Early repair of proximal hamstring tears while respecting the anatomical landmarks give predictable surgical and functional outcomes.
Dr. Supreet Bajwa, Department of Orthopaedics, Sunshine Coast Orthopaedic Group, Queensland, Australia. E-mail: supreetbajwa90@gmail.com
Introduction:Proximal hamstring injuries are rarely encountered sport injuries which cause great functional impairment in the activities of performance. Since these injuries are rarely encountered in orthopedic training, many young surgeons find it challenging to explore and successfully perform the required repairs. The technical demands of tendon retraction, scar tissue formation along with a great possibility of nerve injury during surgical dissection make these procedures a nightmare for young surgeons.
Results:Between January 2020 and December 2021, 11 patients underwent a proximal hamstring repair at our practice. All cases were of acute hamstring tears and diagnosed on magnetic resonance imaging (MRI) evaluation post-injury. No repeat MRI was performed but the patients outcomes were judged based on clinical outcomes such as return to sport or the presence of residual pain. All patients reached their pre-injury level of activity within 6 months of surgical repair.
Conclusion:This technical note describes pearls of surgical repair of these injuries that help in better execution of such injuries with minimal soft tissue damage and complications.
Keywords:Proximal Hamstring tear, hamstring avulsion, hamstring repair.
As a trainee in orthopedics, I received a lot of advice while developing my surgical acumen. Most of it in the form of harsh past experiences of my senior colleagues while learning their own trades. One of my earliest lesson while assisting a senior surgeon was in the art of soft tissue handling with his exact words being, “Treat all soft tissues like you would treat your family.” That one statement developed a paranoia in me to be meticulous but also question myself thoroughly before each case to deliberate on all details and plan for contingency- incase I go wrong. In many ways, this one position of paranoia and self-doubt defines the success of my surgery.
Proximal hamstring repairs make me nervous especially after reading Cvetanovich et al. [1] on neural structures around the proximal hamstrings origin. To add further, I like many of my contemporaries do not see these injuries commonly during our orthopaedic residency. Compounded by the constant hammering of “Avoid going too far back, there’s danger lurking there!” during each of our initiating years in learning a conventional posterior hip replacement approach. I write this article with an experience of 11 acute proximal hamstring tears to clarify the risks involved in surgery and technical tips on avoiding them.
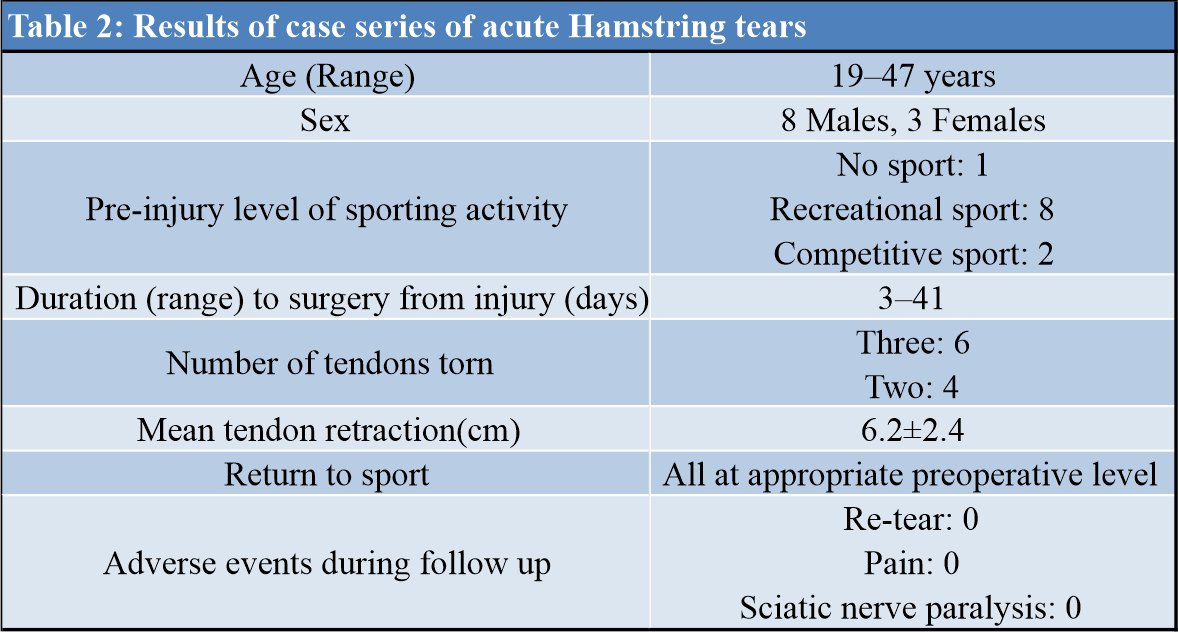
The proximal hamstrings attach to the ischial tuberosity (Figs. 1-3), a bony surface with ample soft tissue protection for the long hours of sitting that most of us employ in our current virtual learnings. Directly under the skin lies a thick layer of fat, separated by fibrous bands. The gluteal cutaneous brand of Sciatic nerve and perforating nerve run along this layer which adds to the trickery of the approach.

A newer source of complication (injury to Pudendal nerve) has been identified in recent literature [1] usually by the placement of retractors supers-medially to the ischium. With the Pudendal nerve lying 2–3 cm medial to the ischial tuberosity, a number of cases of transient Pudendal neuropraxia after surgery have been reported [9]. Avoid placing the retractors superomedial to the ischial tuberosity particularly as a tendency during suture anchor placement. The timing of surgery of these tendon repairs also contributes to the likelihood of nerve injuries. Subbu et al. [10] reported higher chances of nerve injury after 6 weeks of tendon rupture compared to repairs performed within 6 weeks. It is expected, greater scarring in prolonged delay in surgical management would increase chances of handling of neurological structures, thereby increasing rate of nerve damage during dissection.
Once exposed, the suture anchor placement on the ischium should be relatively straight forward. Start off by preparing the surface of the ischium by freshening with a corrugated curette or rongeur for the correct healing of tendons. Transosseous reinsertion of tendons is thereafter performed by first drilling 3-4 tunnels using an awl followed by suture anchor placement (Fig. 6, 7). Modified Mason-Allen stitches are then performed to secure the tendon using the sutures from anchors. The tendons are then pulled to the ischium using the free end of the sutures and tied down with the hip extended and knee flexed to about 30°.
Post-operatively, brace locked in 30° of knee flexion is maintained to prevent active extension for 2 weeks. the patient is mobilized immediately to walk non-weight-bearing as comfortable. At 2 weeks, active flexion is allowed and the brace is gradually removed by 6 weeks. Patient progresses from non-weight bearing to partial weight-bearing and full weight bearing at 2 weeks intervals from surgery. Isometric exercises of quadriceps and hamstrings are started immediately while active strengthening is started at 6 weeks post-operatively with full activities resuming between 12 and 16 weeks post-operatively.
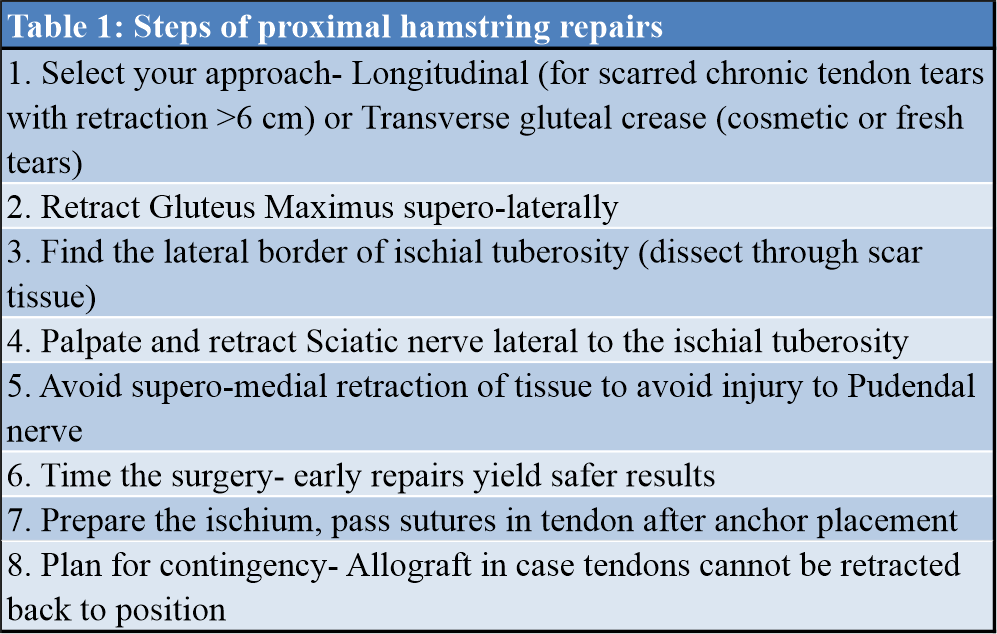
Between January 2020 and December 2021, 11 patients underwent a proximal hamstring repair at our practice. All cases were of acute hamstring tears and diagnosed on MRI evaluation post-injury. No repeat MRI was performed but the patients outcomes were judged based on clinical outcomes such as return to sport or the presence of residual pain (Table: 1, 2). All patients reached their pre-injury level of activity within 6 months of surgical repair.
Although described previously, these pearls of my own experience have heightened my pre-operative preparation for all repairs ultimately resulting in safer surgery and predictable outcomes.
Surgical repair of proximal hamstring tears has significantly improved functional outcomes when performed correctly. However, the rare presentation of the cases and limited knowledge of the anatomy around the ischium make it a difficult operation to perform.
Given the positive outcomes noted in previous literature, we recommend repair of avulsion injuries to the proximal hamstring. In this Technical Note, we present our approach for an anatomic proximal hamstring repair. This technique has been validated biomechanically, and we believe it provides a strong repair that can tolerate early rehabilitation, give good long-term results, and avoids the potential debilitating neurological problem of gluteal sciatica.
References
- 1.Cvetanovich GL, Saltzman BM, Ukwuani G, Frank RM, Verma NN, Bush-Joseph CA, et al. Anatomy of the pudendal nerve and other neural structures around the proximal hamstring origin in males. Arthroscopy 2018;34:2105-10. [Google Scholar]
- 2.Dierckman BD, Guanche CA. Endoscopic proximal hamstring repair and ischial bursectomy. Arthrosc Tech 2012;1:e201-7. [Google Scholar]
- 3.Moatshe G, Chahla J, Vap AR, Ferrari M, Sanchez G, Mitchell JJ, et al. Repair of proximal hamstring tears: A surgical technique. Arthrosc Tech 2017;6:e311-7. [Google Scholar]
- 4.Suppauksorn S, Nwachukwu BU, Beck EC, Okoroha KR, Nho SJ. Endoscopic approach to proximal hamstring avulsion repair. JBJS Essent Surg Tech 2020;10:e19.00037. [Google Scholar]
- 5.Blakeney WG, Zilko SR, Edmonston SJ, Schupp NE, Annear PT. A prospective evaluation of proximal hamstring tendon avulsions: Improved functional outcomes following surgical repair. Knee Surg Sports Traumatol Arthrosc 2017;25:1943-50. [Google Scholar]
- 6.Hamming MG, Philippon MJ, Rasmussen MT, Ferro FP, Turnbull TL, Trindade CA, et al. Structural properties of the intact proximal hamstring origin and evaluation of varying avulsion repair techniques: An in vitro biomechanical analysis. Am J Sports Med 2015;43:721-8. [Google Scholar]
- 7.Miller SL, Webb GR. The proximal origin of the hamstrings and surrounding anatomy encountered during repair. Surgical technique. J Bone Joint Surg Am 2008;90 Suppl 2 Pt 1:108-16. [Google Scholar]
- 8.Wilson TJ, Spinner RJ, Mohan R, Gibbs CM, Krych AJ. Sciatic nerve injury after proximal hamstring avulsion and repair. Orthop J Sports Med 2017;5:2325967117713685. [Google Scholar]
- 9.Popeney C, Ansell V, Renney K. Pudendal entrapment as an etiology of chronic perineal pain: Diagnosis and treatment. Neurourol Urodyn 2007;26:820-7. [Google Scholar]
- 10.Subbu R, Benjamin-Laing H, Haddad F. Timing of surgery for complete proximal hamstring avulsion injuries: successful clinical outcomes at 6 weeks, 6 months, and after 6 months of injury. Am J Sports Med 2015;43:385-91. [Google Scholar]