The most common tumor which causes bone erosion is giant cell tumor of the tendon sheath (GCTTS) while the erosion is quite rarely caused by Fibroma of the tendon sheath (FTS).
Dr. Yuto Minagawa, Department of Orthopaedic Surgery, Showa University Fujigaoka Hospital, Yokohama, Kanagawa, Japan. E-mail: fujiortho@med.showa-u.ac.jp
Introduction:Fibroma of the tendon sheath (FTS) is a soft-tissue tumor strongly attaches to the tendon sheath. The most common tumor which causes bone erosion is giant cell tumor of the tendon sheath while the erosion is quite rarely caused by FTS.
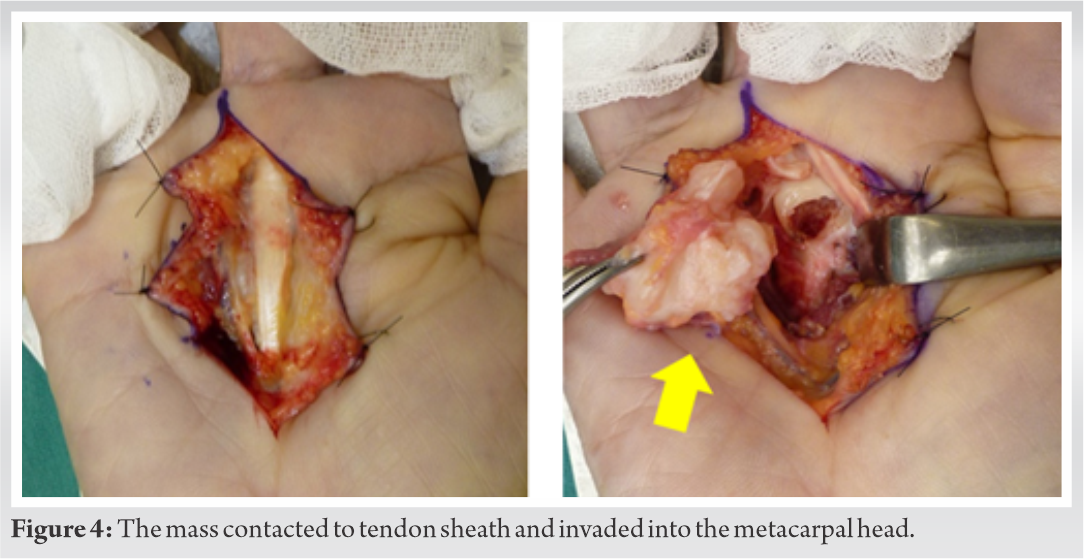
Case Report:A 50-year-old housewife presented a swelling around the A1 pulley of the right third finger as well as bone erosion and a trigger finger. Against our preoperative suspect as GTTS, the pathological findings showed FTS. The snapping disappeared after the surgery. At 2.5 years postoperatively, we found no recurrence.
Conclusion:FTS can be added to one of the differential diagnoses for tumor presenting bone erosion in fingers though our case is rare.
Keywords:Fibroma of tendon sheath, bone erosion, trigger finger.
Fibroma of the tendon sheath (FTS) is a soft-tissue tumor strongly attaches to the tendon sheath. It is most commonly observed in patients aged between 30 and 50 years on the upper extremities. In general, the tumors are small in size, with most sized between 1 and 2 cm [1]. The majority of patients presented no particular clinical symptoms other than a painless mass [1]. Surgery must be resected as the entire tumor including all tumor lobules to prevent local recurrence. FTS rarely causes bone lesions, and we have been able to find in only four cases. This is the fifth such case report. We reported a case presented bone lesion and trigger finger caused by FTS.
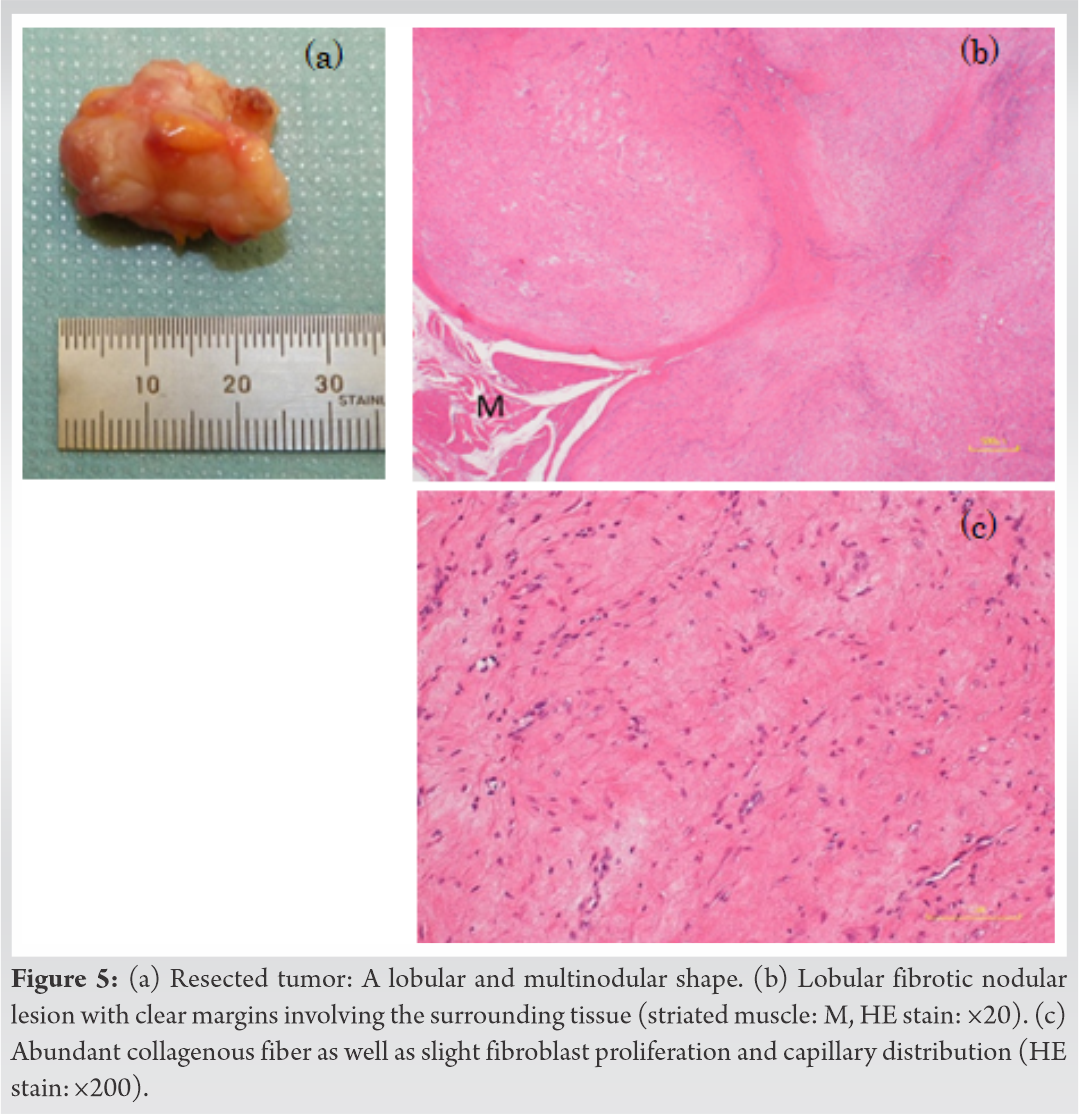
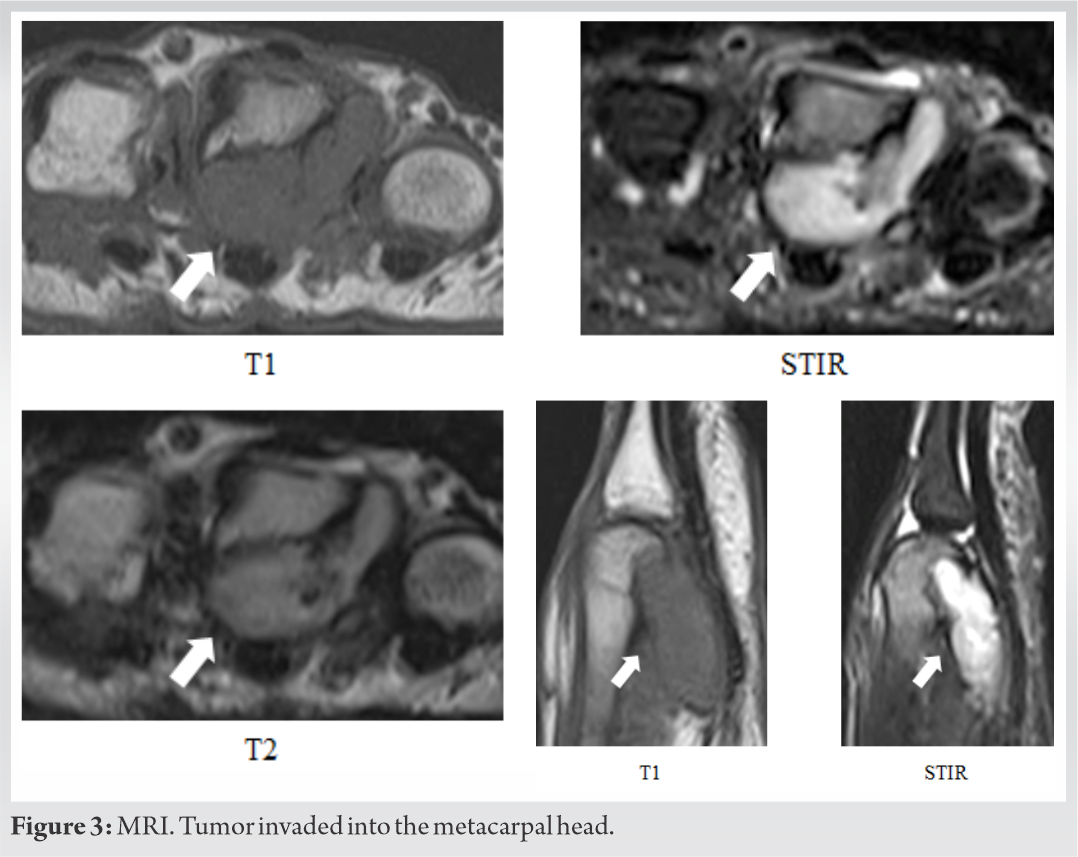
A 50-year-old housewife consulted a family doctor for her swelling around the A1 pulley in the right third finger and diagnosed as a trigger finger, and the lesion was treated by a tendon sheath injection. Resulting in no improvement, she consulted our hospital. On the initial examination, approximately 2 cm of an elastic hard mass was palpated on the ulnar side of the metacarpal head in the right third finger. The lesion was accompanied with tenderness and snapping. No restriction of the range of motion (ROM) of the finger existed. An oblique view of the plain radiograph indicated radiolucency in the metacarpal head (Fig. 1). 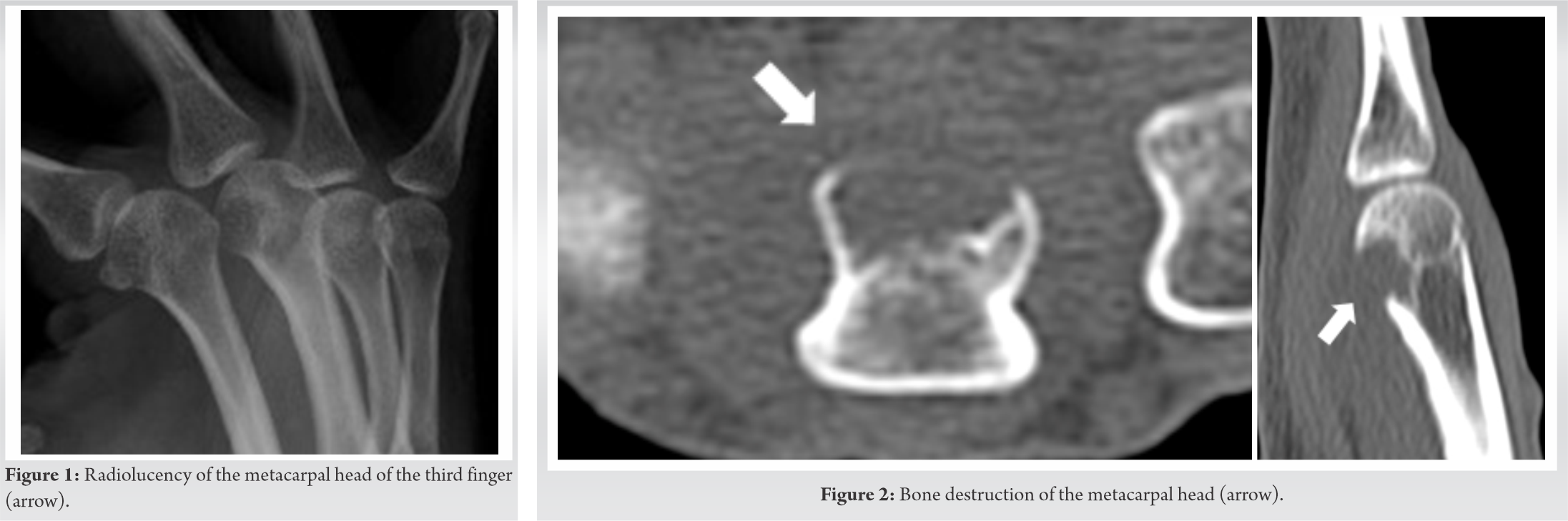
FTS is a soft-tissue tumor that strongly adheres to a tendon or tendon sheath. It is most commonly observed in patients aged between 30 and 50 years and is more common in males (75%) than in females (25%) [1]. The chief complaints include tenderness and pain in the affected area [1]. The vast majority (98%) of tumors occur on the extremities, with the preponderance on the upper extremities (87.5%) rather than in the lower extremities (12.5%) [1]. FTS is observed, in descending order of frequency, in the fingers (50%), hands (21%), wrists (12%), or knees (5%) [1]. Bone lesions have been observed in only two of 138 cases [1]. FTS tumors are circular, spherical, elliptical, or spindle in shape and have a clearly lobular structure [1]. In general, the tumors are small in size, with most sized between 1 and 2 cm [1]. Its microscopic finding has a lobular structure and strong adhesion to a tendon or tendon sheath as well as the presence of fibroblasts, collagen fibrosis in the stroma, and slit-like vascular channels [1]. Occasionally, FTS has several multinucleated giant cells inside, while it lacks macrophages – such as foam cells and siderophages – which often exist in GCTTS [2]. In the literature, the possible mean follow-up was 4.3 years in 54 of the 138 cases [1]. The recurrence rate in these 54 cases was 24%, of which 18% experienced a single recurrence and 6% experienced two recurrences [1]. FTS is usually surgically treated. It must be resected as the entire tumor including all tumor lobules to prevent local recurrence. Differential diagnoses of tumors accompanied with bone lesions include GCTTS, hemangioma, lipoma, schwannoma, glomus tumor, synovial chondromatosis, fibrosarcoma, rhabdomyosarcoma, clear cell sarcoma, epithelioid sarcoma, and rheumatoid arthritis [3, 4]. In rheumatoid arthritis, initially, the inflammatory tissue thickens at the bare areas and gradually extends into the joint space across the cartilaginous surfaces [5]. Our case had a lesion in the bare area just like rheumatoid arthritis. However, rheumatoid arthritis can be excluded from the differential diagnoses because our case lacked symptoms in other joints, inflammatory reaction, radiologic bone atrophy, and synovitis on MR scans. Bone lesion are caused sometimes by GCTTS but rare by FTS [1, 4, 6, 7]. According to Kitagawa’s review among 115 operated patients underwent with soft-tissue tumor or neoplasm in the hand, the most common diagnoses were GCTTS and ganglion [4]. Of 21 patients with bone lesions, two-thirds were GCTTS [4]. From the opposite viewpoint, half of GCTTS had related bone lesions [4]. On the other hand, Chung reported on the article that only two patients showed bone lesions among 138 patients with FTS [1]. Plate reported that many cases with bone lesions caused by GCTTS as pressure erosions [6].
Fletcher reported that the tumor pressure itself or phagocytes (i.e., basic cell in GCTTS) possibly causes the bone lesion in GCTTS [7]. On the other hand, unlike GCTTS, FTS has a structure characterized by fibroblasts, fibrous stroma, and slit-like vascular channels [1]. Because FTS does not include phagocytes, FTS can hardly cause bone lesions. In our case, the bone lesion can be brought about by the tumor pressure just like suggested by Kitagawa and Southwick [2, 4]. Fletcher pointed out when a soft-tissue tumor firmly attaches to a ligament or tendon, it often erodes into the bone marrow beyond the cortex due to high pressure [7]. In our case, the tumor grew up in a quite limited space surrounded by the tendon sheath, A1 pulley, and metacarpal bone. As the result, high pressure in the space seemed to cause the erosion.
At the surgery, we only removed the tumor. If a pathologic fracture occurred accompanied with the erosion, some reconstruction might be necessary such as bone transportation or cement filling or an internal fixation. Ultrasonography is recommendable as a simple and useful examination for identifying the location of tumor in the hand and also the cause of snapping finger [8]. We did not perform ultrasonographic examination. It was retrospectively unnecessary for the pre-operative diagnosis of the tumor because it could not distinguish FTS from GCTTS or other rare malignant tumors and normal trigger finger was already excludable before the surgery [9, 10].
We reported a case presented bone lesion and trigger finger caused by FTS. The representative tumor is GCTTS when a tumor attaches to the tendon sheath and is accompanied by bone lesion. However, as our case shows, FTS can be added to the differential diagnosis while FTS rarely shows such situation.
The cause of the trigger finger may be not only tenosynovitis and hypertrophy of flexor sheaths but also tumor. Pathological diagnosis is necessary because some tumors are malignant. Even benign tumors need to be completely resected to prevent local recurrence.
References
- 1.Chung EB, Enzinger FM. Fibroma of tendon sheath. Cancer 1979;44:1945-54. [Google Scholar]
- 2.Southwick GJ, Karamoskos P. Fibroma of tendon sheath with bone involvement. J Hand Surg 1990;158:373-5. [Google Scholar]
- 3.Lourie JA, Lwin KY, Woods CG. Case report 734. Skeletal Radiol 1992;21:273-5. [Google Scholar]
- 4.Kitagawa Y, Tamai K, Tsunoda R, Sawaizumi T, Takai S. Bone changes associated with soft-tissue tumors of the hand. J Nippon Med Sch 2012;79:267-73 [Google Scholar]
- 5.Sommer OJ, Kladosek A, Weiler V, Czembirek H, Boeck M, Stiskal M. Rheumatoid arthritis: a practical guide to state-of-theart imaging, image interpretation, and clinical implications. Radiographics 2005;25:381-98. [Google Scholar]
- 6.Plate AM, Lee SJ, Steiner G, Posner MA. Tumorlike lesions and benign tumors of the hand and wrist. J Am Acad Orthop Surg 2003;11:129-41. [Google Scholar]
- 7.Fletcher AG Jr., Horn RC Jr. Giant cell tumors of tendon sheath origin. Ann Surg 1951;133:374-85. [Google Scholar]
- 8.Tanaka Y, Gotani H, Yano K, Sasaki K, Miyashita M, Hamada Y. Sonographic evaluation of effects of the volar plate on trigger finger. J Orthop Sci 2015;20:999-1004. [Google Scholar]
- 9.Guerini H, Morvan G, Vuillemin V, Campagna R, Thevenin F, Larousserie F, et al. Ultrasound of wrist and hand masses. Diagn Intervent Imaging 2015;96:1247-60. [Google Scholar]
- 10.Fox MG, Kransdorf MJ, Bancroft LW, Peterson JJ, Flemming DJ. MR imaging of fibroma of the tendon sheath. Am J Roentgenol 2003;180:1449-53. [Google Scholar]