Careful examination has to be done preoperatively to evaluate the neurology and during surgery extra precautions has to be taken during exploration, as the nerve can get entrapped both on the medial and lateral side.
Dr. Akil Prabhakar, Department of Orthopedics, Seth Gordhandas Sunderdas Medical College and King Edward Memorial Hospital, Mumbai, Maharashtra, India. E-mail: akil.prabhakar@gmail.com
Introduction: Elbow dislocation usually presents with a deformity and swelling, yet it can also present with neurological complication. Nerve injury with dislocation is common in the pediatric age group and is reported infrequently among adults. The most common nerve involved with dislocation is the ulnar nerve followed by the median nerve. The median nerve usually slips medially during dislocation and gets entrapped posterior to the medial epicondyle or it can get entrapped between the fractured medial epicondyle. Here, we describe a unique case of posterolateral elbow dislocation in a 30-year-old female patient with having lateral displacement of the median nerve and the mechanism probably by which the nerve got displaced laterally.
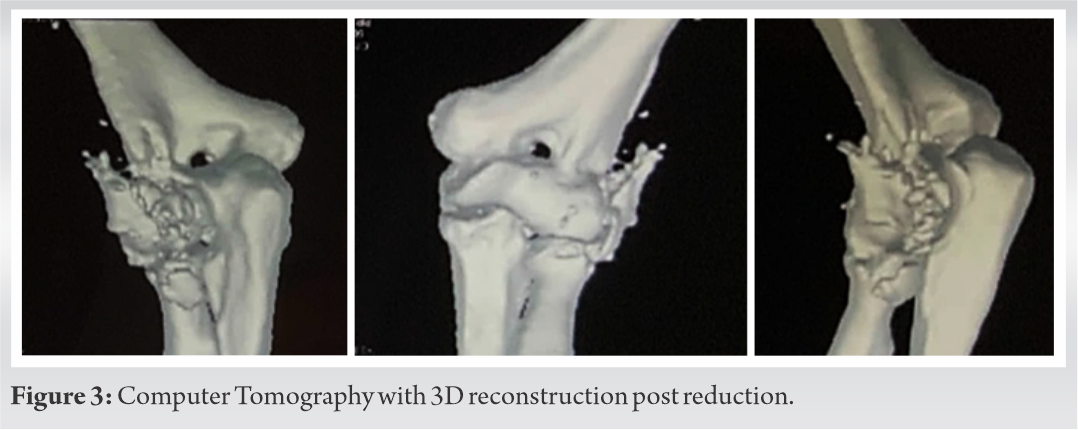
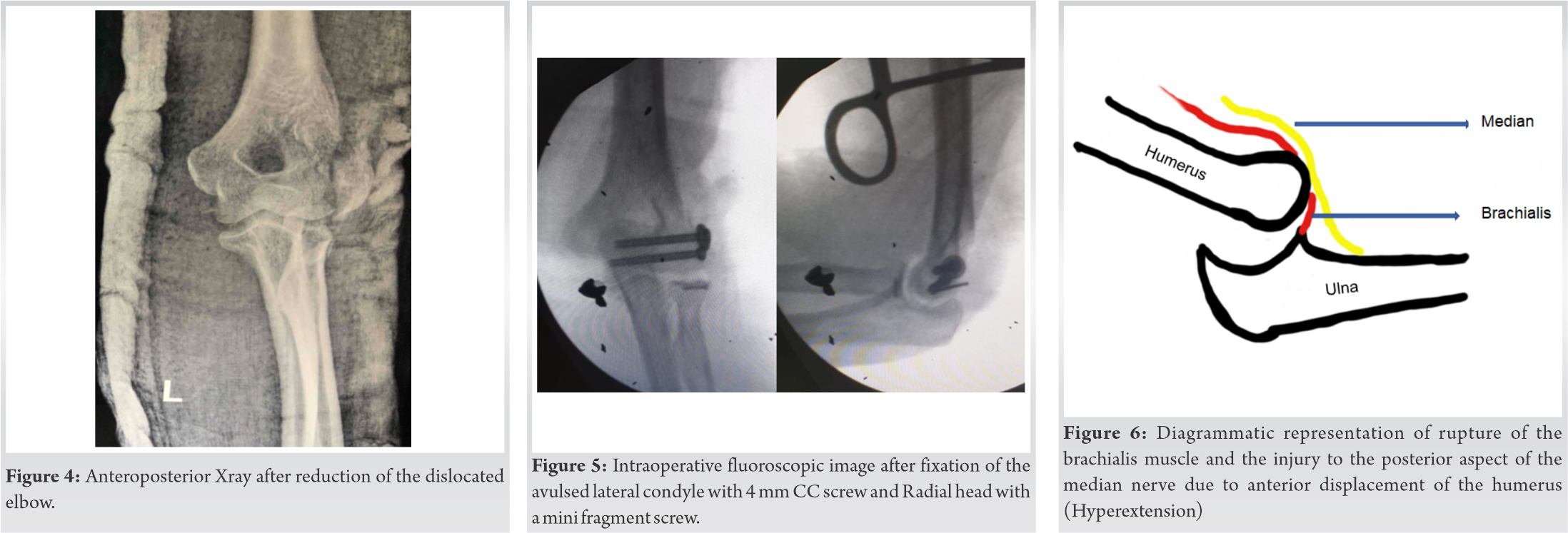
Case Presentation: A 30-years-old female patient of right hand dominant came to us with a left elbow injury after a road traffic accident. Clinical and Radiological examination revealed a posterior-lateral dislocated elbow with a fracture of the radial head and lateral condyle avulsion. Clinically, there was a weakness and sensory hypoesthesia along the median nerve distribution over the left hand and forearm. Initially, closed reduction and splinting done. Later, a planned surgery with a lateral approach avulsed lateral condyle and radial head fixation done with relocation of the median nerve, which was displaced laterally.
Conclusion: There are numerous cases of elbow dislocation with nerve involvement and their complications have been previously described throughout literature. Here, we present a rare case of lateral displacement of the median nerve in a dislocated elbow and the possible mechanism with its management.
Keywords: Median nerve, elbow dislocation, nerve injury.
Nerve injury following dislocation or fracture-dislocation of the elbow is rare [1, 2], it commonly occurs in the pediatric age group, yet it can occur rarely in adults. The most commonly involved is the ulnar nerve followed by the median nerve with an incidence of 3% [3]. Anatomically median nerve lies medial to the brachial artery, deep to bicipital aponeurosis, and anterior to brachialis muscle at the level of the elbow. Hackel et al. [4, 5] showed that the median nerve lies close to the trochlea in extension (4.8 mm in full extension and 8.4 mm in 90° flexion) and it is located above the medial quarter of the trochlea (5.9 mm from the medial border of trochlea). As the median nerve lies medially in the elbow in relation to the distal humerus, it usually displaces medially with dislocation and gets entrapped either behind the medial epicondyle or between the fractured medial epicondyle [3]. O’Driscoll proposed mechanism of Posterolateral Rotatory Instability of elbow involves axial loading with flexion at the elbow. The Ulno-humeral joint undergoes external rotation due to eccentrically loaded triceps, while the humerus (whole-body) rotates internally due to the prominent action of the shoulder adductors and internal rotators. As the mechanical axis falls medially, the elbow joint is forced into the valgus. This valgus force along with external rotation produced at the forearm causes rupture of the elbow joint capsule and ligaments starting with Lateral Ulnar Collateral Ligament and ending with Anterior fibers of Medial Collateral Ligament (AMCL), this mechanism of disruption of ligaments and capsular structure from lateral to medial is coined as Horri`s circle [6, 7]. Schreiber et al. [7] Proposed an alternate theory to Horii circle by analyzing multiple online videos and suggested, that dislocation commonly occurs (Pattern 1–53%) with an axial load in an extended elbow with valgus force and external rotation of the forearm. They found that due to gross valgus deformity, the AMCL is tore more commonly, and this might be even necessary for an elbow to get dislocated in some cases. This is contrary to Horii`s circle in which AMCL is the last structure to be involved. Based on this mechanism of elbow dislocation we have tried to sequence the list of events that could have caused the median nerve to displace laterally in our case.
A 30-year-old Female patient with no comorbidities came to us with a left elbow injury after a road traffic accident. Clinical examination in the emergency room revealed a dislocated elbow with sensory hypoesthesia along the median nerve distribution and pointing index (Fig. 1).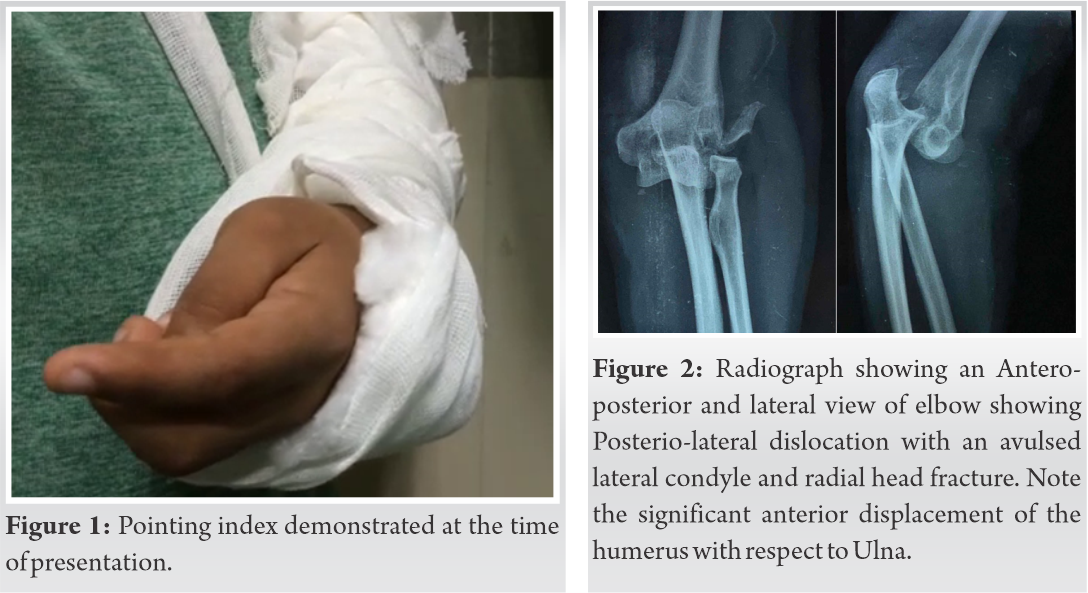
The initial plan was doing an open reduction and internal fixation through a lateral approach and exploration of the median nerve through a separate anterior incision. Under tourniquet through Kocher’s approach, the lateral condyle and radial head fracture fragment was exposed, a thick cord-like structure was found entrapped between the avulsed lateral condyle and distal humerus. Further exploration revealed a torn anterior capsule and torn brachialis muscle. Intra-operative nerve stimulation showed that cord-like structure to be the median nerve. The nerve was edematous and stretched, but there was no visible contusion and the nerve was intact. The nerve was repositioned medially by neurolysis. Post neurolysis the nerve was free of stretching. Fractured fragments were fixed with 4mm Cannulated Cancellous screw and radial head with one mini compression screw. Post fracture fixation, the elbow was stable throughout the range of motion and there was no significant varus or valgus laxity (Fig. 5).
Once pain and swelling subsided patient was started with passive elbow range of movements in a hinged brace, but the weakness of index finger flexion persisted. An improvement in sensory distribution and motor power of Flexor digitorum profundus was noted after 8 weeks and elbow ROM recovered fully. The patient went on to recover with full motor power 12 weeks post-surgery with 2 point discrimination similar to the opposite side.
Nerve injury with elbow dislocation is primarily a problem occurring in children [3, 6, 7, 8, 9] and it occurs rarely in adults. Diagnosis of median nerve palsy in a dislocated elbow is usually delayed in children and they present at a later stage [3]. Matev sign is a radiological sign of entrapment of the median nerve behind the medial epicondyle in a dislocated elbow, where there is cortical depression along with interrupted periosteal reaction [9]. Ultrasound and Magnetic Resonance Imaging (MRI) is a gold standard investigation in the initial evaluation and confirmation of diagnosis. Ultrasound helps in identifying dynamic compression of the nerve, while, MRI is useful in tracing the course of the nerve in an acute entrapment and to see for signs of chronic neuropathy in chronic entrapment [3, 10, 11]. Various mechanism has been reported on how the median nerve is involved with elbow dislocation. Hallet [1] classified median nerve involvement in the pediatric age group into three Types and further two types were added by Al. Quattan [10] and McCarthy et al. [8] (Table 1). All the five types of nerve entrapment reported previously had median nerve displaced towards the medial side with dislocation. Here, we report a unique case, where the median nerve in an adult has been displaced laterally. Beverly et al. reported a case of Anterior Interosseous nerve (AIN) palsy in a 15-year-old pediatric patient post-reduction, in a dislocated elbow which went on to full recovery with conservative management [12]. Our case had median nerve entrapped between the fracture lateral condyle yet there was only palsy of the muscles supplied by AIN. On reviewing the literature of AIN palsy in supracondylar fracture and cadaveric dissection of AIN by Vincelet et al. [13], we found AIN was divided into two zones. Zone 1 was a transitional zone 45 mm from the humeral intercondylar line and ends at a place where it enters the interosseous membrane, 117 mm from the intercondylar line. Zone 2 is from the point where it enters the interosseous membrane to the pronator quadratus muscle, this entire length of Zone 2 is fixed by fibrous bands. Their dissection also revealed AIN fascicles to be located over the posterior aspect of the median nerve. They concluded that AIN palsy in a supracondylar fracture occurs due to direct injury to the posterior aspect of the median nerve by anteriorly displaced proximal fragments and by the stretching of the AIN in zone 2 (as zone 2 is fixed) . Similarly, in our case, a posterolateral dislocation there is hyperextension at the elbow, which translates the humerus anteriorly giving a direct blow to the posterior aspect of the median nerve and significantly stretching the Zone 2 of AIN, leading to its palsy. If nuerodefict in our case was due to nerve entrapment, it would have involved other muscles supplied by the median nerve. AIN palsy in our case should be due to stretching of the zone 2 of AIN because of the direct injury to the posterior fascicles of the median nerve. In our case, the following sequence of events should have occurred which had led to the lateral displacement of the median nerve. The initial Hyperextension during elbow dislocation probably have caused the rupture of a brachialis muscle, a similar case reported by Krych et al. [14], this rupture would have exposed the posterior surface of the median nerve, causing direct injury to the posterior fascicles (fascicles of AIN) and stretching of the zone two fibers leading to AIN palsy (Fig. 6). Subsequent external rotation of the forearm with internal rotation of the whole body along with valgus force at the elbow joint might have caused radial head fracture and avulsion of the lateral condyle. Further internal rotation of the anteriorly displaced humerus along with valgus deformity might have displaced the distal humerus medially and internally rotated, exposing the fractured surface to the median nerve (Fig. 7). This normally would not have occurred if the brachialis muscles were intact. The muscle located posterior to the nerve would have normally protected the nerve from the fracture site and with an intact brachialis, the nerve would have just slipped medially with internal rotation of the humerus causing the usual type of median nerve displacement.
Elbow dislocation can be associated with neurological complications such as nerve entrapment; we present a very rare case of lateral displacement of the median nerve in a posterolaterally dislocated elbow. Careful examination has to be done pre-operatively to evaluate the neurology and during surgery extra precautions have to be taken during exploration, as the nerve can get entrapped both on the medial and lateral side.
Although median nerve commonly displaces medially with the elbow dislocation, lateral displacement can also occur and careful exploration of the fractured fragments in such patients is essential to prevent iatrogenic injury to the nerve. Nerve involvement in elbow dislocation occurs commonly in children’s, but can also occur in adults. Brachialis muscle rupture is an essential event for lateral displacement of the median nerve.
References
- 1.Hallett J. Entrapment of the median nerve after dislocation of the elbow. A case report. J Bone Joint Surg Br 1981;63:408-12. [Google Scholar]
- 2.Paterson T, Ong K, Counsel P, Falconer T. The use of MRI in median nerve entrapment after posterior elbow dislocation and medial epicondyle fracture. J Clin Radiol Case Rep 2019;3:1-4. [Google Scholar]
- 3.Dubey V, Saify A, Samant A, Shahane S. Median nerve entrapment after elbow dislocation and the role of ultrasonography a case report. J Orthop Case Rep 2017;7:4. [Google Scholar]
- 4.Hackl M, Lappen S, Burkhart KJ, Leschinger T, Scaal M, Müller LP, et al. Elbow positioning and joint insufflation substantially influence median and radial nerve locations. Clin Orthop Relat Res 2015;473:3627-34. [Google Scholar]
- 5.Hackl M, Lappen S, Burkhart KJ, Neiss WF, Müller LP, Wegmann K. The course of the median and radial nerve across the elbow: An anatomic study. Arch Orthop Trauma Surg 2015;135:979-83. [Google Scholar]
- 6.Robinson PM, Griffiths E, Watts AC. Simple elbow dislocation. Shoulder Elb 2017;9:195-204. [Google Scholar]
- 7.Schreiber JJ, Warren RF, Hotchkiss RN, Daluiski A. An online video investigation into the mechanism of elbow dislocation. J Hand Surg 2013;38:488-94. [Google Scholar]
- 8.McCarthy CF, Kyriakedes JC, Mistovich RJ. Type-V median nerve entrapment in a pediatric medial condyle fracture: A case report. JBJS Case Connect 2018;8:e108. [Google Scholar]
- 9.Matev I. A radiological sign of entrapment of the median nerve in the elbow joint after posterior dislocation. A report of two cases. J Bone Joint Surg Br 1976;58:353-5. [Google Scholar]
- 10.Ozkoç OG, Akpinar S, Hersekli MA, Ozalay M, Uysal M, Tandoğan NR. Type 4 median nerve entrapment in a child after elbow dislocation. Arch Orthop Trauma Surg 2003;123:555-7. [Google Scholar]
- 11.Akansel G, Dalbayrak S, Yilmaz M, Bekler H, Arslan A. MRI demonstration of intra-articular median nerve entrapment after elbow dislocation. Skeletal Radiol 2003;32:537-41. [Google Scholar]
- 12.Beverly MC, Fearn CB d’A. Anterior interosseous nerve palsy and dislocation of the elbow. Injury 1984;16:125-8. [Google Scholar]
- 13.Vincelet Y, Journeau P, Popkov D, Haumont T, Lascombes P. The anatomical basis for anterior interosseous nerve palsy secondary to supracondylar humerus fractures in children. Orthop Traumatol Surg Res 2013;99:543-7. [Google Scholar]
- 14.Krych AJ, Kohen RB, Rodeo SA, Barnes RP, Warren RF, Hotchkiss RN. Acute brachialis muscle rupture caused by closed elbow dislocation in a professional American football player. J Shoulder Elbow Surg 2012;21:e1-5. [Google Scholar]