Hibernoma should be considered as one of the differential diagnosis while working up on soft tissue tumor.
Dr. Devanshu Gupta, Department of Orthopaedic Surgery, Grant Government Medical College and Sir J J Group of Hospital, Byculla, Mumbai - 400 008, Maharashtra. India. E-mail: devmittal2293@gmail.com
Introduction: Hibernomas are uncommon benign proliferations arising from the adipocytes of brown fat usually occurring over back, neck, shoulder, and thighs. It is an underreported entity often misdiagnosed as a lipoma.
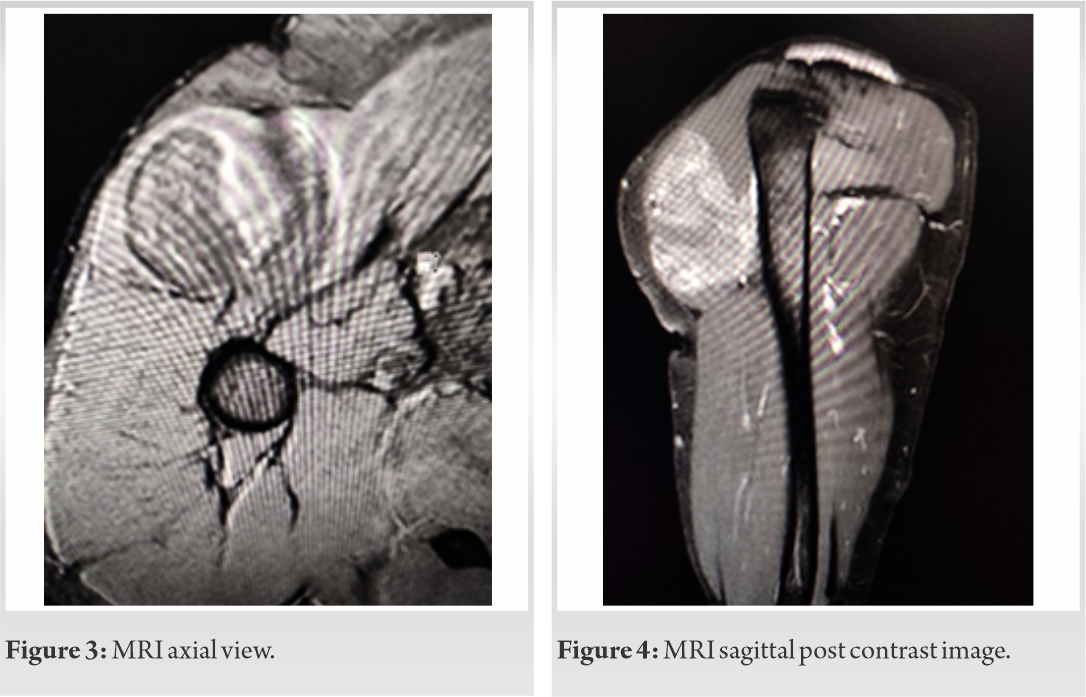
Case Report:We report a case of an otherwise healthy thirty-four-year-old male who presented with a painless swelling, with no preceding trauma, involving the right shoulder joint of three months duration. MRI revealed it to be a fatty intense lesion arising within the anterior fibers of the right deltoid. The tumor was removed en-masse with wide local excision through the deltopectoral route. The histopathology of the resected tumor was consistent with the diagnosis of hibernoma. The patient recovered the previously hindered movements at the shoulder joint 2 weeks post-operatively.
Conclusion: Hibernoma should be considered as a differential diagnosis for soft tissue tumors occurring in the above-mentioned sites. It can be completely resected surgically and no recurrences post-excision have been reported till date.
Keywords: Hibernoma, shoulder girdle, brown fat, MRI.
Hibernomas are uncommon, benign soft tissue tumors of brown fat origin [1]. Hibernoma arises from vestigial remnants of fetal brown adipose cells and usually manifests as a slow growing, painless, and soft-tissue mass. It is seen mainly in adults, with slight female preponderance. It is commonly seen in the subcutaneous region of the back, especially the periscapular and interscapular area, neck, axilla, shoulder, thorax, thighs, and retroperitoneum [2]. It accounts for 1.1% of all adipocytic tumors and is commonly mistaken for lipoma or liposarcoma. Around 10% of cases are intramuscular [3]. It has been described in less than 200 case reports or case series [4].
A 34-year-old male presented to us with a painless swelling in the right shoulder region for 3 months. The swelling was insidious in onset, gradually progressive associated with restriction of shoulder movement. There was no history of any other swelling in the body, any trauma or any chronic medical illness, or any prior surgery. 

Hibernoma is a rare, benign soft tissue tumor originating from brown fat. It is a slow‑growing, painless tumor that accounts for 1.6% of benign lipomatous tumors and 1.1% of all adipocytic tumors [4]. In 1906, Merkel was the first to describe this tumor as “pseudolipoma” [5]. Grey coined the term “hibernoma” because it resembled the brown fat of the hibernating animal [4] Due to the hypervascularity, hibernomas may sometimes appear with locally increased skin temperature. They can reach a size of up to 20 cm so that symptoms secondary to compression of adjacent structures may be developed. The most common site of hibernoma is the thigh, which usually occurs in the periscapular and interscapular region, neck, shoulder, and less frequently in trunk, retroperitoneum, upper and lower extremities. Rare locations such as intraosseous, paraaortal, and intracranial regions have also been reported. Multiple lesions in a single patient are possible [5]. The etiology of hibernomas is unknown. Molecular genetics show deletions respectively reciprocal translocation of chromosome 11 which encodes the tumor suppressor gene MEN 1 [6]. Its occurrence in the third to fourth decade of life contrasts with other fatty tissue tumors such as liposarcomas that occur in the fourth to seventh decade [4]. Hibernomas are well-circumscribed masses on CT, appearing mildly hyperdense to subcutaneous fat, with attenuation ranging between skeletal muscle and fat. Hypothesized to be due to active thermogenesis, hibernomas are also noted to be FDG-avid on positron emission tomography.
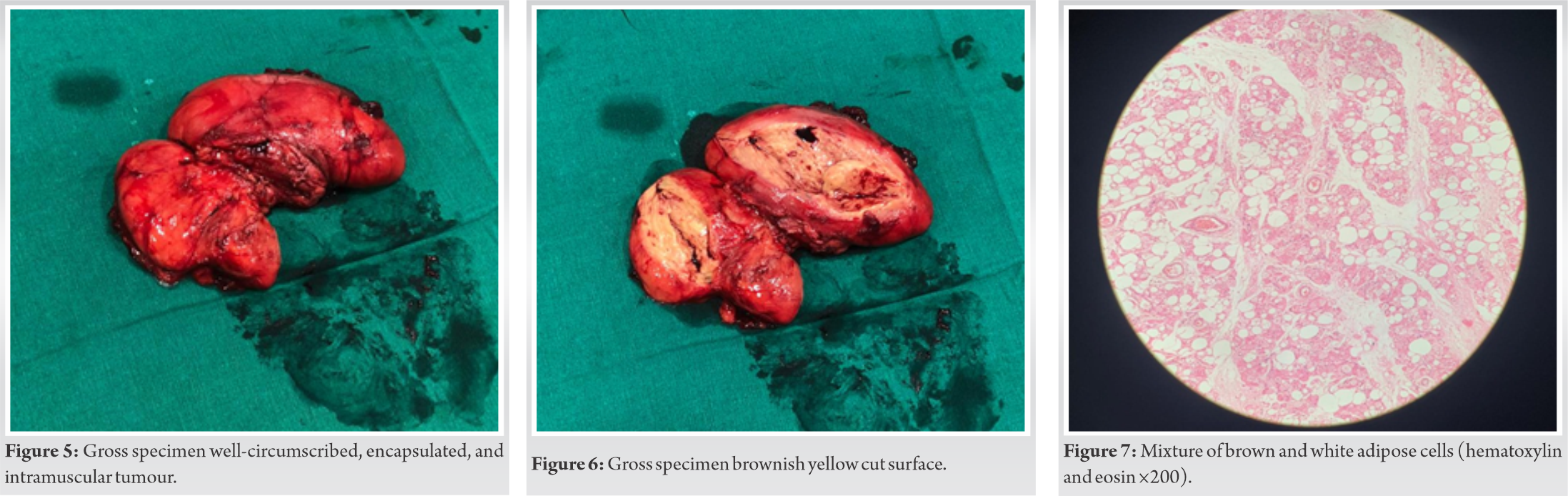
Hibernomas generally have decreased signal intensity compared with subcutaneous fat on T1-weighted MRI and fail to suppress on STIR or fat-saturated T2-weighted imaging. While surgical excision remains the gold standard of treatment and diagnosis, MRI or CT findings such as these may be reassuring in cases of poor surgical candidates or patients declining surgical intervention. Incisional biopsy is not recommended secondary to hypervascularity and potential for bleeding complications [1]. Cytogenetic analysis of hibernomas has consistently revealed rearrangements of chromosome bands 11q13–21.9. However, these findings are not unique to hibernomas and have also been reported in lipomas and liposarcomas [7]. Macroscopically, hibernomas are well‑circumscribed, encapsulated, lobulated soft greasy mass of usually 5–10 cm size. The cut surface reveals a yellow to red-brown appearance with rare areas of hemorrhage. Microscopic sections reveal encapsulated tumors comprising large multivacuolated cells and univacuolated cells. Multivacuolated cells have an eccentric vesicular nucleus and characteristically fine granular, vacuolated cytoplasm. Four histological variants have been identified based on the tinctorial quality of hibernoma cells, the nature of the stroma, and the presence of a spindle cell component: typical (82% of cases), myxoid (8%), lipoma-like (7%), and spindle cell (2%) [8] Abundant capillaries with a lack of mitosis or atypia is a usual feature. The presence of atypia and lipoblasts helps to differentiate liposarcoma from lipoma and hibernoma. These adipocytic tumors can be reliably diagnosed with the help of molecular markers such as MDM‑2, CDK‑4, and p‑16 [4]. Treatment is complete surgical resection of the tumor. Local recurrence does not occur with complete excision. There are no reports of metastases or malignant transformation in the reviewed literature.
Hibernoma even though being rare benign soft-tissue tumor of brown fat origin, should be considered as a differential diagnosis along with atypical lipoma and low-grade liposarcoma. Complete excision should be the main goal of surgical intervention. No reported rate of recurrence was seen after complete surgical excision.
With <200 cases being reported, hibernoma should be considered as differential diagnosis of soft tissue tumors. Treatment is complete surgical excision of the tumor. There are no reports of metastases or malignant transformation in the reviewed literature.
References
- 1.Greenbaum A, Coffman B, Rajput A. Hibernoma: Diagnostic and surgical considerations of a rare benign tumour. BMJ Case Rep 2016;2016:bcr2016217625. [Google Scholar]
- 2.Chen CL, Chen WC, Chiang JH, Ho CF. Interscapular hibernoma: Case report and literature review. Kaohsiung J Med Sci 2011;27:348-52. [Google Scholar]
- 3.Pujani M, Khan S, Jetley S, Raina PK. Intramuscular hibernoma of the scapular region misdiagnosed on cytology as a malignant lesion: A report of a rare case. Iran J Pathol 2017;12:406-9. [Google Scholar]
- 4.Patil SD, Sheik AR, Tewari V, Mutreja D. Hibernoma: A missed diagnosis! Indian J Pathol Microbiol 2019;62:461-3. [Google Scholar]
- 5.Reichel T, Rueckl K, Fenwick A, Vogt N, Rudert M, Plumhoff P. Hibernoma of the upper extremity: Complete case of a rare but benign soft tissue tumor. Case Rep Orthop 2019;2019:6840693. [Google Scholar]
- 6.Daubner D, Spieth S, Pablik J, Zöphel K, Paulus T, Laniado M. Hibernoma--two patients with a rare lipoid soft-tissue tumour. BMC Med Imaging 2015;15:4. [Google Scholar]
- 7.Cipriano CA, Gray RR, Fernandez JJ. Hibernomas of the upper extremity: A case report and literature review. Hand (NY) 2015;10:547-9. [Google Scholar]
- 8.Furlong MA, Fanburg-Smith JC, Miettinen M. The morphologic spectrum of hibernoma: A clinicopathologic study of 170 cases. Am J Surg Pathol 2001;25:809-14. [Google Scholar]










