Lateral malleolar giant cell tumour is rare but this type of tumour can be managed by biological options, and the most preferable option will be the ipsilateral proximal fibula.
Dr. Kunal Mondal, Subuddhipur, Beltala, Green Park, P. O+P. S-Baruipur, Kolkata - 700144, West Bengal, India. E-mail: kunal.doc91@gmail.com
Introduction:A giant cell tumor is a locally aggressive non-cancerous tumor. It usually develops near a joint at the end of the bone. Most occur in the long bones of the legs and arms. Presently, we are considering a case of Ggiant cell tumor over lateral malleolar region with the line of management.
Case Report: A 21-year-old male patient came with left ankle swelling over lateral malleolar region with subsequent episodes of pain during walking. Radiographic investigation suggestive of Ggiant cell tumour which was managed by en block resection of tumour with reconstruction of lateral malleolus using a proximal fibular graft, harvested from same side with protecting the neurovascular structures and used it as a newly reconstructed lateral malleolus with proper fixation.
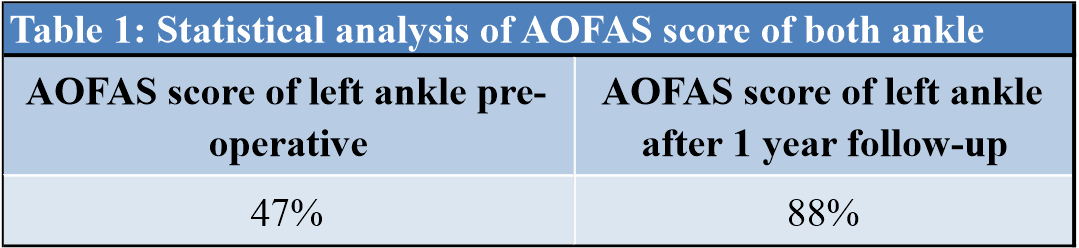
Conclusion:Post -operative functional outcome was estimated by using AOFAS score with radiographic evaluation of ankle mortis. Both implied a satisfactory outcome which conclude that though a giant cell tumour localized on the lateral malleolus are rare, but it can be managed by en bloc resection and restore the ankle biomechanics with a reverse proximal fibular graft.
Keywords:Giant cell tumour, lateral malleolus, reverse proximal fibular graft, ankle mortis.
A giant cell tumor localized on the distal fibula is rare, although it is a tumor of giant cell variety originating from the epiphysis. Occasionally, it requires total exeresis due to its locally aggressive property. Resection of the lateral malleolus can produce instability of the ankle and can potentially induce valgus deformity. Several techniques have been described for the reconstruction of the lateral malleolus in cases of benign or malignant tumors. It can be obtained using a reverse proximal fibular graft from the same side following the en-block resection of the tumor.
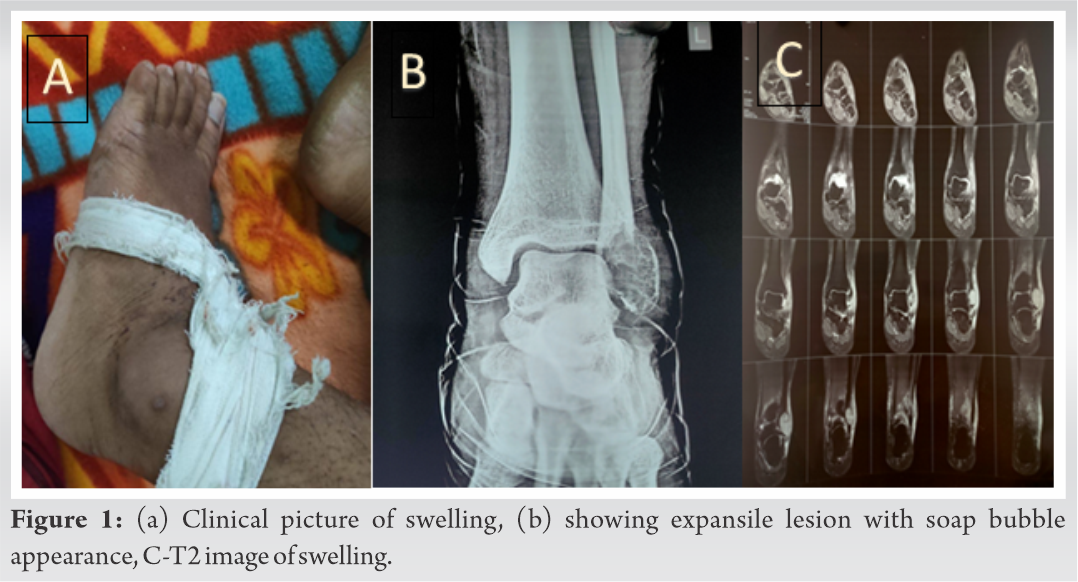
A 21-year-old male consulted for pain and swelling over left ankle (Fig. 1a) over 5 months with difficulty in walking. A swelling on the external side of the left ankle was noticed upon clinical examination, with no signs of inflammation and infection. Articular motions were free, with the dorsiflexion angle measured at 10° and the plantar flexion angle measured at 25°. Radiographic examination showed a 5 cm lytic lesion on the lateral malleolus (Fig. 1b). Anteroposterior and lateral radiographs showed single epiphyseal expansile lesion extending into metaphysis with soap bubble appearance. The cortex of the fibula had thinned; however, the lesion was clearly defined with no periosteal reaction. MRI of left ankle region shows well defined T1 Hypointense and T2 Hyperintense/STIR (Fig. 1c) lesion in the lateral malleolus. Computerized tomography scan revealed cortical break medially. No other significant findings over general and systemic examination. The histologic analysis confirmed the diagnosis of giant cell tumor.
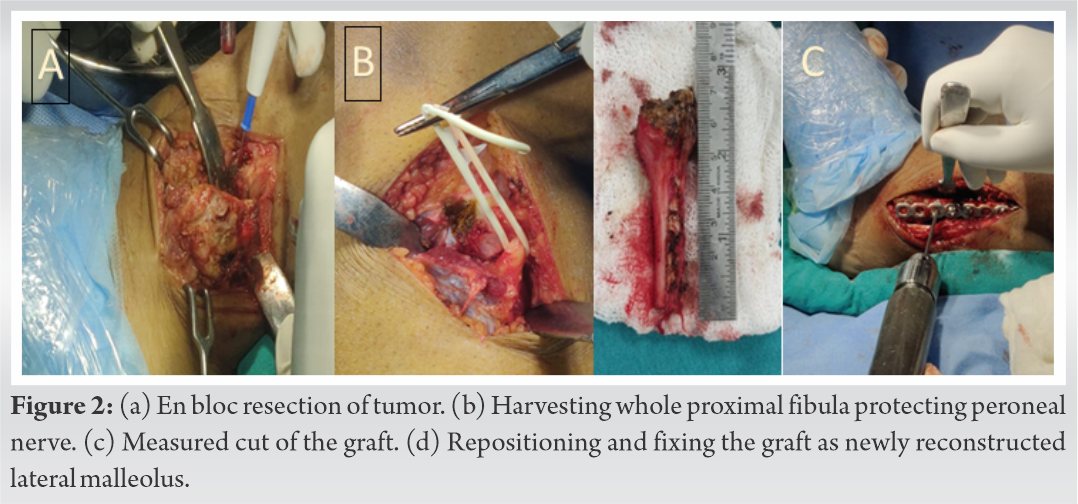
The patient was positioned in supine. We proceed with direct lateral approach. En bloc resection of the tumor was done, carrying the distal tibiofibular joint. Measurement was taken as a reference for graft harvesting of proper length. After meticulous dissection of the neurovascular bundle with protecting the common peroneal nerve (Fig. 2a-b), the proximal fibula was removed after proper measured cut (Fig. 2c), reversed, and fixed as a new lateral malleolus with plate and screw support over syndesmotic joint (Fig. 2d). The proximal end ligaments (fibular collateral ligaments with tendons of biceps femoris) were attached to the tibia to improve the stability. Vascular anastomosis was not done. After the transfer, the lateral malleolus was stable during passive motion and stress test intraoperatively. The contour of the ankle was satisfactory. The peroneal longus and brevis tendon sheath were repaired. Histopathological examination confirmed the diagnosis of giant cell tumor. Initial post-operative period was uneventful. At 1 month mobility of the ankle was slightly limited dorsiflexion +5 degree and plantar flexion at 10 degrees without any signs of wound dehiscence. Swelling and pain had resolved. Gradual weight bearing started at 3 months into a well molded weight bearing cast. The patient was given complete weight bearing at 5 months with satisfactory functional outcome (Fig. 3a). At 1-year post-operative, good range of motion was found at clinical examination; the trophic state is good with no signs of infection. Ankle mobility became +10° dorsiflexion (Fig. 3b) during knee extension and +15° plantar flexion. There was no ankle laxity and no palpatory gap over the newly reconstructed distal fibula. There was no pain during contraction of lateral compartment muscle. Palpation over the peri-articular region was painless. Syndesmotic screw was left in situ. In Radiographs, both medial and lateral columnar spaces were maintained with talocrural angle was evaluated closely for preservation of ankle biomechanics. Here, the Talocrural angle of newly reconstructed left ankle is 87 degrees compared to the right ankle which is 78 degrees. There was a radiolucent gap at junction of graft over proximal end, but it was well supported by plate which did not cost any functional progression (Fig. 3c). Furthermore, it limits the stress rise over proximal screw systems. Functional evaluation was done by AOFAS ankle hindfoot scoring system. Pre-operative AOFAS score of left ankles was 47% which became 88% on 12 months follow-up post-operatively (Table 1). When compared with the right ankle as standard (100%), there was no statistically significant difference on numerical evaluation of ankle function.
Reconstruction of lateral malleolar defects can be successfully done by ipsilateral proximal fibula. Points in favor are morphological similarity, minimal intra-operative complication, low positional hazards, minimal donor site complications, and vascular anastomosis can be avoided, functional outcome will be far better. Hence, despite of other methods, a reverse proximal fibula transfer should be used for lateral rmalleolar econstruction.
Management of Giant cell tumor at lateral malleolus includes:
En block resection of tumor. Reconstruction of the lateral malleolus.
Moreover, the most preferable method of doing this is using a reverse proximal fibular graft aided by plates and screws including syndesmosis fixation.
References
- 1.Shoji H, Koshino T, Marcove RC, Thompson TC. Subperiosteal resection of the distal portion of the fibula for aneurysmal bone cyst. J Bone Joint Surg Am 1970;52:1472-6. [Google Scholar]
- 2.Papagelopoulos PJ, Savvidou OD, Mavrogenis AF, Galanis E, Shaughnessy WJ, Unni KK, et al. Lateral malleolus en bloc resection and ankle reconstruction for malignant tumors. Clin Orthop Relat Res 2005;437:209-18. [Google Scholar]
- 3.Eger W, Schorle C, Zeiler G. Giant cell tumor of the distal fibula: Fifteen-year result after en bloc resection and fibula reconstruction. Arch Orthop Trauma Surg 2004;124:56-9. [Google Scholar]
- 4.Springfield D. Autograft reconstruction. Orthop Clin North Am 1996;27:483-91. [Google Scholar]
- 5.Jamshidi K, Mazhar FN, Masdari Z. Reconstruction of distal fibula with osteo-articular allograft after tumor resection. Foot Ankle Surg 2013;19:31-5. [Google Scholar]
- 6.Faure P, Canovas F, Bonnel F, Teot L, Quatra F, Giovannini UM, et al. Free osteocutaneous scapular apophysis flap for reconstruction of the lateral malleolus. Ann Plast Surg 2001;47:328-31. [Google Scholar]
- 7.Delloye C, van Cauter M, Dufrane D, Francq BG, Docquier PL, Cornu O. Local complications of massive bone allografts: An appraisal of their prevalence in 128 patients. Acta Orthop Belg 2014;80:196-204. [Google Scholar]
- 8.Carrell WB. Transplantation of the fibula in the same leg: Transplantation of the fibula for loss of the tibial diaphysis. J Bone Joint Surg Am 1938;20:627-34. [Google Scholar]
- 9.Beris AE, Lykissas MG, Korompilias AV, Vekris MD, Mitsionis GI, Malizos KN, et al. Vascularized fibula transfer for lower limb reconstruction. Microsurgery 2011;31:205-11. [Google Scholar]
- 10.Wood MB. Free vascularized fibular grafting 25 years’ experience: Tips, tech-niques, and pearls. Orthop Clin North Am 2007;38:1-12. [Google Scholar]
- 11.Henry SL, Frome BA, Pederson WC. Vascularized bone transfer for severe injury around the ankle. Microsurgery 2009;29:353-60. [Google Scholar]
- 12.Dieckmann R, Ahrens H, Streitburger A, Budny TB, Henrichs MP, Vieth V, et al. Reconstruction after wide resection of the entire distal fibula in malignant bone tumours. Int Orthop 2011;35:87-92. [Google Scholar]
- 13.Lee SH, Kim HS, Park YB, Rhie TY, Lee HK. Prosthetic reconstruction for tumours of the distal tibia and fibula. J Bone Joint Surg Br 1999;81:803-7. [Google Scholar]