Garre’s sclerosing osteomyelitis is a rare clinical entity, confusing in diagnosis, and difficult to treat. It must be considered as differential diagnosis for chronic sclerosing bony lesions in the extremities. The diagnosis requires a thorough workup after excluding more aggressive lesions occurring in childhood and adolescence, which are radiological mimickers. Hence, surgeons should be aware of this condition and vigilant in managing the sclerosing conditions they encounter in their practice.
Dr. Mantu Jain, Department of Orthopedics, All India Institute of Medical Sciences, 102-J Cosmopolis, Dumduma, Bhubaneswar, Odisha - 751019, India. E-mail: montu_jn@yahoo.com
Introduction: Garre’s sclerosing osteomyelitis (GSO) is a rare chronic inflammatory disease resulting in thickening of cortices with loss of medullary canal without any signs of active infection.
Case Report:A 13-year-old boy presented in 2017 with the right thigh pain of 3 years duration, who had exhausted all conservative attempts. We operated the patient with intramedullary reaming with antibiotic-impregnated cement augmented Kuntscher nail, which got jammed. The nail was subsequently removed and left-over cement pieces required an extended trochanteric osteotomy with aggressive curettage. The intra-operative culture was negative at all times, but histopathology suggested chronic inflammation. The patient had complete relief of symptoms at 2 years follow-up with all acute phase reactants reaching baseline and no further periosteal deposition. A follow-up magnetic resonance imaging was not possible due to stainless steel implants in situ.
Conclusion: GSO is a confusing diagnosis that must exclude other mimickers and may recur even after surgical debridement.
Keywords: Sclerosing osteomyelitis, garre’s, non-suppurative osteomyelitis.
Garre’s sclerosing osteomyelitis (GSO) is a rare chronic inflammatory disease that results in the thickening of bony cortices with loss of the medullary canal but lacks any active infection signs [1]. Hence, several eponyms are also known, such as chronic osteomyelitis with proliferative periostitis or chronic sclerosing osteomyelitis or ossifying periostitis [2, 3]. This rare disease affects the male sex, mainly in children and young adults, through cases in older people have also been reported [1, 3]. The mandible is the common site with only a few extremities involvement [3]. GSO is insidious in onset, having variable presentation duration with non-progressive episodic and intermittently recurring pain. However, the patient may not have severe functional loss [4]. The hallmark of the condition is the radiograph appearance of thickening of cortices. Although the blood inflammatory acute phase reactants are raised, intramedullary (IM) culture is usually negative and the biopsy displays a chronic nonspecific inflammation [5]. The recommended treatment is symptomatic with analgesics and broad-spectrum antibiotics, and surgical intervention is reserved for non-responders [6]. However, despite all the measures, the symptoms may reappear again.
This present case highlights such a case of GSO in a 13-year-old child affecting the whole of the right femoral diaphysis who underwent multiple operative interventions.
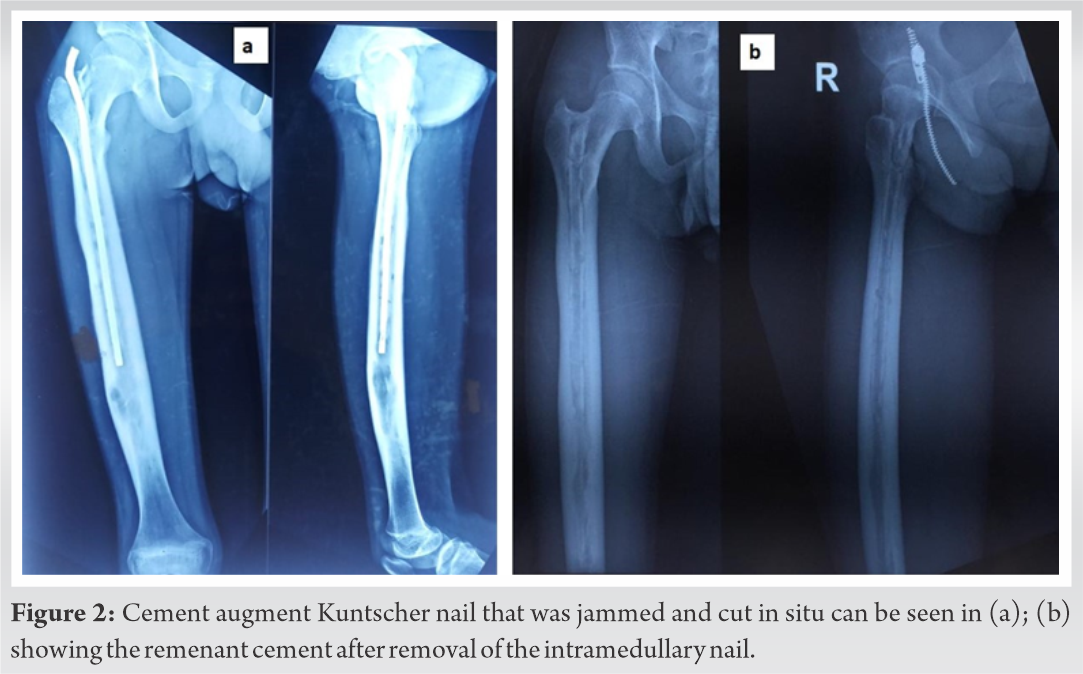
A 13-year-old male presented to the outpatient department with complaints of pain in the right thigh and limp for the past 3 years. He had visited several centers and conservatively management without any success. The patient was afebrile with good general condition on the presentation without any skin changes (redness, edema, or discharging sinus) over the thigh. The radiographs showed a pan-femoral involvement on the right side (Fig. 1a, b) with the widening of the bone (compared to opposite side), thickening of the cortices, and some IM lucent areas. The part was subjected to magnetic resonance imaging (MRI) which displayed T2-weighted hyperintensity extending along the whole length of the femur without any cortical breach (Fig. 1c-e). The patient parents were counseled for the need for surgery. He was planned for intraosseous debridement using serial IM reaming and insertion of an antibiotic-impregnated Kuntscher (K) nail. 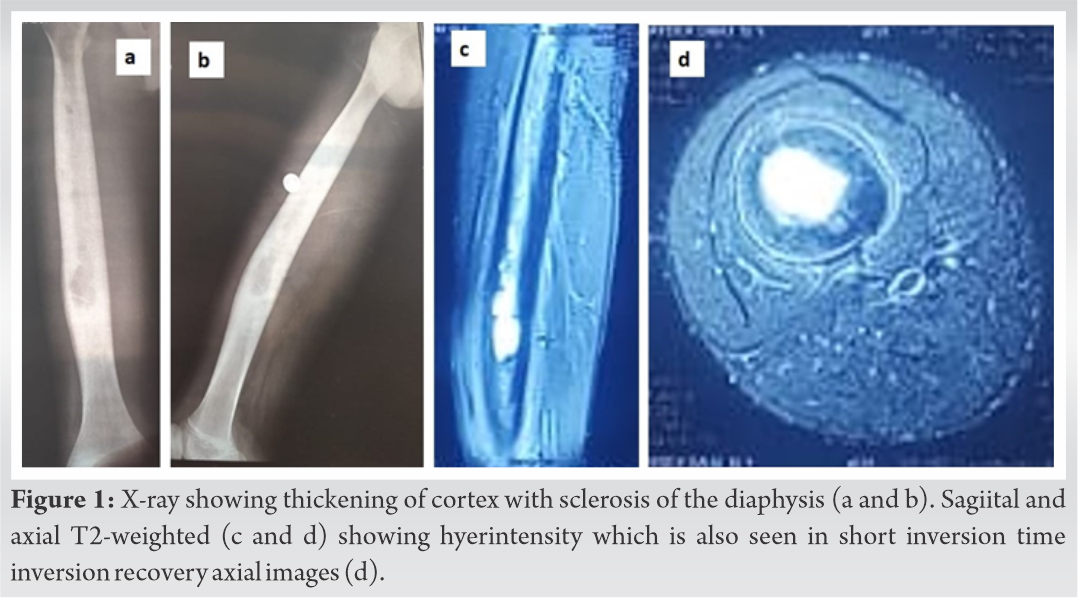
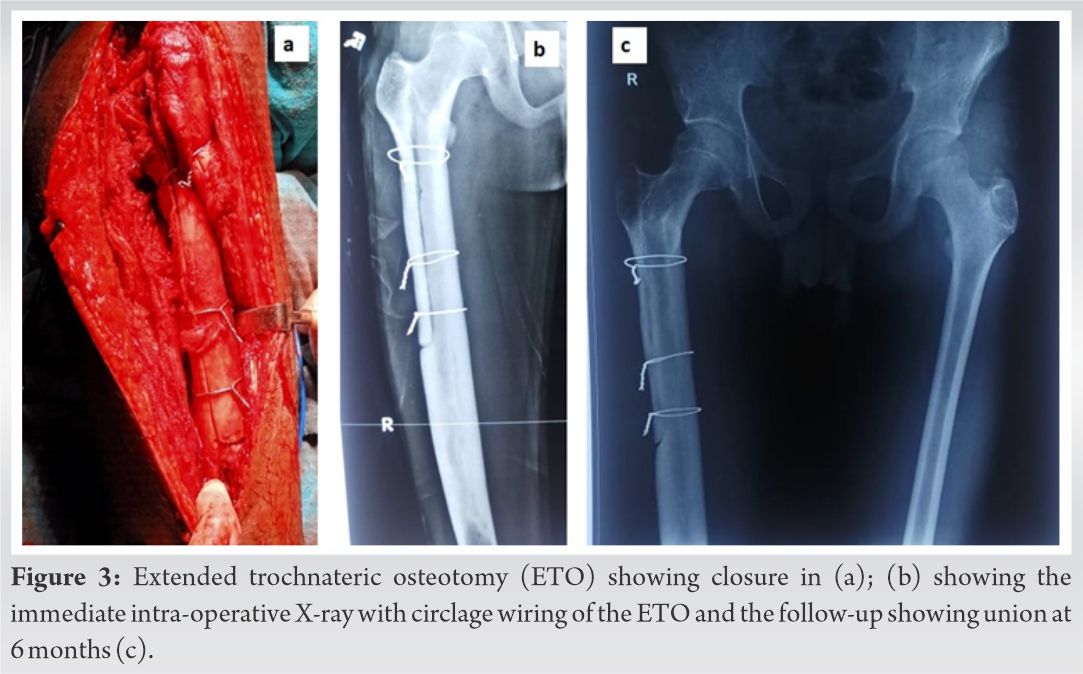
Nevertheless, 2 months after the index surgery, he complained of discharge from the entry site with granulation tissue. The cement-impregnated-antibiotic K-nail was then removed, which had become loose this time. However, at follow-up, some remnants of broken cement particles were seen in the X-ray and the ooze from the wound continued (Fig. 2b). Subsequently, he was taken to the operating theatre for the 3rd time. An extended trochanteric osteotomy was done to remove all the cement pieces, followed by an aggressive curettage of the medullary canal. The osteotomy was closed using three cerclage wires (Fig. 3a, b). His intra-lesional culture was yet again negative. He received the same empirical antibiotics for further 12 weeks with serial monitoring of acute-phase reactants. This time the wound healed and the patient became pain and limp-free.
At 2 years’ follow-up, the patient is entirely pain-free, walking normally, and performing all daily life activities. The blood acute phase reactants were normal levels, and there was no progression of the cortical thickening (Fig. 3c). We could not get a repeat MRI as the stainless steel (SS) wires precluded the MRI and the patient was unwilling to undergo another surgical procedure.
Carl Alois Philipp Garre first described chronic sclerosing osteomyelitis in 1983, which was characterized by thickening of cortices of long bones without suppuration or sequestrum formation [7]. The etiology is generally unclear. Although attributable to low-virulence bacterial infection, the culture is negative most of the time [8]. Again, response to prolong duration antibiotics also supports the infectious theory [2]. The commonly affected bone is the mandible and only a few sporadic cases involving the long bones such as tibia, femur, humerus, metacarpal, metatarsal, and rib have been reported [6, 9, 10, 11, 12, 13]. There are no specified diagnostic criteria to stamp this condition and tissue biopsy of chronic inflammation in the presence of a prolonged disease course is usually confirmatory [14]. The characteristic X-ray findings are periosteal thickening but not specific to GSO. Recently, with the advent of MRI, De Moraes et al. reported a T2-hyperintensity while Vannet et al. reported a heterogeneous low signal intensity in their case [3, 11]. We also similarly found pan-femoral T2-hyperintensity and thought to be an abscess but failed to see pus intraoperatively. An isotope can show an increase in uptake bone scan, which is not specific [11].
An aggressive workup is mandatory to rule out other tumorous conditions with similar radiological pictures of periosteal thickenings, such as osteoid osteoma, eosinophilic granuloma, or Ewings sarcoma. Non-tumorous mimickers could be pustulosis palmoplantar, SAPHO syndrome, ulcerative colitis, and Ribling’s disease. In older people, Paget’s disease is also a possibility [1, 3, 15]. While CT scan can be helpful in osteoid osteoma, others may need histopathological confirmation.
The most appropriate treatment is still unclear. Few patients respond to non-steroidal anti-inflammatory drugs, analgesics, and intermittent antibiotics; few require surgical intervention. Interestingly, Hallmer et al. reported successful management of two cases of GSO of the jaw with Denusumab and Taylor treated a patient using the bisphosphonates [16, 17]. The surgical approach is fenestration and curettage if the disease is localized [6]. Some authors have reported bone resection followed by bone transport using a circular external fixator [14]. For diffuse involvement, such as in our case, IM reaming is an option. Collert et al. reported eight cases with favorable outcomes with IM reaming [4]. IM reaming can be difficult, as we found in our case. Vannet et al. used a combination of hand and power reamers to open the canal but had re-sclerosing of the IM canal, so the authors had to IM nail on a second attempt [11]. We also planned the same, but the K-nail got jammed.
A repeat MRI in follow-up could be exciting, but we could not get it done due to the SS wires. We believe that altered intensity could alert and predict recurrence in diffuse cases as experienced by Vannet et al. [11].
GSO is a rare clinical entity, confusing in diagnosis, and difficult to treat. The diagnosis requires a thorough workup after excluding more aggressive lesions, which are radiological mimickers. There is a possibility of recurrence. Hence, surgeons should be aware of this condition and vigilant in managing the sclerosing conditions they encounter in their practice.
GSO must be considered a differential diagnosis for chronic sclerosing bony lesions primarily occurring in childhood and adolescence. Even though they are benign, they are difficult to diagnose and treat because of their rarity outside the jaw.
References
- 1.Song S, Jeong HJ, Shin HK, Kim E, Park SJ, Park JH. Sclerosing osteomyelitis of Garré: A confusing clinical diagnosis. J Orthop Surg 2019;27:1-4. [Google Scholar]
- 2.Vienne P, Exner G. Osteomyelitis sclerosans Garré [Garré sclerosing osteomyelitis]. Orthopade 1997;26:902-7. [Google Scholar]
- 3.de Moraes FB, MoBarratta TM, Severin AA, de Alencar Faria D, de Oliveira César F, de Souza Carneiro S. Garré’s sclerosing osteomyelitis: Case report. Rev Bras Ortop 2014;49:401-4. [Google Scholar]
- 4.Collert S, Isacson J. Chronic sclerosing osteomyelitis (Garre). Clin Orthop Relat Res 1982;164:136-40. [Google Scholar]
- 5.Macnicol M, Watts A. Haematogenous osteomyelitis. Surg 2005;23:25-30. [Google Scholar]
- 6.Sharma H, Taylor GR. Chronic sclerosing osteomyelitis of Garré affecting fifth metatarsal bone of the foot. Foot 2003;13:209-11. [Google Scholar]
- 7.Wood RE, Nortj’e CJ, Grotepass F, Schmidt S, Harris AM. Periostitis ossificans versus Garre's osteomyelitis. Part I. What did Garre really say? Oral Surg Oral Med Oral Pathol 1988;65:773-7. [Google Scholar]
- 8.Vienne P, Exner GU. Osteomyelitis sclerosans Garr’e. Orthopade 1997;26:902-7. [Google Scholar]
- 9.Kelkar AS, Malshikare VA. Chronic sclerosing osteomyelitis of a metacarpal. J Hand Surg Br 2005;3:298-301. [Google Scholar]
- 10.Kadish LJ, Muller CJ, Mezger H. Chronic sclerosing osteomyelitis in a long bone caused by actinomycosis. A case report. S Afr Med J 1982;62:658-9. [Google Scholar]
- 11.Vannet N, Williams H, Healy B, Morgan-Jones R. Sclerosing osteomyelitis of Garré: Management of femoral pain by intramedullary nailing. BMJ Case Rep 2014;2014:bcr2014206533. [Google Scholar]
- 12.Schwartz AJ, Jones NF, Seeger LL, Nelson SD, Eckardt JJ. Chronic sclerosing osteomyelitis treated with wide resection and vascularized fibular autograft: A case report. Am J Orthop (Belle Mead NJ) 2010;39:E28-32. [Google Scholar]
- 13.Bai S, Zhang H, Li Z, Li D, Li H. A 53-year-old man with a sclerosing rib lesion: A case report. Medicine (Baltimore) 2017;96:e8692. [Google Scholar]
- 14.Schultz C, Holterhus PM, Seidel A, Jonas S, Barthel M, Kruse K, et al. Chronic recurrent multifocal osteomyelitis in children. Pediatr Infect Dis J 1999;18:1008-13. [Google Scholar]
- 15.Mukkada PJ, Franklin T, Rajeswaran R, Joseph S. Ribbing disease. Indian J Radiol Imaging 2010;20:47-9. [Google Scholar]
- 16.Hallmer F, Korduner M, Møystad A, Bjørnland T. Treatment of diffuse sclerosing Osteomyelitis of the jaw with denosumab shows remarkable results-a report of two cases. Clin Case Rep 2018;6:2434-7. [Google Scholar]
- 17.Taylor H, Patel V, Matharu J, Kwok J. The treatment of diffuse sclerosing osteomyelitis with oral bisphosphonates. Oral Surg 2018;11:69-78. [Google Scholar]