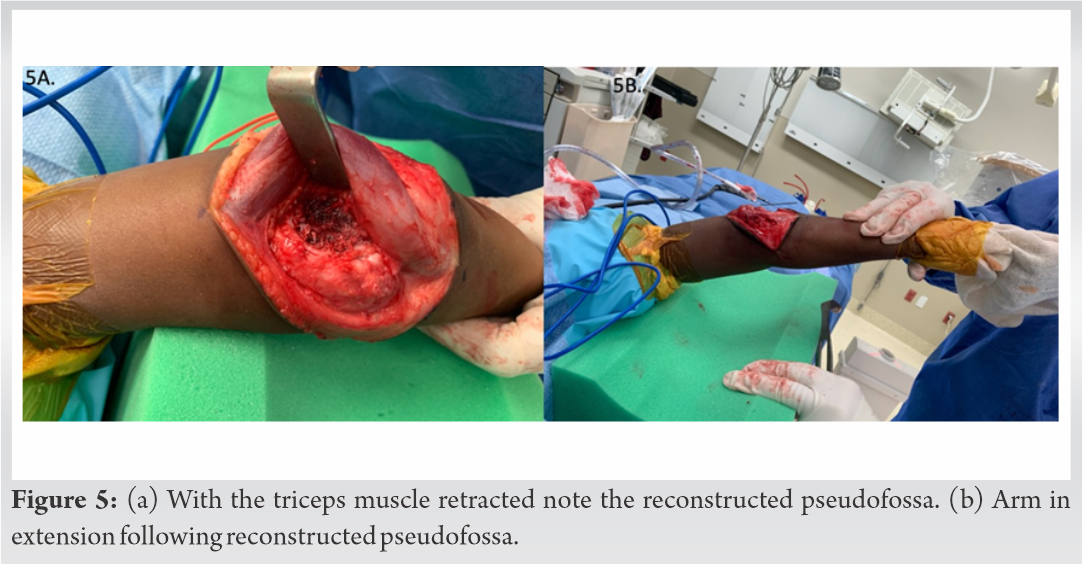
Attention was then focused on the exophytic osteochondroma overlaying the supracondylar region. Utilizing a small osteotome and working from medial to lateral whilst protecting the ulnar nerve, the sessile osteochondroma was separated from the humeral metaphysis to the midline, then the same was carried out from lateral to medial, meeting in the middle and thereby removing the osteochondroma in its entirety, which was sent to pathology for analysis (Fig. 4). A ROM of exam was repeated at this time and it was discovered that the cartilaginous portion of the olecranon was striking the cancellous portion of bone exposed in the posterior distal humerus, precluding extension past about 25°. While flexing the elbow and retracting the triceps, a pneumatic high-speed burr was utilized to recreate the ovoid pseudofossa of distal humerus posteriorly utilizing frequent elbow extension to ensure proper trajectory of burring and taking care not to perforate through bone anteriorly (Fig. 5). When near full extension was achieved, an additional 2 mm of resection was performed in anticipation of some bone re-formation postoperatively.
Surgical summary
The patient underwent an excision of both the osteochondroma of the posterior distal humerus as well as of the loose osteocartilaginous body within the elbow joint and subsequently had osteoplasty of the left distal humerus with reconstruction of the olecranon fossa. Histopathology noted multiple macroscopic nodular pieces of tan bone with cartilage caps. Microscopic analysis noted columns of organized cartilage. Both findings noted to be benign in etiology and consistent with osteochondromas given clinical history.
Post-operative course
Postoperatively, an extension splint was applied but permittance for early ROM with PT. She was seen at 1-week post-operative for wound check at which point there were no immediate complications and she maintained extension to within 5° of full.
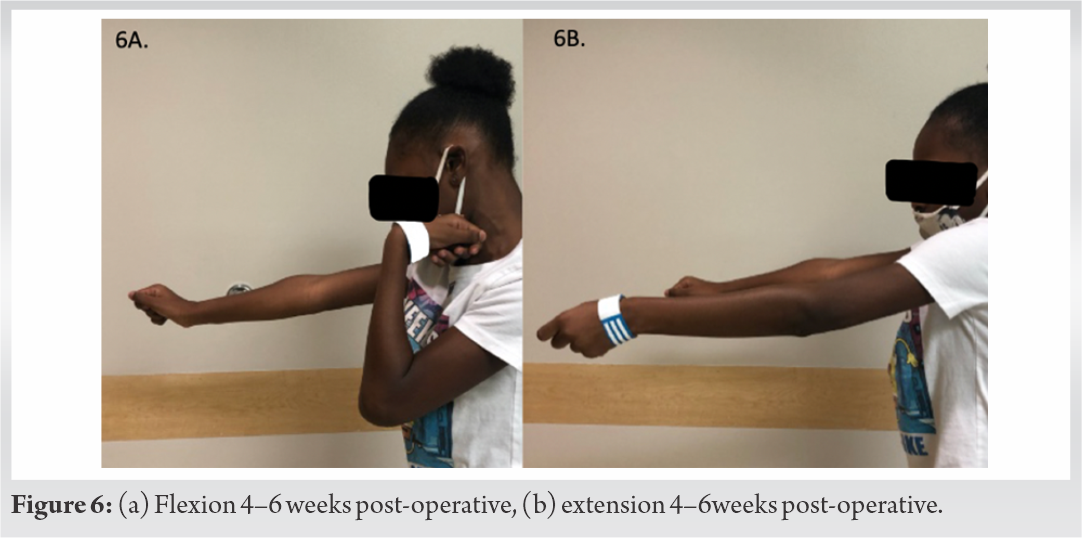
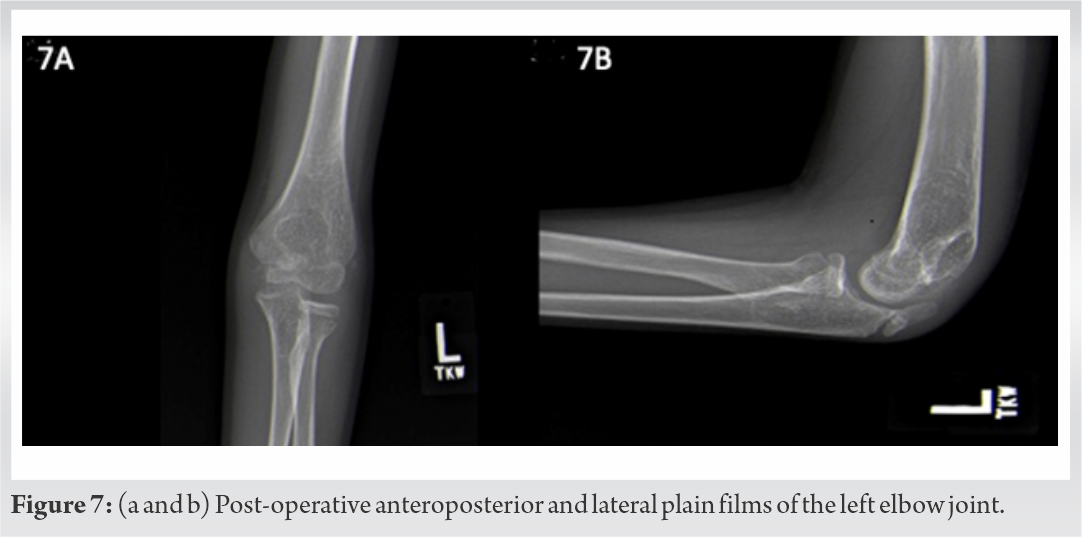
At 4 month’s post-operative, her wounds had completely healed without issue and there had been no fractures. Her elbow ROM was from 10 to 120° with full pronation and supination (Fig. 6). X-rays obtained at that time showed no evidence of lesion recurrence. She was permitted to resume activities ad lib at this visit (Fig. 7).
This report presents what could be one of the first cases of coexisting HME and Trevor’s disease of the upper extremity in a 7-year-old female with a chief complaint of inability to extend the left elbow. Multiple hereditary exostoses are an autosomal dominant disorder which commonly results in multiple asymptomatic osteochondromas arising from the metaphysis of long bones [2, 3]. To the best of our knowledge, intra-articular osteochondromas associated with HME have only previously been reported in the hip and knee [16, 17]. Osteochondromas of the distal humerus are rare in HME given the slow growing nature of the respected physis [18, 19]. Given the extension of the osteochondroma off the lateral column of the distal humeral physis in our patient, we believe that this is consistent with HME though being an unexpected location. However, we report an intra-articular osteochondroma like lesion consistent with Trevor’s disease. Although, it is possible that the intra-articular lesion is a remanent of the olecranon osteochondroma given her genetic history. Unfortunately, the patient was referred to us late and it is not possible to delineate with certainty between the two. Since osteochondromas arising from HME grow juxta-epiphyseal along long bones, it is unusual to find pathology intraarticularly [20]. The treatment of intra-articular osteochondromas has included resection of exostosis through open and arthroscopic approaches [21]. In the presence of intra acetabular exostoses, surgical removal and indicated reconstruction procedures have resulted in restoration of motion and resolution of pain [22, 23].
Our patient has since made a full recovery following excision and osteoplasty of the left elbow and has maintained appropriate ROM. The patient is without recurrence at 4 months postoperatively and has no reported neurovascular deficits. We plan to continue monitoring the patient annually for development of complications.
Our patient’s unique presentation of an intra-articular osteochondroma speculated to be a result of Trevor’s disease, in the presence of an established HME diagnosis. Management for this patient did not deviate heavily from the established approach for HME which entails conservative observation until symptomatic. Due to the substantial loss of ROM, surgical intervention took place in the form of exostoses removal and necessary reconstruction of the fossa. The patient’s ROM subsequently was restored to near normal. With the limited reports of intra-articular osteochondromas being contemporaneous with Trevor’s or sequela with HME, removal of exostosis has benefited the patient’s ROM and function. Limiting this case report is the lack of pre-operative clinical exam photos, this hinders to highlight the gravity of the post-operative results.
Osteochondromas seen in HME disease are seldom seen at slower growing physis such as the distal humerus. Osteochondromas are commonly asymptomatic but in limited cases can limit joint ROM but are not commonly found intra-articular. However, in Trevor’s disease, intra-articular involvement is not uncommon. Both disease processes commonly necessitate surgical evaluation to improve patient’s functional mobility and symptomatology.
References
- 1.Peterson HA. Multiple hereditary osteochondromata. Clin Orthop Relat Res 1989;239:222-30. [Google Scholar]
- 2.Yang C, Zhang R, Lin H, Wang H. Insights into the molecular regulatory network of pathomechanisms in osteochondroma. J Cell Biochem 2019;120:16362-9. [Google Scholar]
- 3.Pacifici M. Hereditary multiple exostoses: New insights into pathogenesis, clinical complications, and potential treatments. Curr Osteoporos Rep 2017;15:142-52. [Google Scholar]
- 4.Schmale GA, Conrad EU 3rd., Raskind WH. The natural history of hereditary multiple exostoses. J Bone Joint Surg Am 1994;76:986-92. [Google Scholar]
- 5.Hennekam RC. Hereditary multiple exostoses. J Med Genet 1991;28:262-6. [Google Scholar]
- 6.Arealis G, Nikolaou VS, Lacon A, Ashwood N, Hayward K, Karagkevrekis C. Trevor’s disease: A literature review regarding classification, treatment, and prognosis apropos of a case. Case Rep Orthop 2014;2014:940360. [Google Scholar]
- 7.Wang YZ, Park KW, Oh CS, Ahn YS, Kang QL, Jung ST, et al. Developmental pattern of the hip in patients with hereditary multiple exostoses. BMC Musculoskelet Disord 2015;16:54. [Google Scholar]
- 8.D’Arienzo A, Andreani L, Sacchetti F, Colangeli S, Capanna R. Hereditary multiple exostoses: Current insights. Orthop Res Rev 2019;11:199-211. [Google Scholar]
- 9.Payne R, Sieg E, Fox E, Harbaugh K, Rizk E. Management of nerve compression in multiple hereditary exostoses: A report of two cases and review of the literature. Childs Nerv Syst 2016;32:2453-8. [Google Scholar]
- 10.Huang P, Zhu L, Ning B. Forearm deformity and radial head dislocation in pediatric patients with hereditary multiple exostoses: A prospective study using proportional ulnar length as a scale to lengthen the shortened ulna. J Bone Joint Surg Am 2020;102:1066-74. [Google Scholar]
- 11.Oestreich AT, Huslig EL. Hereditary multiple exostosis: Another etiology of short leg and scoliosis. J Manipulative Physiol Ther 1985;8:267-9. [Google Scholar]
- 12.D’Ambrosi R, Ragone V, Caldarini C, Serra N, Usuelli FG, Facchini RM. The impact of hereditary multiple exostoses on quality of life, satisfaction, global health status, and pain. Arch Orthop Trauma Surg 2017;137:209-15. [Google Scholar]
- 13.Porter DE, Lonie L, Fraser M, Dobson-Stone C, Porter JR, Monaco AP, et al. Severity of disease and risk of malignant change in hereditary multiple exostoses. A genotype-phenotype study. J Bone Joint Surg Br 2004;86:1041-6. [Google Scholar]
- 14.Song SH, Lee H, Youssef H, Oh SM, Park JH, Song HR. Modified Ilizarov technique for the treatment of forearm deformities in multiple cartilaginous exostoses: Case series and literature review. J Hand Surg Eur Vol 2013;38:288-96. [Google Scholar]
- 15.Florez B, Monckeberg J, Castillo G, Beguiristain J. Solitary osteochondroma long-term follow-up. J Pediatr Orthop B 2008;17:91-4. [Google Scholar]
- 16.El-Fiky TA, Chow W, Li YH, To M. Hereditary multiple exostoses of the hip. J Orthop Surg (Hong Kong) 2009;17:161-5. [Google Scholar]
- 17.Kong M, Cao LI, Zhang Q, Fang Y, Zhao C, Gu H, et al. Identification of a rare case of intra-articular osteochondroma manifesting as three loose bodies in a patient with hereditary multiple osteochondromas: A case report. Oncol Lett 2015;10:798-804. [Google Scholar]
- 18.Pritchett JW. Growth plate activity in the upper extremity. Clin Orthop Relat Res 1991;268:235-42. [Google Scholar]
- 19.Beltrami G, Ristori G, Scoccianti G, Tamburini A, Capanna R. Hereditary multiple exostoses: A review of clinical appearance and metabolic pattern. Clin Cases Miner Bone Metab 2016;13:110-8. [Google Scholar]
- 20.Le Merrer M, Legeai-Mallet L, Jeannin PM, Horsthemke B, Schinzel A, Plauchu H, et al. A gene for hereditary multiple exostoses maps to chromosome 19p. Hum Mol Genet 1994;3:717-22. [Google Scholar]
- 21.Kong M, Cao LI, Zhang Q, Fang Y, Zhao C, Gu H, et al. Identification of a rare case of intra-articular osteochondroma manifesting as three loose bodies in a patient with hereditary multiple osteochondromas: A case report. Oncol Lett 2015;10:798-804. [Google Scholar]
- 22.Ettl V, Siebenlist S, Rolf O, Kirschner S, Raab P. Intra-acetabular localisation of an osteochondroma causing subluxation of the hip joint. Z Orthop Ihre Grenzgeb 2006;144:87-90. [Google Scholar]
- 23.Bonnomet F, Clavert P, Abidine FZ, Gicquel P, Clavert JM, Kempf JF. Hip arthroscopy in hereditary multiple exostoses: A new perspective of treatment. Arthroscopy 2001;17:E40. [Google Scholar]