CLAP therapy may emerge as a novel treatment for chronic osteomyelitis.
Dr. Takahiro Niikura, Department of Orthopaedic Surgery, Kobe University Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe 650-0017, Japan. E-mail: tniikura@med.kobe-u.ac.jp
Introduction: Chronic osteomyelitis is difficult to cure definitively, because local areas are often covered with sequestrum and scar tissues with a poor blood flow; these may render systemic antibiotic administration ineffective. We present a case of chronic osteomyelitis that was successfully treated with continuous local antibiotic perfusion (CLAP) through an intramedullary antibiotic perfusion (iMAP) pin.
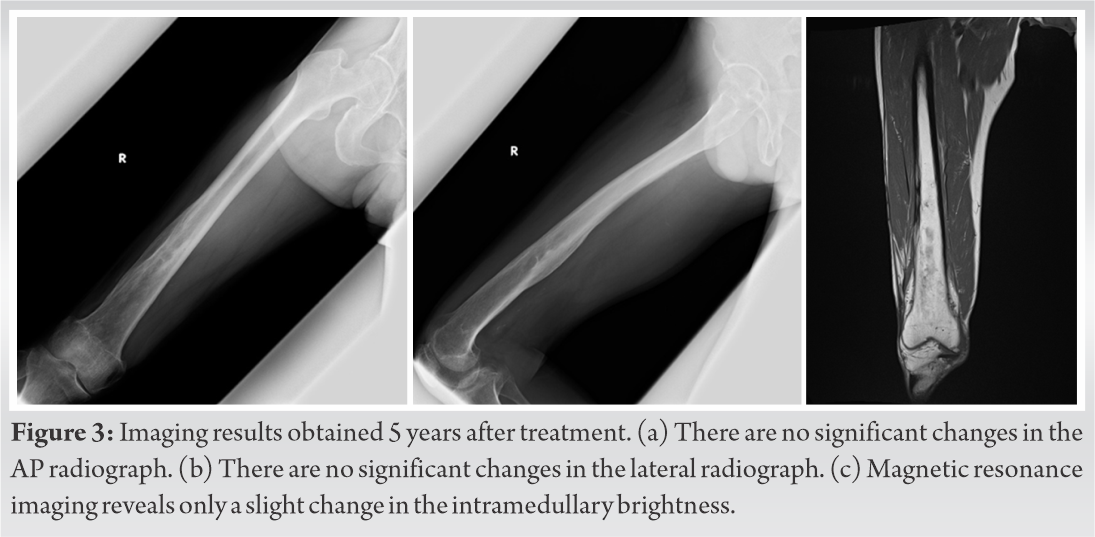
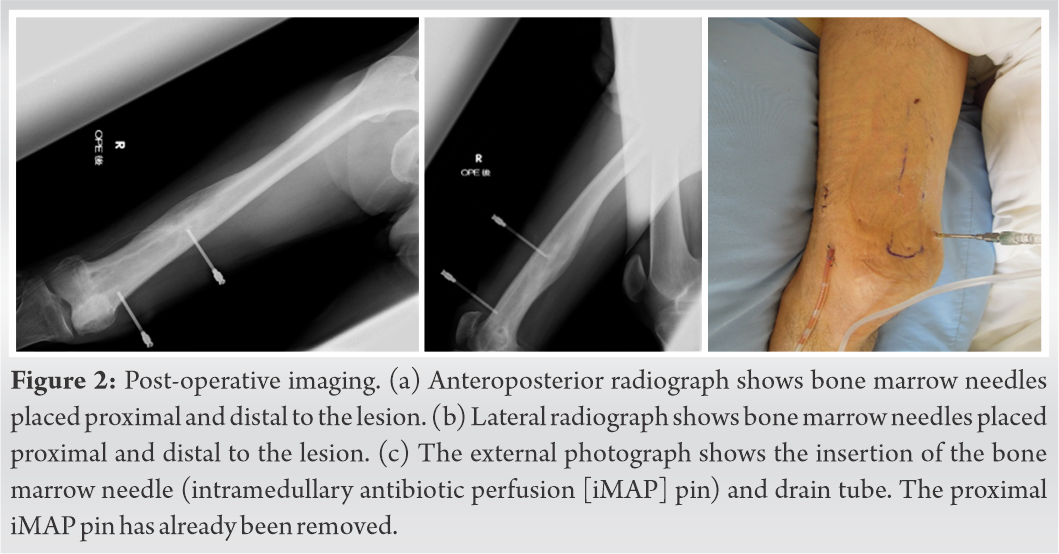
Case Presentation:A 65-year-old man who suffered an episode of the right femoral osteomyelitis at the age of 15 years experienced a relapse at the age of 63 years. Systemic administration of antibiotics could not control the infection; thus, a surgery was performed. A bone marrow needle (i.e., an iMAP pin; diameter: 3 mm) was percutaneously inserted, from the front, distally and proximally to the cystic lesion in the distal femur. After washing through the iMAP pins, the pins were left indwelling. A closed drain tube was placed on the bone surface, which was close to the fistula of the bone marrow lesion. CLAP therapy was then initiated. Gentamicin was continuously infused through the iMAP pin at a rate of 2 mL/h and drained using the tube. Accordingly, 2.4 mg/mL, 1.2 mg/mL, and 1.2 mg/mL of gentamicin were administered for 4 days using two iMAP pins, for 5–8 days using two iMAP pins, and for 9–15 days using one iMAP pin, respectively, with a syringe pump. The iMAP pins and the drain tube were removed 15 days after the initiation of the CLAP therapy. The C-reactive protein level normalized 25 days postoperatively. The patient recovered full range of motion of the knee joint and recreational sports activity without recurrence of osteomyelitis for 5 years after the therapy.
Conclusions: CLAP therapy allows local administration of a sufficient concentration of antibiotics and device removal after treatment is simple. This may be a novel treatment for chronic osteomyelitis.
Keywords: Chronic osteomyelitis, continuous local antibiotic perfusion, femur, gentamicin, intramedullary antibiotic perfusion.
Chronic osteomyelitis rarely has systemic manifestations. However, it is difficult to eradicate completely, because pus, sequestrum, and infected granulation are present in the local bone and surrounding tissues, which can cause a relapse after several years [1, 2]. Infection may be controlled by antibiotics; however, the local areas are often covered with sclerotic bone or scarred soft tissue with a poor blood flow. Thus, systemic antibiotic administration may be ineffective. Surgical treatment is based on the complete removal of the sequestrum with radical debridement and topical administration of antibacterial agents. However, radical debridement can result in large dead spaces and bone defects, requiring large-scale soft tissue and bone reconstruction [3, 4].
In our hospital, difficult-to-treat bone and soft-tissue infections are treated with continuous local antibiotic perfusion (CLAP), in which, antibiotics are continuously circulated through the infected lesion. Furthermore, cases with osteomyelitis are treated by “intramedullary antibiotic perfusion” (iMAP) and cases with soft-tissue infection are treated by “intra-soft-tissue antibiotic perfusion;” some cases are treated with a combination of both [5]. Thus, we report a case of chronic osteomyelitis that was treated with CLAP therapy.
We present the case of a 65-year-old man with a history of diabetes and hypertension. At the age of 15 years, he underwent focal curettage for acute osteomyelitis of the right femur and remained asymptomatic for approximately 50 years. At the age of 63, he developed a swelling with local heat and redness in the distal portion of his right thigh; thus, he visited a nearby clinic. Blood examination revealed a C-reactive protein (CRP) level of 4.89 mg/dL. He was diagnosed with an acute relapse of osteomyelitis and oral antibiotic treatment was started. The condition gradually improved and remission was achieved. However, 2 months later, osteomyelitis recurred in the right distal femur, and he was referred to our hospital. Radiographs revealed bone hypertrophy, thickening of the bone cortex, and osteosclerosis located distally in the femoral shaft (Fig. 1a, b). Bone scintigraphy revealed a high uptake of technetium-99m in the distal femur. Magnetic resonance imaging showed a wide range of intramedullary and soft-tissue signal changes in the distal femur (Fig. 1c).
The treatment of chronic osteomyelitis involves debridement of the infected bone and soft tissues and systemic and local administration of antibiotic agents. Inadequate debridement may lead to a recurrence [1, 2]. Extensive bone and soft-tissue loss can occur with definitive debridement and reconstruction of the resulting bone defects includes the use of autologous bone grafts, vascularized bone grafts, the Masquelet technique, local or free flaps, and the Papineau technique [3, 4]. Long-term treatments are not only a physical burden, but also a financial burden. Thus, our treatment method aimed to minimize bone and soft-tissue debridement and achieve a high concentration of the antibacterial drug continuously and locally using an intramedullary needle. We previously introduced the CLAP treatment for acute fracture-related infections and reported good clinical results [5]. Because CLAP allows local administration of a high concentration of antibacterial agents, it can be expected to eradicate biofilms. It has been reported that to eradicate biofilms, antimicrobial agents are required at concentrations of 100–1000 times the minimum inhibitory concentrations; these are termed as the minimal biofilm eradication concentrations (MBECs) [6, 7]. However, local delivery of antimicrobial agents at MBEC through intravenous administration is impossible without adverse systemic effects. CLAP is safe as it can be administered by percutaneous insertion of a bone marrow needle into the lesion and aspirated by drainage tube to prevent unnecessary systemic inflow while simultaneously monitoring the antibacterial drug concentration in the blood. On treatment completion, the needle and the drain tube can be removed without making an incision, which is very convenient. Other local antibiotic administration methods include antibiotics containing cement or biomaterials, which require a short period of time to ensure an effective local concentration and surgery to remove it after the end of the treatment [8, 9, 10]. The bactericidal effect of dose-dependent agents increases with an increase in the dose. Conversely, the bactericidal effect of time-dependent agents reaches a plateau as the number of doses increases. Therefore, we considered that gentamicin was suitable for local administration; it has been reported to be locally administered for musculoskeletal infections [11, 12, 13].
The end of CLAP therapy is determined by comprehensively evaluating three criteria: Local findings, blood test results, and local heat. However, if the treatment is unsuccessful, the conventional debridement method may be considered instead of continuing the CLAP therapy indiscriminately. The disadvantage of this treatment is that the surface of the bone marrow needle is too smooth to avoid leakage of the antibiotic solution, and can easily loosen and come off. To solve these problems, we are currently developing a pin with a thread attached to the pin tip.
The indications for CLAP therapy are acute and chronic osteomyelitis [14], infection after instrumented spinal surgery [15], and fracture related infections [5]. There are no contraindication cases at this time.
CLAP therapy may be a useful, minimally invasive method for the treatment of chronic osteomyelitis.
Osteomyelitis, which is difficult to treat through conventional means, can be treated with CLAP therapy. CLAP therapy is minimally invasive and can be used to locally administer a sufficient concentration of antibiotics. Device removal after treatment is simple as well. Thus, CLAP therapy may emerge as a novel treatment for chronic osteomyelitis.
References
- 1.Lima AL, Oliveria PR, Carvalho VC, Cimerman S, Savio E. Recommendations for the treatment of osteomyelitis. Braz J Infect Dis 2014;18:526-34. [Google Scholar]
- 2.Cierny G, Mader JT, Penninck JJ. A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res 2003;7-24. [Google Scholar]
- 3.Rahimnia A, Fitoussi F, Penneçot G, Mazda K. Treatment of segmental loss of the tibia by tibialisation of the fibula: A review of the literature. Trauma Mon 2012;16:154-9. [Google Scholar]
- 4.Taylor BC, French BG, Fowler TT, Russell J, Poka A. Induce membrane technique for reconstruction to manage bone loss. J Am Acad Orthop Surg 2012;20:142-50. [Google Scholar]
- 5.Maruo A, Oda T, Miya H, Muratsu H, Fukui T, Oe K, et al. Intra-medullary antibiotics perfusion (iMAP) for the control of fracture-related infection early after ostosynthesis. J Orthop Surg (Hong Kong) 2021;29:23094990211051492. [Google Scholar]
- 6.Ceri H, Olson ME, Stremick C, Read RR, Morck D, Buret A. The Calgary biofilm device: New technology for rapid determination of antibiotic susceptibilities of bacterial biofilms. J Clin Microbiol 1999;37:1771-6. [Google Scholar]
- 7.Tassew DD, Mechesso AF, Park NH, Song JB, Shur JW, Park SC. Biofilm formation and determination of minimum biofilm eradication concentration of antibiotics in Mycoplasma hyopneumoniae. J Vet Med Sci 2017;79:1716-20. [Google Scholar]
- 8.Ferguson J, Diefenbeck M, McNally M. Ceramic biocomposites as biodegradable antibiotic carriers in the treatment of bone infections. J Bone Joint Infect 2017;2:38-51. [Google Scholar]
- 9.Anagnostakos K, Wilmes P, Scmitt E, Kelm J. Elution of gentamicin and vancomycin from polymethylmethacrylate beads and hip spacers in vivo. Acta Orthop 2009;80:193-7. [Google Scholar]
- 10.Pesch S, Hanschen M, Greve F, Zyskowski M, Seidl F, Kirchhoff C, et al. Treatment of fracture related infection of the lower extremity with antibiotic eluting ceramic bone substitutes: Case series of 35 patients and literature review. Infection 2020;48:333-44. [Google Scholar]
- 11.De Meo D, Cannari FM, Petriello L, Persiani P, Villani C. Gentamicin-coated tibia nail in fractures and nonunion to reduce fracture-related infections: A systematic review. Molecules 2020;25:5471. [Google Scholar]
- 12.Knaepler H. Local application of gentamicin-containing collagen implant in the prophylaxis and treatment of surgical site infection in orthopaedic surgery. Int J Surg 2012;10:S15-20. [Google Scholar]
- 13.Maczynska B, Secewicz A, Smutnicka D, Szymczyk P, Dudek-Wicher R, Junka A, et al. In vitro efficacy of gentamicin released from collagen sponge in eradication of bacterial biofilm preformed on hydroxyapatite surface. PLoS One 2019;14:e0217769. [Google Scholar]
- 14.Himeno D, Matsuura Y, Maruo A, Ohtori S. A novel treatment strategy using continuous local antibiotic perfusion: A case series study of a refractory infection caused by hypervirulent Klebsiella pneumoniae. J Orthop Sci 2020;19:30350. [Google Scholar]
- 15.Takahashi H, Koda M, Funayama T, Noguchi H, Miura K, Mataki K, et al. Continuous local antibiotic perfusion for patients with surgical site infection after instrumented spinal surgery; a novel technique to retain the implants. J Clin Neurosci 2021;93:70-4. [Google Scholar]