Lipoblastoma in children warrants a high index of suspicion in any patient who presents with slow growing painless mass especially in the extremities.
Dr. Abdulaziz Adnan Altammar, Department of Orthopaedics, Al Razi Hospital, Shuwaikh Area, Kuwait city, P.O Box: 4078, 13001, Suffix. E-mail: Abdulaziz.a.92@outlook.com
Introduction: Lipoblastoma is a rare mesenchymal benign tumor of the white fat cells that affect mostly infants and children below 3 years old. MLipoblastoma can be found in various locations in the body, however, it is usually located in the extremities, lower extremities in particular.
Case Report: We describe a case of a 2-year-old Middle Eastern boy who has a rare lipoblastoma of his left shoulder that is unusual.
Conclusion: The most common presentation of this rare tumor is a child younger than 3 years old with asymptomatic, painless, rapidly growing mass that warrants an appropriate index of suspicion to avoid misdiagnosis. Complete excision with free margins is fundamental as a definitive treatment of this benign tumor to eradicate any chance of recurrence or any possible complications including compressive symptoms, magnetic resonance imaging may be helpful in identifying the nature of the mass, however, the diagnosis confirmed postoperatively through histological and cytogenetic analysis. Chromosomal analysis is quite helpful in differentiating lipoblastoma from liposarcoma because they have different management and prognosis.
Keywords: Lipoblastoma, high index of suspicion, complete excision.
Lipoblastoma is relatively rare benign rapidly growing neoplasm of embryonal fat. The majority of these tumors affecting infants and children in their early childhood, a few cases reported in adults. In pediatrics, adipose tissue neoplasia is a rare disease, accounting for approximately 6% of all soft-tissue tumors [1]. The previous reported cases showed a slight male predominance. Typical presentation of a case of lipoblastoma is a painless, non-tender rapidly enlarging mass; however, symptoms can occur if the mass affects the adjacent structures [2]. As illustrated by the previous literatures that around two-third of the cases originated from the extremities, although there are some reported cases of lipoblastoma which has arisen from scrotum, trunk, neck, and retroperitoneal soft tissues [3]. Extremity arising lipoblastoma has been seen less often in most recent case reports that make it less common lately [4]. These benign neoplasms differ from myxoid liposarcoma, which has a quite similar presentation, in their cellular immaturity. Appropriate level of suspicion is crucial. In this manuscript will demonstrate a rare case of lipoblastoma originating from the shoulder of a 2-year-old boy which was difficult to diagnose preoperatively because of the unusual location of the mass
A 2-year-old boy previously healthy, he has no history of any birth or congenital abnormalities. In addition, there was no familial history of tumors referred with his parents to our orthopedic oncology department in Al Razi Hospital complaining of swelling on his left shoulder noticed by his mother 2 weeks ago. The boy was completely healthy and he meets his developmental milestone and immunizations.
On physical examination, he is afebrile and vitally stable, there was an approximately 2 cm firm mass rapidly increasing in size in a progressive course on his left shoulder, it was not tender at all, no warmness, no erythema, or any skin discoloration. His laboratory investigations and inflammatory markers were all within the normal range.
Ultrasound-guided biopsy is done for the boy and revealed a heterogeneous intramuscular lesion, measured 2.3 cm with fair vascularity at the center, suggesting for biopsy.
Magnetic resonance imaging (MRI) for the left shoulder with contrast is requested and demonstrated that there is intramuscular lesion arising from the posteroinferior fibers of the deltoid muscle, the lesion is lobulated, contains internal thin separations, and has areas of fat intensity (Fig. 1, 2). Two enlarged axillary lymph nodes are noted 6*3 mm and 8*4 mm. The lesion is separable from axillary nerve and circumflex arteries .
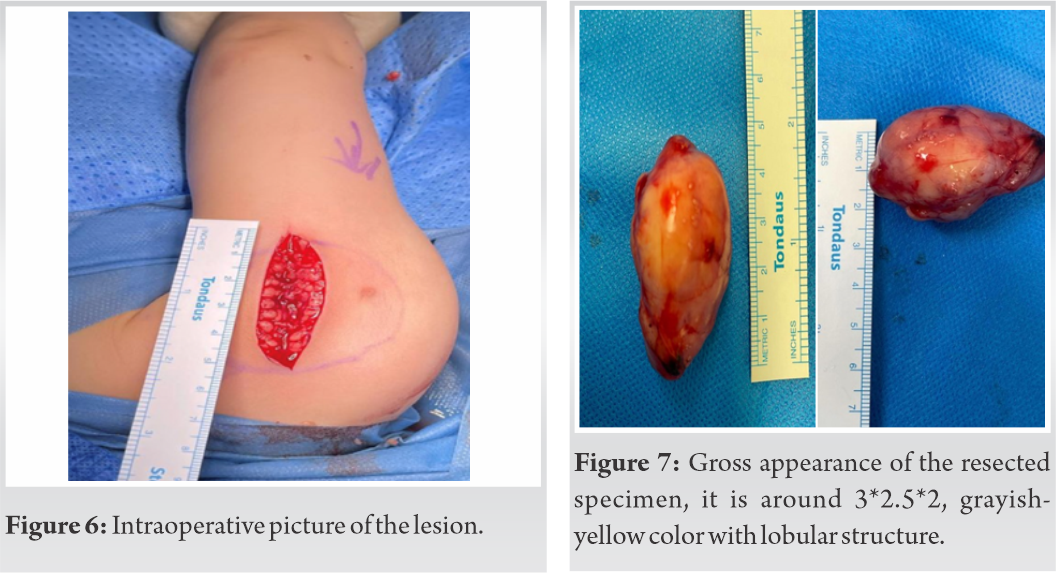
The histopathology grossly described the mass as 4.5*2.5*2.0 cm with lobulated smooth outer surface, the mass was tan in color with focally bluish and yellowish areas. Cut section was solid and showed fatty lobules separated by fine white fibrous trabeculae. Occasional areas of hemorrhage were seen.
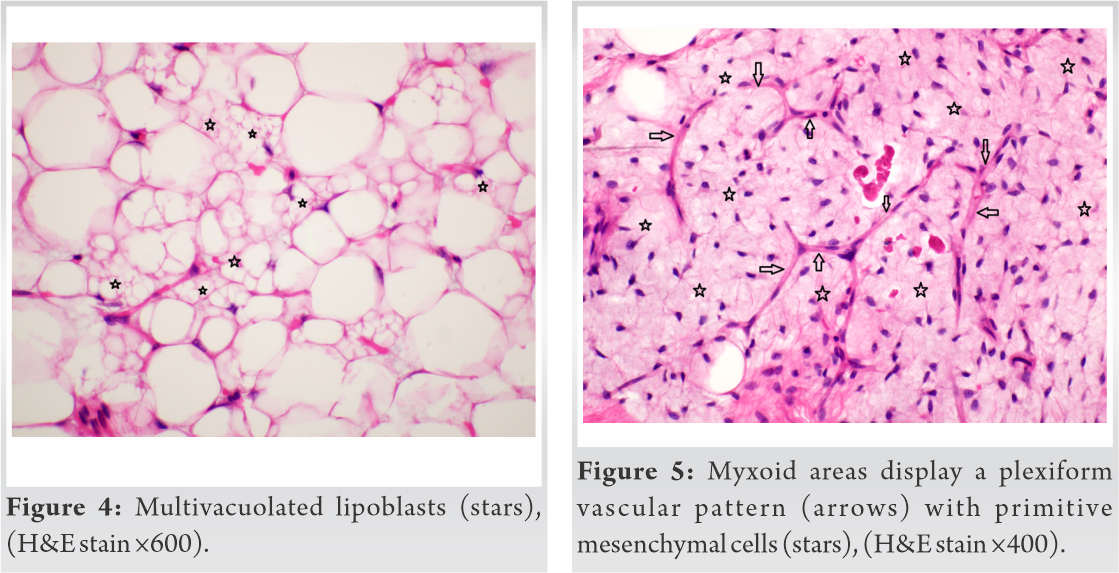
The microscopic description of the biopsy was presenting features of lipoblastoma, characterized by sheets of adipocytes separated by fibrovascular septa within myxoid background (Fig. 3). The fat cells showed a spectrum of maturation, ranging from primitive stellate and/or spindled mesenchymal cells (Fig. 4) to multivacuolated (Fig. 5) with mature adipocytes at the center (Fig. 4). The background myxoid areas showed plexiform vascular pattern (Fig. 6). No increased mitosis and necrosis were seen.
Shortly after the biopsy result, the boy was taken to the operation theater (Fig. 7). The mass was completely excised (Fig. 8). The operation went uneventful; there were no surgical or post-surgical complications. The patient is followed up in the outpatient clinic for 24 months with great outcome.
Lipoblastomas are best described as a rare benign soft-tissue tumor of the fat cells, which affect predominately infants and children in their early childhood [3]. The majority of the affected cases are children below 3 years old. Adipose tissue tumors are rare accounting for 15% of all benign soft-tissue tumors that affect children under 3 years old. The previous literature has illustrated that there is slight male predominance as male-to-female ration 3:1, however, some reported cases emphasized that the gender factor is inconclusive [5]. The vast majority of lipoblastomas originate from the extremities accounting for around 70%, although there are some reported cases of lipoblastoma in scrotum, mediastinum, vagina, and mesenteric and other locations. Lipoblastoma has been known by many names previously, such as embryonal lipoma, fetal lipoma, infantile lipoma, and benign childhood adipocyte tumor [6]. The precise pathogenesis of lipoblastoma is still unknown [7]. In 1926, tumor of immature cells was first described as lipoblastoma by Jaffe [8], whereas Vellios described fetal fat tissue neoplasm in postnatal period as lipoblastomatosis [8].
There are two types of adipose tissue neoplasms. The first is a well-differentiated, superficial, encapsulated, and localized known as lipoblastoma, while the diffuse and deep multicentric invasive form and fat cells tumor is lipoblastomatosis. In the majority of cases, lipoblastomatosis tends to invade adjacent soft tissue and muscular planes unlike lipoblastomas that occur superficially in the subcutis [9].
In spite of the benign nature of these neoplasms and the zero potential of metastasis, there is high recurrence rate around 14–25%, so occasionally, it requires several excisions [5]. Lipoblastoma is a benign lesion and lack of metastatic ability, however, a close follow-up is recommended for 2–5 years due to the high rate of recurrence [10]. There is a high recurrence rate around 50% if it arises from the black with intraspinal extension [11]. . If recurrence happens in lipoblastoma it will mostly be on the same previous site,as recurrence to different sites has not been reported yet[7].Local recurrence has been reported after 10 years of excision [9]. Clinical presentation is usually like a rapidly growing mass, which is totally painless and soft in consistency without any skin discoloration or constitutional symptoms. It warrants a high index of suspicion to ovoid misdiagnosis or a delay in diagnosis that might harm the patients. Imaging modalities such as ultrasonography, computed tomography (CT) scan, or MRI are occasionally helpful, however, a final diagnosis cannot be made before surgery, by microscopic analysis. Ultrasonography is useful in detecting fluid collection and vascularity [7]. CT scan with intravenous contrast might reveal a heterogeneous fat density lesion [12]. MRI is the image modality of choice for several reasons including the ability of MRI to illustrate the anatomical extent, tissue involvement, tumor composition, tumor extension, and for surgical planning [4]. Therefore, the absolute and definitive treatment for lipoblastoma is total excision of the lesion to avoid any chance of recurrence.
Macroscopic appearance of lipoblastoma is usually encapsulated, grayish-yellow parenchyma composed of lobulated soft-tissue mass [9]. Tumor size of all cases is ranging from 2 cm to 9 cm [13].
Microscopic appearance of both lipoblastoma and lipoblastomatosis is a wide range of cellular maturation and differentiation including primitive mesenchymal cells, lipoblasts, mature adipocytes, and spindle cells [14].
The common differential diagnoses of lipoblastoma are myxoid liposarcoma and hemangiomas.
Histologically, lipoblastomas are commonly described and recognized by the presence of vacuolated lipoblasts within the lobules of adipose tissue. The differential diagnosis of lipoblastoma histologically involves lipoma, myxoid liposarcoma, and well-differentiated liposarcoma [15].
It is very difficult to differentiate histologically between liposarcoma and lipoblastoma, helpful findings including the lack of lobulation variable growth pattern and increase in nuclear atypia are seen in liposarcoma [16]. The presence of lipoblasts is one of the important findings in distinguishing lipoblastoma from other lipomatous tumors [17].
In certain cases, the histopathological evaluation is inconclusive; at this point, cytogenetic study is recommended. The typical chromosomal anomaly in myxoid liposarcoma is in t (12; 16) (q 13; p11), while in lipoblastomas, the abnormality is in the long arm of chromosome 8 (5). Translocation of the PLAG1 oncogene that is located in chromosome band 8q12 is a distinctive feature of lipoblastoma [17]. Around 70% of tested cases through cytogenetic analysis showed the presence of translocation of PLAG1 gene that is located at 8q12.1 chromosome [18]. PLAG1 gene is can be seen easily by FISH testing technique [18].
Lipoblastoma is a benign tumor of the adipose tissue which originated mostly from the extremities and trunk and affects almost exclusively children below 3 years old. Our aim is to remind the reader of considering this rare tumor in the differential diagnosis of infants and young children with rapidly growing mass for better management and prognosis, and the importance of complete surgical resection of the mass followed by a continuous follow- up to discover any sign of recurrence.
Diagnosing a child with lipoblastoma can be challenging, especially if the child presents with an unusual site and clinical symptoms. The treating clinician should have a high index of suspicion for diagnosing a lipoblastoma in children in upper body. A thorough assessment is crucial.
References
- 1.Delsordo R, Cavaliere R, Sidoni A, Colella R, Bellezza G, Intercostal lipoblastoma: A case report and reviw of the literature. J Pediatr Surg 2007;42:e9-11. [Google Scholar]
- 2.Vo N, Mashiana M, Vo C, Ward K, Nguyen J. Atypical presentation of lipoblastoma of a 9 month old. Ear Nose Throat J 2019;98:261-2. [Google Scholar]
- 3.Whyte AM, Powell N. Mediastinal lipoblastoma of infancy. Clin Radiol 1990;47:205-6. [Google Scholar]
- 4.Susam-Sen H, Yalcin B, Kutluk T. Lipoblastoma in children: Review of 12 cases. Pediatr Int 2017;59:545-50. [Google Scholar]
- 5.McVay MR, Wagne JE, Jackson R, Smith D. Surgical management of lipoblastoma. J Pediatr Surg 2006;41:1067-71. [Google Scholar]
- 6.Kamal NM, Jouini R, Yahya S, Haiba M. Benign intracostal lipoblastoma in a 4 month old infant: A case report and review of literature. J Pediatr Hematol Oncol 2011;26:e9-12. [Google Scholar]
- 7.Han J, Kim H, Youn J. Analysis of clinical features of lipoblastoma in children. Pediatric Hematologu Oncol 2017;34:212-20. [Google Scholar]
- 8.Kim W, Park KW, Lee SE, Jung SE. Lipoblastoma. J Pediatr Surg 2001;36:905-7. [Google Scholar]
- 9.Seguier-Lipszyc E, Baazov A, Fichman S, Ash S, Freud E. Current management of lipoblastoma. Eur J Pediatr 2018;177:237-41. [Google Scholar]
- 10.Childress KJ, Hicks J, Wu H. Liboblastoma in labia. J Pediatr Adolesc Gynecol 2016;29:e29-99. [Google Scholar]
- 11.Kassem R, Faiz A, Kumar SY. Lipoblastoma and lipomatosis in children-case report. J Pediatr Surg Case Rep 2017;19:4-5. [Google Scholar]
- 12.Ambusaidi F, Al-Mammari L, Al-Brashdi Y. Imaging features of lipoblastoma. Int J Pediatr Adolesc Med 2021;???:???.2352-6467. [Google Scholar]
- 13.Schoolmeester JK, Michal M, Steiner P, Michal M, Folpe AL, Sukov WR. Lipoblastoma-like tumor of the vulva: A clinicopathologic, immunohistochemical, fluorescence in situ hybridization and genomic copy number profiling study of seven cases. Mod Pathol 2018;31:1862-8. [Google Scholar]
- 14.Shen L, Amin S, Chamlin S, Mancini A. Varied presentation of pediatric lipoblastoma: Case series and review of literature. Pediatr Dermatol 2017;34:180-6. [Google Scholar]
- 15.Gerhard-Hartmann E, Wiegering V, Benoit C, Meyer T, Rosenwald A, Maurus K, et al. A large retroperitoneal lipoblastoma as an incidental finding: A case report. BMC Pediatr 2021;21:159. [Google Scholar]
- 16.Armenise T, Gentise O. Lipoblastoma in infant: Our experience. J Pediatr Surg Case Rep 2015;3:63-4. [Google Scholar]
- 17.Nitta Y, Miyachi M, Tomida A. Identification of a novel BOC-P1AG1 fusion gene in a case of lipoblastoma. Biochem Biophys Res Commun 2019;512:49-52. [Google Scholar]
- 18.Ferreira J, Esteves G, Fonseca R. Fine needle aspiration of lipoblastoma: Cytological, molecular, and clinical features. Cancer Cytopathol. 2017;125:934-49. [Google Scholar]