A strong suspicion and proper evaluation for Tuberculosis is necessary when the patient presents with labial abscess associated with osteomyelitis of pubis.
Dr. Divesh Jalan, Department of Orthopaedics, Central Institute of Orthopaedics, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi - 110 029. India. E-mail: dvsh_jalan@yahoo.com
Introduction: Skeletal tuberculosis (TB) accounts for 10–15% of all cases of extra-pulmonary TB. The involvement of pubis is extremely rare with only 40 cases of pubic bone TB reported in the medical literature. The presentation of the disease with labial abscess is much rarer with only one case reported till now.
Case Report:A 23-year-old female presented with symptoms of pain and swelling in the right groin. The patient was evaluated with hematological and radiological investigations and the diagnosis of Tubercular osteomyelitis of pubis with labial abscess was confirmed using AFB staining and culture of the aspirate. The patient was subsequently managed with Anti-tubercular chemotherapy for 18 months and the lesion healed with excellent functional outcome.
Conclusion:Tubercular Osteomyelitis of the pubis is a rare disease with varied clinical presentation. Timely diagnosis and anti-tubercular chemotherapy usually result in complete recovery.
Keywords: Tubercular osteomyelitis, pubis, labial abscess, skeletal tuberculosis, extra-pulmonary tuberculosis.
Tuberculosis (TB) is a major health burden in developing countries like India. However, its incidence is also on the rise in affluent societies of the world owing to the increasing evidence of immunodeficiency disorders, use of immunomodulators, use of biologics, poor nutrition, and unhealthy lifestyle. Skeletal TB accounts for 10–15% of all cases of extra-pulmonary tuberculosis [1, 2]. It can involve uncommon sites of the body [3] such as the pubic bone, sacroiliac and sternoclavicular joints [4]. Only 40 cases of pubic bone TB has been described in the medical literature till now [5] out of which only one case has presented with labial swelling [6]. Here, we report one such case of a 23-year-old female with tubercular osteomyelitis of pubis with right labial abscess.
A 23-year-old female presented in the Orthopedic Outpatient department with chief complaints of pain in right groin region for 9 months and swelling for last one month. The pain was continuous, insidious in onset, dull aching in nature, mild-to-moderate in intensity which increased on exertion and relieved with rest and medication. The patient had no history of fever, weight loss or any other constitutional symptoms. There was no history of TB or any contact with TB. There was no history of any trauma and gynecological or surgical procedures.
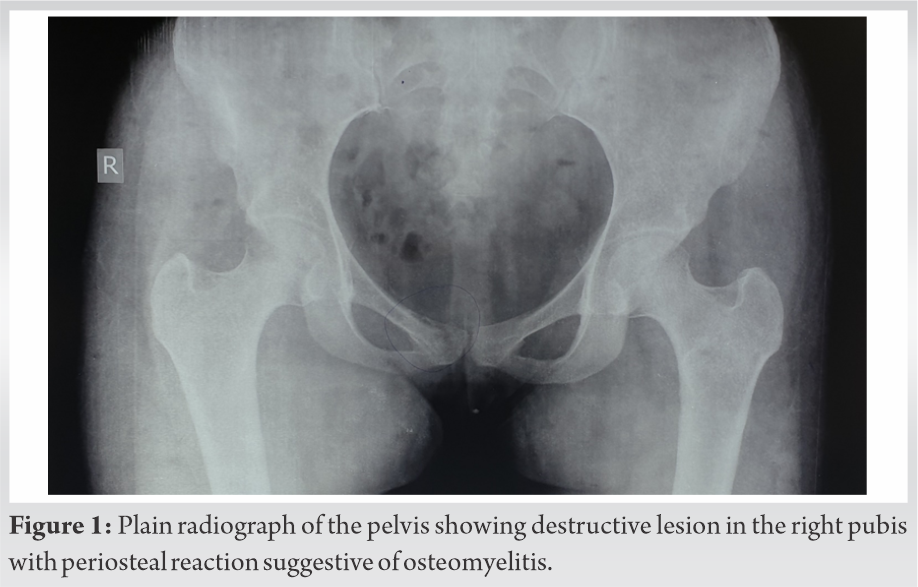
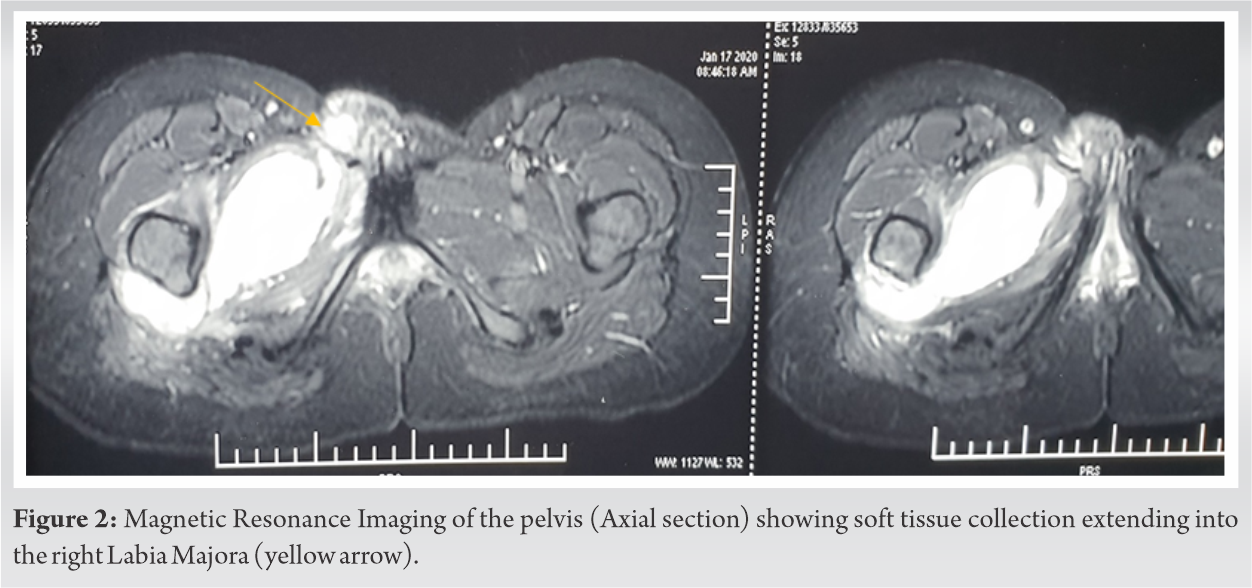
On examination, an ill-defined fluctuant swelling was present over the right labium. The overlying skin was erythematous with a local rise of temperature. There was severe tenderness over the swelling. The palpation did not reveal any inguinal lymphadenopathy and there was no distal neurovascular deficit. The movements at the hip joint were normal. Hematological investigations showed elevated ESR (22 mm in 1st h) and C-reactive protein (CRP) (36 mg/dl). The Montoux test was positive with (38 × 45 mm) of induration. The radiograph of the pelvis revealed a destructive lesion in the right pubis extending into the superior pubic rami with periosteal reaction suggestive of chronic osteomyelitis (Fig. 1). The patient was further investigated with Magnetic Resonance Imaging (MRI) which revealed oblong multiloculated multi-septate thick walled collection measuring 11.5 (TR) × 5.0(AP) × 5.1 (CC) involving right adductor longus, brevis, obturator externus muscles with focal bony destruction along right superior pubic rami (Fig. 2). Anteriorly, one of the loculi measuring 2.8 × 2.5 × 2.1 cm was seen extending into the subcutaneous plane anterior to the right pubic symphysis. There was mild fluid in the right hip joint.
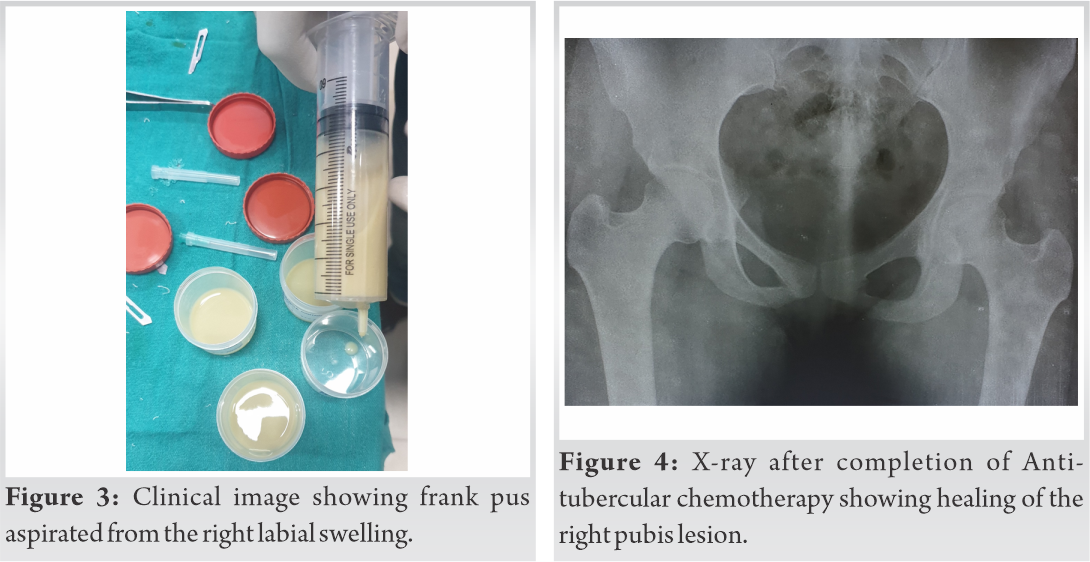
Subsequently, under all aseptic precaution, labial swelling was aspirated with 16 G needle which revealed frank pus (Fig. 3). It was then sent for microbiological investigations including Gram stain, AFB stain, culture and sensitive for aerobic and Mycobacterium tuberculosis and gene expert for TB. The AFB staining, Bactec Mycobacteria Growth Indicator Tube culture and gene expert for M. tuberculosis came out to be positive.
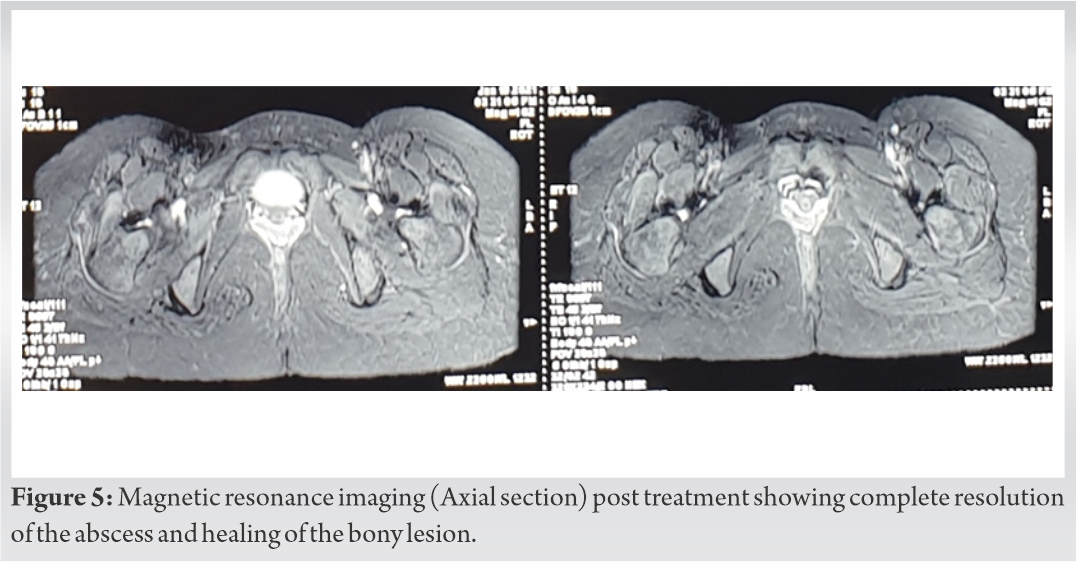
Hence, the final diagnosis of tubercular osteomyelitis of pubis with labial abscess was made and the patient was started on multidrug Anti-tubercular chemotherapy comprising of Rifampicin, Isoniazid, Ethambutol, and Pyrazinamide for 2 months as intensive phase and then Rifampicin, Isoniazid, Ethambutol for the next 16 months as continuous phase. The patient started improving clinically after two months of treatment with subsidence of pain and swelling and improvement of her daily activities. At 18 months, patient had no pain and swelling in the local area, the hematological (Hemogram, ESR, CRP) parameters were normal and radiological investigations (X-ray, MRI) revealed healing of the lesion (Fig. 4, 5). The ATT treatment was stopped and supportive treatment and physiotherapy was advised. At 2 years follow up, patient is asymptomatic and is able to do all her daily activities. She didn’t have any urinary complaints and was not sexually active.
Osteoarticular TB is the second most common site of extra-pulmonary TB after lymph nodes, with incidence of 10–15% of all cases of extra pulmonary-TB [7, 8]. The most common site is spine followed by hip, knee and ankle joints. The TB of pubis is rare with less than 40 cases reported in literature and the presentation with labial abscess is much rarer with only one case reported till now [6]. The clinical presentation in the case report by Shende et al. [6] was similar with pain and swelling in the labial region with no constitutional symptoms. However, the swelling was non-tender and the overlying skin was normal. The diagnosis and treatment was similar with our case. They, however, have not done radiographs to assess the bony destruction. The extent of the lesion was assessed only with MRI. The pubic symphysis TB was first reported by Thilsen in 1855 and later on by Hennies in 1888. The largest series is that of Sorrel with 26 cases reported in 1932 [9]. With the rising incidence of Human Immunodeficiency Virus and multi-drug resistant strains, use of immunomodulators and anti-cancer drugs, the incidence of extrapulmonary-TB and at atypical sites is on the rise.
The diagnosis of a tubercular infection is often delayed due to its resemblance with other inflammatory diseases such as osteitis pubis, pyogenic osteomyelitis of pubis, and adolescent osteochondrosis [10]. Therefore, it is important to differentiate the entity from other mimicking conditions. The clinical presentation is however similar in all the above condition that is suprapubic pain sometimes radiating to groin. Osteitis pubis is a self-limiting non-infective inflammation of the pubis and is often associated with Rheumatic disease, exertion, athletic activity, pregnancy, and following gynecological or urological surgery or trauma to pubic symphysis [11]. The patient complains of pain over the pubis but without any abscess formation. The symptoms are usually mild and decreases with time. Radiologically, destruction of symphysis pubis and pubis is often seen. The abscess can be seen with pyogenic and tubercular osteomyelitis. Staphylococcus aureus is the most common cause of pyogenic osteomyelitis. Bone Scintigraphy and MRI are more sensitive in the early stages for diagnosis. Three-phase bone scan can be helpful in the differential diagnosis of osteitis and osteomyelitis. Increased uptake in all three phases suggests osteomyelitis while increased uptake in just the mineralization phase is typical for osteitis pubis. Adolescent osteochondrosis of the pubic symphysis is a rare entity and is characterized by pain and tenderness over the pubic symphysis without any abscess formation. MRI is the investigation of choice.
Tubercular osteomyelitis of the pubis may spread from nearby anatomical locations [12, 13]. Sometimes lesion may present as a non-healing sinus or as a cold abscess [5]. Extension to the labia and its presentation as a labial swelling is exceptionally rare. An abscess may rupture into the urinary bladder and result in osteuria [14] and Pyuria [15]. Vulvo-vaginal TB [16] may also present as a labial swelling. However, it has an associated genital involvement with involvement of bone only in the later stage.
Debridement and curettage with antibiotic coverage is the mainstay of treatment of osteomyelitis and abscess formation. However, with the advent of effective anti-tubercular therapy, drainage of the abscess is usually not required, as in our case.
Tubercular Osteomyelitis of the pubis is a rare disease with varied clinical presentations. The presence of labial abscess should be properly investigated to rule out any underlying bony infection. Timely diagnosis and Anti-tubercular chemotherapy usually result in complete recovery.
TB although endemic in country like India, atypical presentation and locations are quite common. A strong suspicion and proper evaluation is necessary when the patient presents with labial abscess with osteomyelitis of pubis.
References
- 1.Ansari S, Amanullah MF, Ahmad K, Rauniyar RK. Pott’s spine: diagnostic imaging modalities and technology advancements. N Am J Med Sci 2013;5:404-11. [Google Scholar]
- 2.Pigrau-Serrallach C, Rodríguez-Pardo D. Bone and joint tuberculosis. Eur Spine J 2013;22 Suppl 4:556-66. [Google Scholar]
- 3.Bali K, Kumar V, Patel S, Mootha AK. Tuberculosis of symphysis pubis in a 17 year old male: A rare case presentation and review of literature. J Orthop Surg Res 2010;5:63. [Google Scholar]
- 4.Gamble JG, Simmons SC, Freedman M. The symphysis pubis. Anatomic and pathologic considerations. Clin Orthop Relat Res 1986;203:261-72. [Google Scholar]
- 5.Lal H, Jain VK, Kannan S. Tuberculosis of the pubic symphysis: Four unusual cases and literature review. Clin Orthop Relat Res 2013;471:3372-80. [Google Scholar]
- 6.Shende P, Gandhewar M, Gaikwad P, Nanaware S, Joshi PR. Labial swelling: A rare presentation of pubic bone tuberculosis. Trop Doct 2017;47:176-8. [Google Scholar]
- 7.Rajasekaran S, Dheenadhyalan J. Tuberculosis of bone and joints. In: Bulstrode C, Buckwalter J, Carr A, Marsh L, Fairbank J, Wilson-MacDonald J, Bowden G, editor. Oxford Textbook of Orthopaedics and Trauma. Oxford, UK: Oxford University Press; 2002. p. 1532-60. [Google Scholar]
- 8.World Health Organization. Treatment of Tuberculosis Guidelines. 4th ed. Geneva: World Health Organization; 2021. Available from: http://whqlibdoc.who.int/publications/2010/9789241547833_eng.pdf [Last accessed on 2021 Jul 05]. [Google Scholar]
- 9.Garg PK, Chaurasia A, Singh AP. An unusual cause of thigh swelling: Tuberculosis of the pubis. Am J Trop Med Hyg 2013;88:1-2. [Google Scholar]
- 10.Singh S, Arora S, Sural S, Dhal A. Tuberculosis of the pubic symphysis masquerading as osteitis pubis: A case report. Acta Orthop Traumatol Turc 2012;46:223-7. [Google Scholar]
- 11.Pauli S, Willemsen P, Declerck K, Chappel R, Vanderveken M. Osteomyelitis pubis versus osteitis pubis: A case presentation and review of the literature. Br J Sports Med 2002;36:71-3. [Google Scholar]
- 12.Balsarkar DJ, Joshi MA. Tuberculosis of pubic symphysis presenting with hypogastric mass. J Postgrad Med 2001;47:54. [Google Scholar]
- 13.Fares G, Pagani A. Tubercular osteitis of the pubis. Minerva Ortop 1966;17:459-69. [Google Scholar]
- 14.Aswathaman K, Devasia A. Osteuria. Urology 2008;71:546.e13. [Google Scholar]
- 15.Devarajan R, Ojha H, Desai KM, Chen K. Tubercular osteomyelitis of the pubic symphysis caseating into the bladder with concurrent tubercular pyonephrosis and epididymitis. BJU Int 2000;86:144. [Google Scholar]
- 16.Alhakeem M, Schneider A. Genital tuberculosis: A rare cause of vulvovaginal discharge and swelling. J Microbiol Infect Dis 2013;3:141-3. [Google Scholar]