Patients should be counseled to avoid deep squatting in a standard posterior stabilized knee as it may cause posterior dislocation of the knee joint.
Dr. Jacob Varughese, Department of Orthopaedics, VPS Lakeshore Hospital, Cochin, Kerala. India. E-mail: varjac@gmail.com
Introduction: We propose a possible mechanism of dislocation in a posterior stabilized (PS) total knee arthroplasty (TKA) and suggest that it can be treated like a stable posteriorly dislocated hip replacement if stable throughout the range on examination under anesthesia.
Case Report:A 71-year-old female presented with the right posterior knee dislocation following 1 year of TKA. Following the successful relocation, the knee was found to be stable throughout the range of movement and an uneventful recovery at 3 years follow-up.
Conclusion: Dislocation can occur in an otherwise stable TKA while squatting and can be successfully treated closed. The patients should be counseled to avoid squatting in a non-high flexion PS knee.
Keywords: Total knee arthroplasty, Dislocation, Instability
Dislocation after total knee arthroplasty (TKA) is uncommon and was first reported in 1979 [1]. The causes include ligament imbalance, neuromuscular dysfunction, implant mal-position, flexion-extension gap mismatch, and polyethylene post breakage. Improved implant designs have reduced the possibility of dislocation post-TKA [2, 3]. Posterior knee dislocation (PKD) is more common than anterior knee dislocation [4, 5].
The patient was informed that data concerning this case would be submitted for publication and they provided consent.
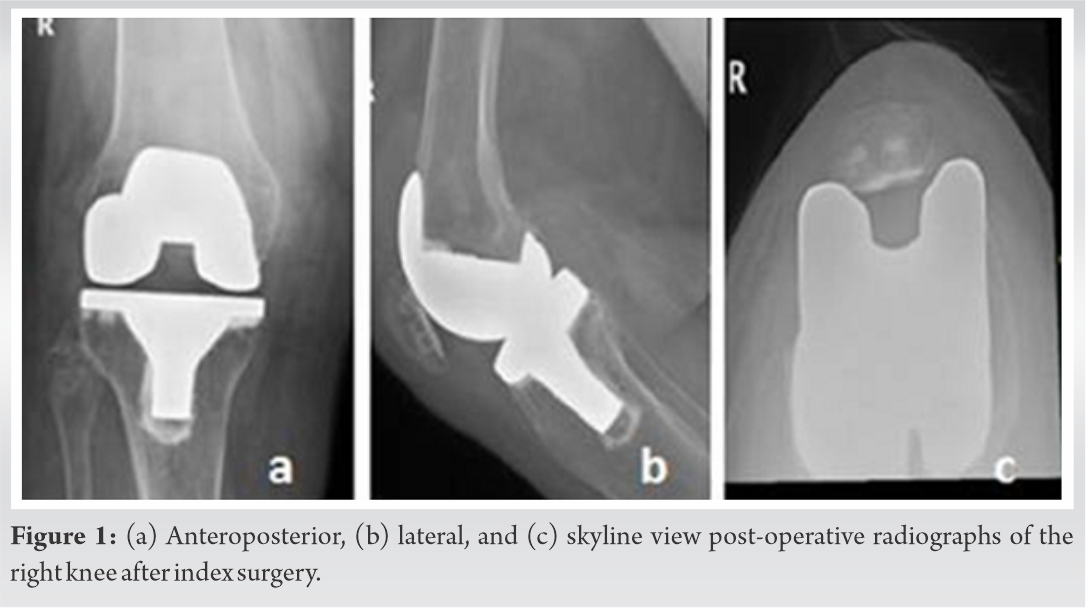
A 71-year-old female patient with the right knee tri compartmental osteoarthritis underwent a right TKA using a posterior stabilized (PS) fixed bearing cobalt chrome implant (PFC Sigma DePuy, Synthes). The surgery was performed through a medial para patellar approach. A combination of measured and gap resection method was used for ligament and flexion/extension balancing. The implant component used was size two femur, size two tibia, 8 mm polyethylene insert and a size 32 patella. The post-operative period was uneventful and post-operative radiographs demonstrated well aligned components (Fig. 1). She was started on a standard TKA rehabilitation protocol with elbow crutch assisted full weight-bearing ambulation from post-operative day 1 for a month. A range of motion (ROM) of 0–125° was achieved by 3 months by which time she was comfortable walking unassisted.
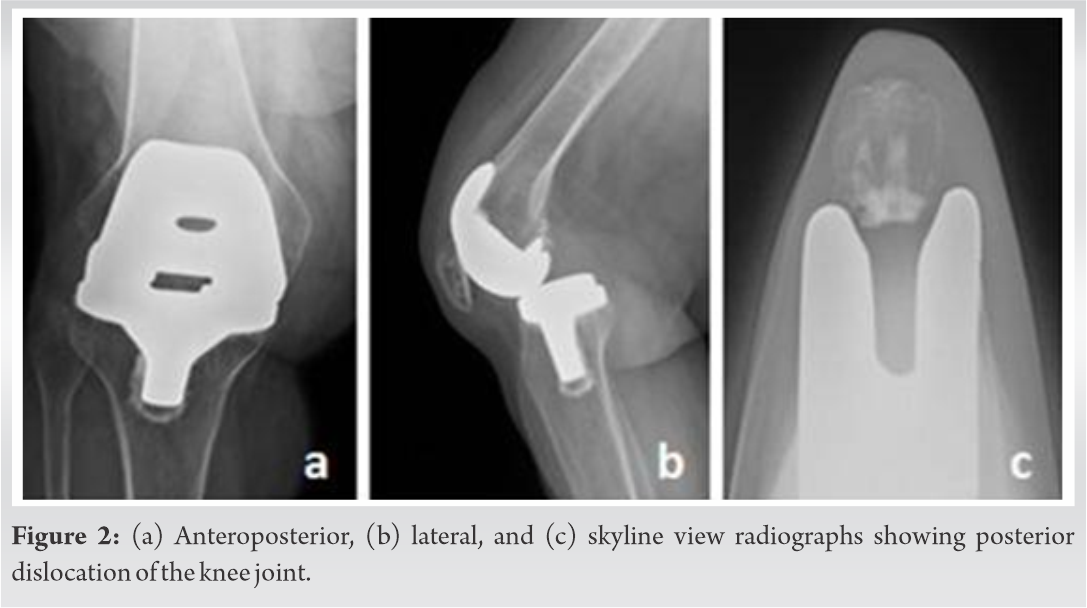
Twelve months after the index surgery, she presented with the operated knee locked in flexion. She described attempting to stand from a squatting position and falling forwards. Examination revealed moderately swollen knee in 60° of fixed flexion with further flexion to 120°. Neurologic examination was found to be normal. Standard radiographs revealed PKD (Fig. 2).
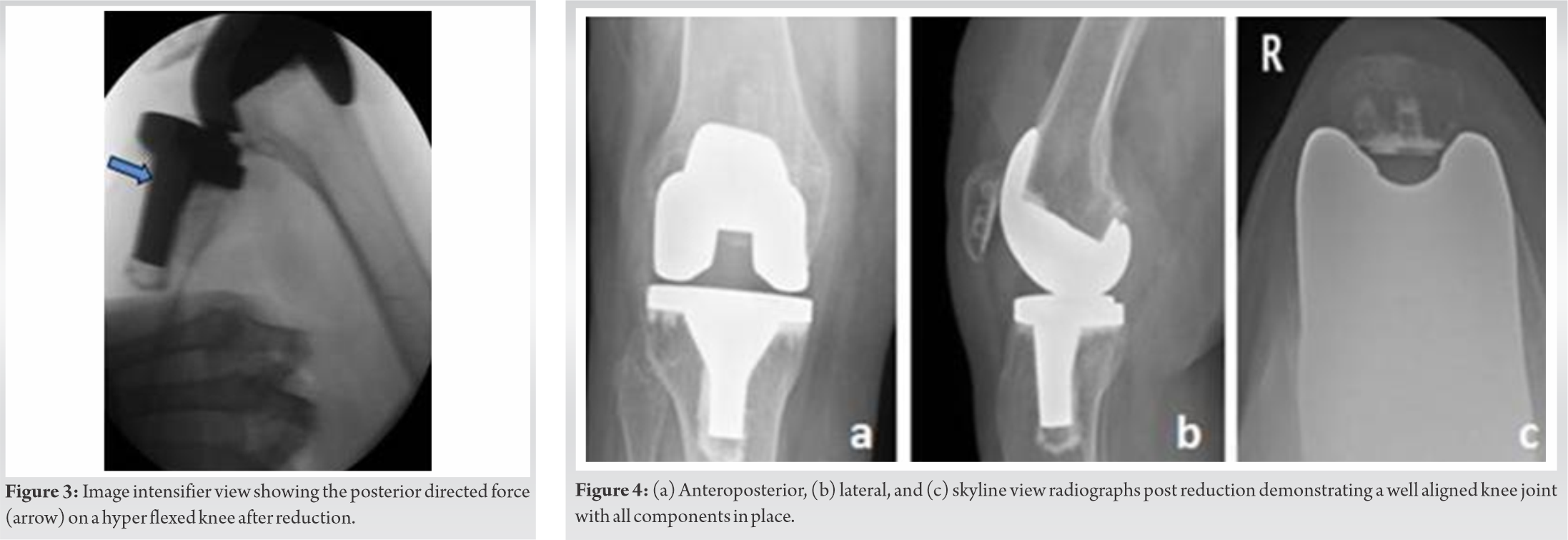
The patient was taken to theatre for an examination under anesthesia with a plan for revision if needed. Under general anesthesia, the knee was flexed to maximum to bring the polyethylene post below and parallel to the inferior aspect of the cam and tibia was pulled anteriorly to reduce the knee. After reduction, we attempted to re-dislocate the knee in full flexion with a posteriorly directed force on the proximal tibia (Fig. 3). We found the joint to be stable through the entire range of movement in both sagittal and coronal plane (Fig. 4) and could not be dislocated even on applying a posterior force in full flexion.
Her range of movement was restored to 0–125° and was mobilized full weight bearing. She had an uneventful recovery at 3 years follow-up.
PS knee implants encompass a femoral cam and a tibial post which allows controlled femoral rollback resulting in improved flexion. However, the flexion range depends on the pre-operative ROM and implant design [6, 7]. Common factors for consideration in a case of knee dislocation post-TKA are tibial component malalignment, polyethylene wear or breakage, flexion-extension gap mismatch, soft-tissue imbalance, and extensor dysfunction [4, 5, 8]. Certain patient-specific factors have also been known to play a role such as obesity and female gender. Most cases result in revision of the implant or insert [5, 9].
Our patient had a well-functioning TKA at 12 months postoperatively and did not have any component malalignment, instability, extensor tendon dysfunction, or a neuromuscular disorder. Insallet al. reported cases of TKA dislocation due to unopposed hamstring pull following extensor malfunction or excess lateral patellar mal tracking [1]. This has been noted in Parkinson’s disease and multiple sclerosis diagnosed patients [9]. In our patient, we presume that the cause was an unopposed hamstring pull with an intact extensor mechanism when falling forwards while getting up from a squatting position. In this scenario, the tibial post is lying inferior and parallel to the cam and a posterior directed force (falling forwards) result in a PKD. This is a potential mechanism of dislocation in a non-high flexion stable PS knee.
We would like to state that a PKD of a PS TKA can occur without component malfunction if posteriorly pulled by the hamstrings in a squatting position and successful treatment can be obtained by closed reduction.
PKD of a PS TKA can occur rarely in a stable well-balanced replaced knee if falling forwards from a squatting position due to an unopposed hamstring pull. Like a stable posteriorly dislocated hip replacement, successful treatment can be obtained by closed reduction alone if stable through entire range under anesthesia. The patients should be counseled not to squat in a standard PS knee not designed for high flexion.
References
- 1.Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg Am 1979;61:173-80. [Google Scholar]
- 2.Lombardi AV Jr., Mallory TH, Vaughn BK, Krugel R, Honkala TK, Sorscher M, et al. Dislocation following primary posterior-stabilized total knee arthroplasty. J Arthroplasty 1993;8:633-9. [Google Scholar]
- 3.Hossain S, Ayeko C, Anwar M, Elsworth CF, McGee H. Dislocation of Insall-Burstein II modified total knee arthroplasty. J Arthroplasty 2001;16:233-5. [Google Scholar]
- 4.Galinat BJ, Vernace JV, Booth RE Jr., Rothman RH. Dislocation of the posterior stabilized total knee arthroplasty: A report of two cases. J Arthroplasty 1988;3:363-7. [Google Scholar]
- 5.Jethanandani RG, Maloney WJ, Huddleston JI 3rd, Goodman SB, Amanatullah DF. Tibiofemoral dislocation after total knee arthroplasty. J Arthroplasty 2016;31:2282-5. [Google Scholar]
- 6.Pandit H, Ward T, Hollinghurst D, Beard DJ, Gill HS, Thomas NP, et al. Influence of surface geometry and the cam-post mechanism on the kinematics of total knee replacement. J Bone Joint Surg Br 2005;87:940-5. [Google Scholar]
- 7.Gandhi R, de Beer J, Leone J, Petruccelli D, Winemaker M, Adili A. Predictive risk factors for stiff knees in total knee arthroplasty. J Arthroplasty 2006;21:46-52. [Google Scholar]
- 8.Lee SC, Am Jung K, Nam CH, Hwang SH, Lee WJ, Park IS. Anterior dislocation after a posterior stabilized total knee arthroplasty. J Arthroplasty 2012;27:324.e17-20. [Google Scholar]
- 9.Rao V, Target JP. Instability after total knee replacement with a mobile-bearing prosthesis in a patient with multiple sclerosis. J Bone Joint Surg Br 2003;85:731-2. [Google Scholar]