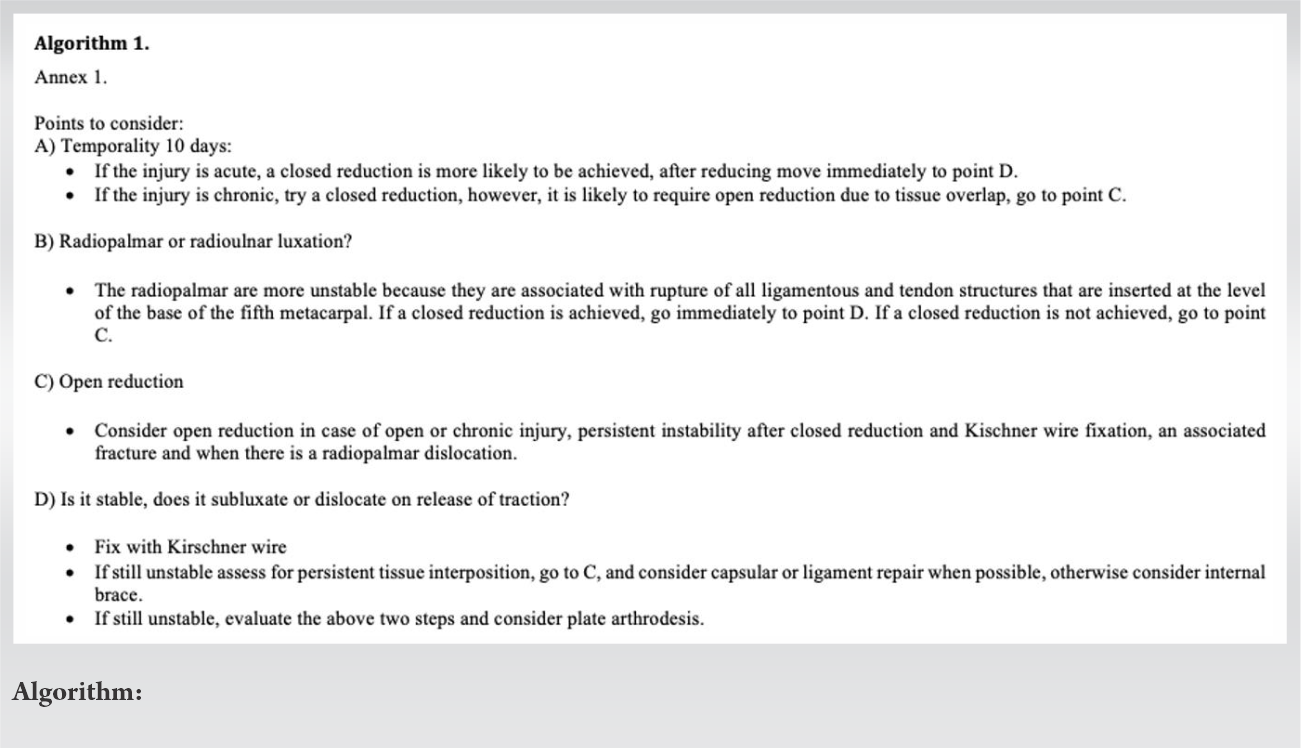
We propose a treatment algorithm for isolated dislocations of the carpometacarpal joint of the fifth finger to the palmar that is not diagnosed and treated early, the surgeon will have a vision of the probable best treatment option.
Dr. Jorge Luciano Villán, Department of Orthopedist and Traumatologist in Training, Universidad del Rosario, Bogotá, Colombia. E-mail: jorgevillangaona@gmail.com
Introduction: Isolated palmar carpometacarpal dislocation of the small finger is infrequent, this injury often goes unnoticed in the evaluation at the emergency room, for which physical evaluation and X-ray findings can avoid missing this diagnosis. We describe a case report and propose a treatment algorithm for isolated dislocations of the carpometacarpal joint of the fifth finger to the palmar that is not diagnosed and treated early, using this algorithm, the surgeon will have a vision of the probable best treatment option.
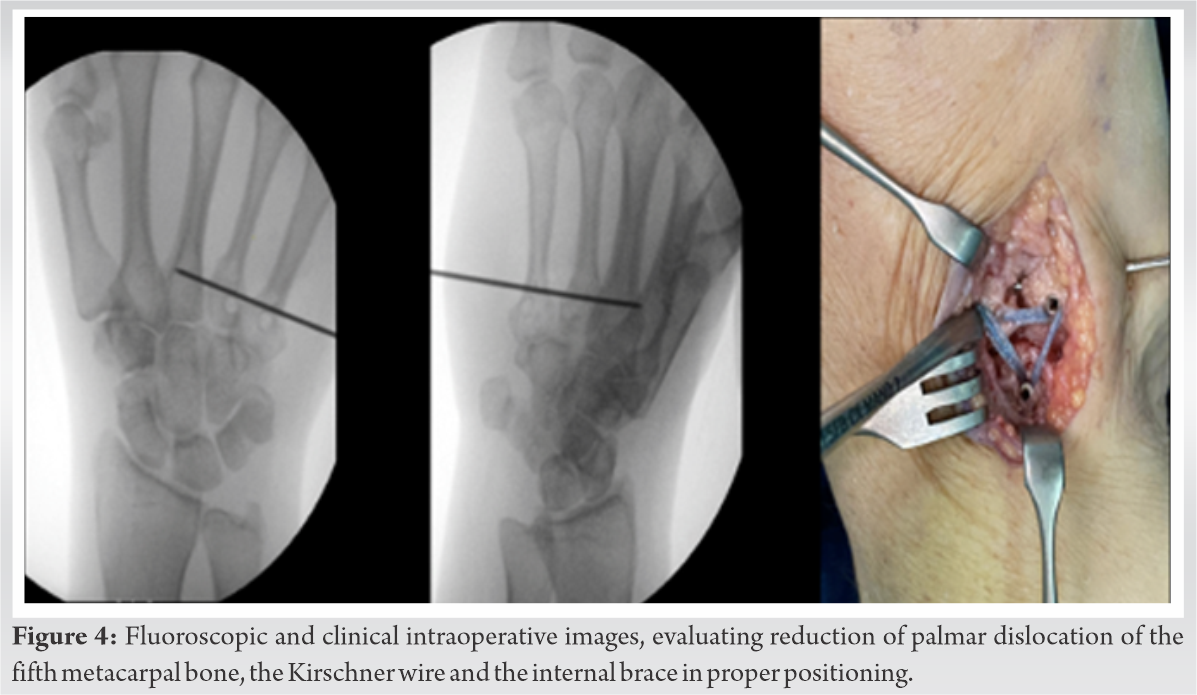
Case Presentation:A 50-year-old with late presentation of palmar dislocation of the fifth metacarpal bone, the diagnosis that went unnoticed in the initial emergency assessment. The patient was taken to an open reduction and internal fixation with an internal brace fixed at the base of the fifth metacarpal, the base of the fourth metacarpal and the hamate, and the fifth metacarpal was fixed to the fourth metacarpal with a Kirschner wire placed transversely to the axis of the metacarpal.
Conclusion: Physical evaluation and X-ray findings, physicians can avoid missing isolated palmar carpometacarpal dislocation of the small finger. Using this algorithm according to the temporality of the injury, direction of the dislocation, and stability of the joint, the surgeon will have a vision of the probable best treatment option.
Keywords: Dislocation, fifth metacarpal bone, treatment, late presentation.
<1% of patients with hand dislocation and/or fractures correspond to carpometacarpal luxation [1]. In 1621 hand injuries described by Dobyns et al., three were carpometacarpal dislocation. The most common dislocation at the carpometacarpal joint is the metacarpal of the fourth and fifth finger simultaneously in 45%, isolation from the fifth metacarpal in 28%, and dislocation of the second to fifth metacarpal in 15%, being more frequently toward dorsal [2, 3]. As an infrequent injury, clinical care is very important, since this injury often goes unnoticed in the initial evaluation at the emergency room, and 30% of carpal injuries can go undetected by radiography [2]. Physical evaluation and X-ray findings, physicians can avoid missing this diagnosis. The carpometacarpal joints play an important role in the grip of the hand [4]. Inadequate treatment can cause pain, compromise the ability to grip, and lead to instability and subsequent osteoarthritis [4]. The main objective of this article is to describe a case report, and propose a treatment algorithm for isolated dislocations of the carpometacarpal joint of the fifth finger to the palmar that is not diagnosed and treated early.
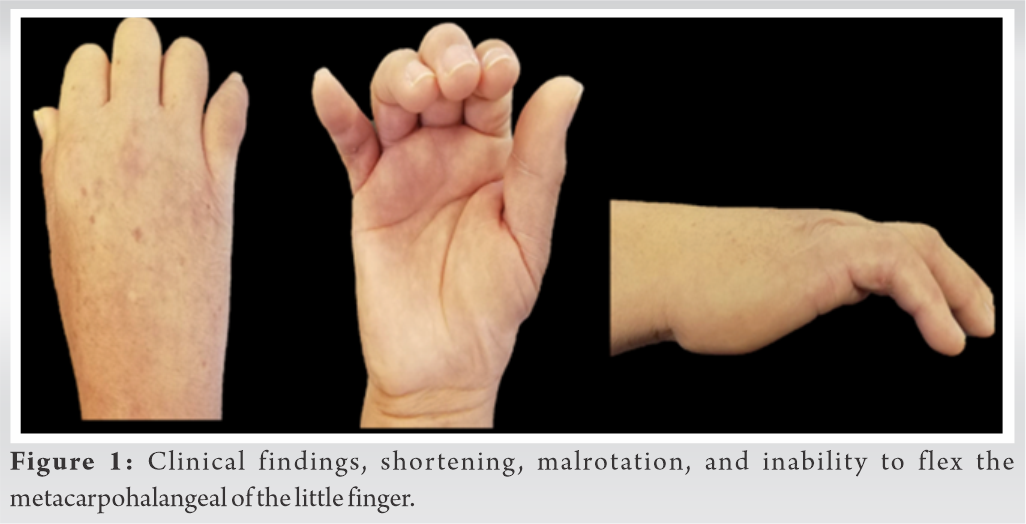
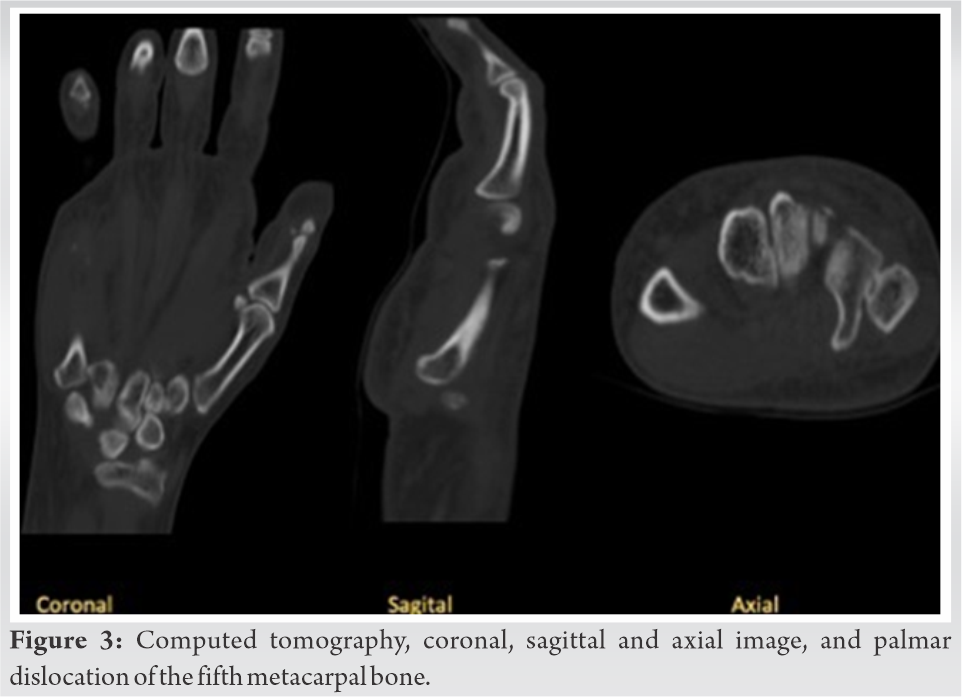
A 50-year-old, right-handed, female housekeeper presented trauma to the right hand as a result of a motorcycle accident. An initial diagnosis of proximal interphalangeal dislocation of the fifth finger was made, which was reduced and immobilized with dynamic finger splint (Fig. 1). X-ray of the hand was taken (Fig. 2), which shows a shortening of the fifth metacarpal, an alteration of the cascade of the metacarpal lines, a disruption of the M line, a loss of the relationship between the base of the fifth metacarpal with the hamate toward the ulnar aspect, and an overlapping of the base of the fifth metacarpal with the hamate. 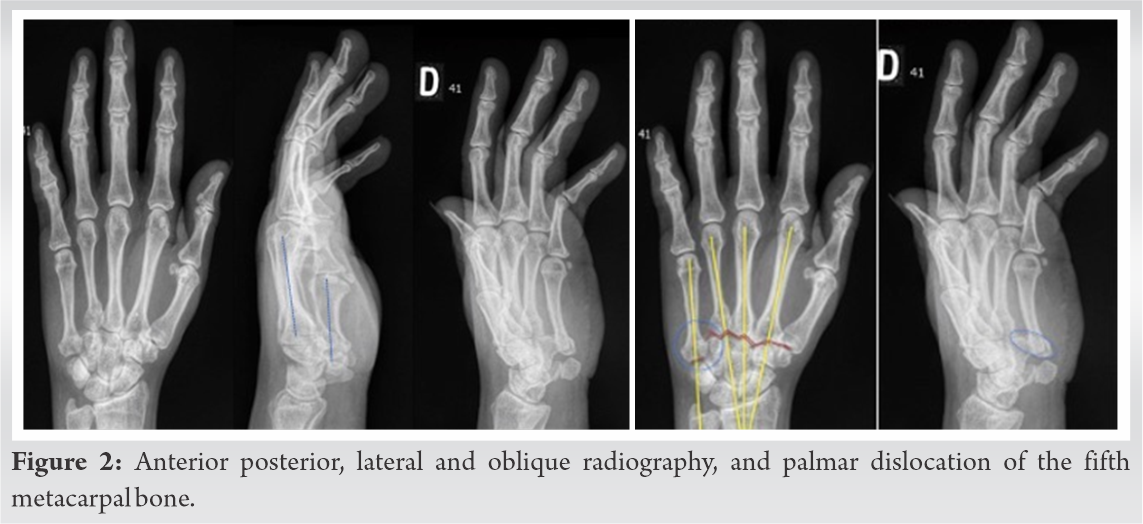
As treatment, the patient was taken to an open reduction and internal fixation. A dorsoulnar approach of the wrist was performed. Fibrous tissue was observed at the level of the articular surface which was removed. Reduction of the luxation was performed, an adequate carpometacarpal reduction was verified under direct vision and fluoroscopy, and the fifth metacarpal was fixed to the fourth metacarpal with a Kirschner wire placed transversely to the axis of the metacarpal. The intermetacarpal ligament and the carpometacarpal ligament were pulled out, without the possibility of repair. The fixation was done with an internal brace (Arthrex, Naples FL) fixed at the base of the fifth metacarpal, the base of the fourth metacarpal and the hamate, achieving an adequate restitution of the articular relationship between the fifth metacarpal and the hamate, and an ulnar gutter was placed (Fig. 4).
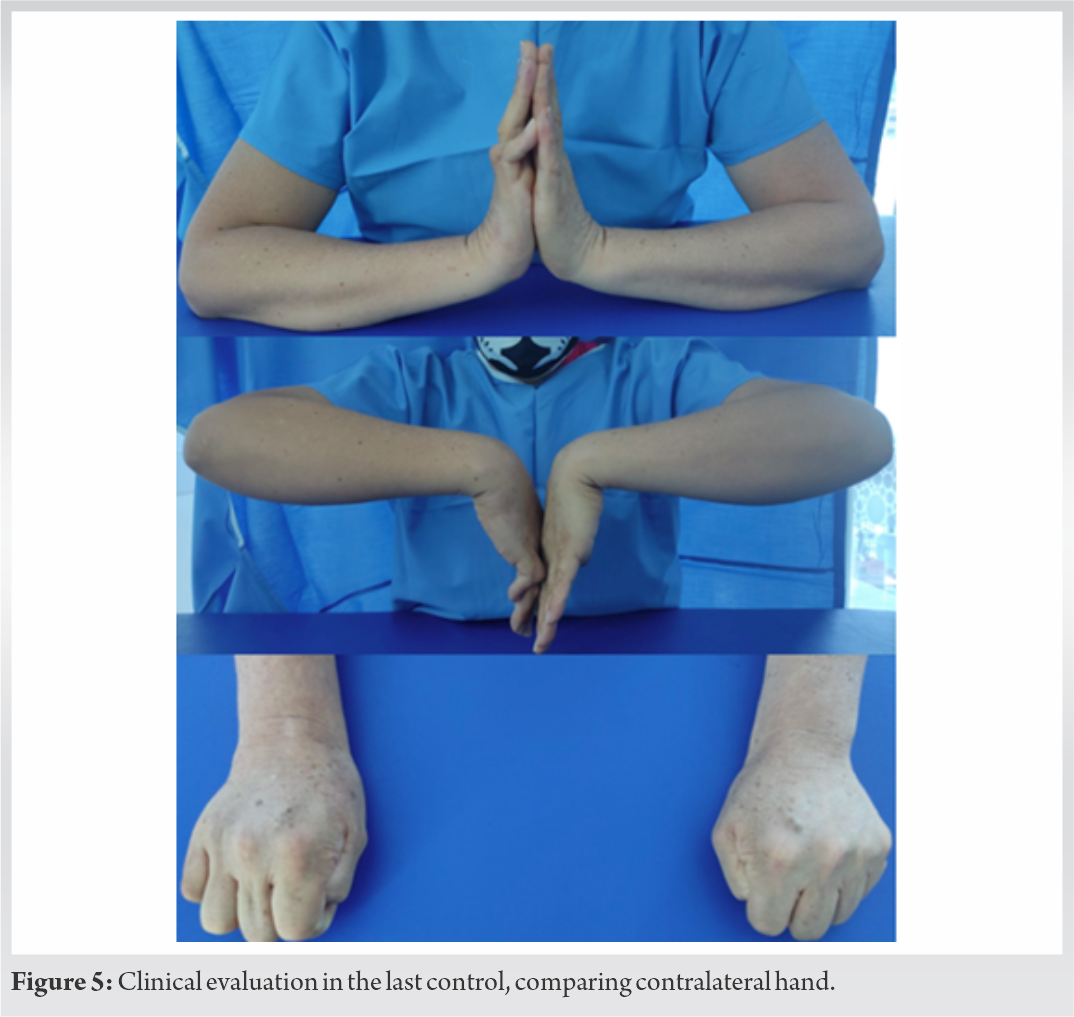
Postoperatively, the patient was left with a splint for 4 weeks, followed by a brace. At the 8th week, the pin was removed. There was no sign of infection, the patient with a less pain. At the 4th week, rehabilitation was started, and by the 6th week, the patient was without pain and with adequate tolerance to physical therapy, though the range of motion of the metacarpophalangeal joints of all fingers was limited; the little finger showed passive flexion of 30°, and extension 20° 9 weeks after surgery, the patient was asked to start using the hand for daily activities. At this time, the small finger had full passive and active extension of the metacarpophalangeal joint, proximal interphalangeal joint extension of 30° and flexion of 100°, and the middle and distal interphalangeal joints without limitation; however, a boutonniere deformity was observed in the small finger, for which a joint jack splint was indicated. At 28 weeks after surgery, the patient was pain free, was using the joint Jack splint at night, and performing her daily life activities. QUICKDASH 6.8, MAYO WS 100, she had grip strength in the right hand of 20 Newtons and left hand 28 Newtons. The little finger had a deformity in flexion of the proximal interphalangeal, the active flexion at the metacarpophalangeal level was 45°, and she was able to perform full extension, the proximal interphalangeal achieving a maximum flexion of 100°, and active extension of 64° (Fig. 5).
Carpometacarpal fracture-dislocations are usually produced by high energy. Nalebuff [5], in 1968, classifying the injury in ulnopalmar or radiopalmar, which would have repercussions in the ligamentary compromise and probably in the stability of the lesion, the radiopalmar carpometacarpal dislocations being the most unstable due to the compromise of the intermetacarpal ligament, carpometacarpal ligament, and the pisometacarpal ligament, unlike the ulnopalmar, where the pisometacarpal ligament remains intact [5, 6, 7]. The flexor carpi ulnaris plays an important role as a deforming force toward palmar and ulnar, when performing traction of the pisometacarpal ligament [1, 8] a concept that should be considered when reducing the dislocation.
The carpometacarpal dislocations of the small finger and ring finger can be associated to lesions of the motor or sensory branch of the ulnar nerve [9] and to carpal fractures, the hook of the hamate being the most frequent [10]. Stress X-rays have been reported, where distraction and compression maneuvers are performed on the joint looking to subluxate or dislocate it, identifying this finding in the radiography [7].
The first reports of carpometacarpal dislocations were made in 1918 by McWhorter, 1934 by Buzby, and in 1936 by Robert [4, 11]; however, the literature of ulnopalmar carpometacarpal dislocation is still scarce, being mostly case reports, including 17 case reports with a total of 23 carpometacarpal to palmar luxation which was found in the literature [1, 2, 4, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17].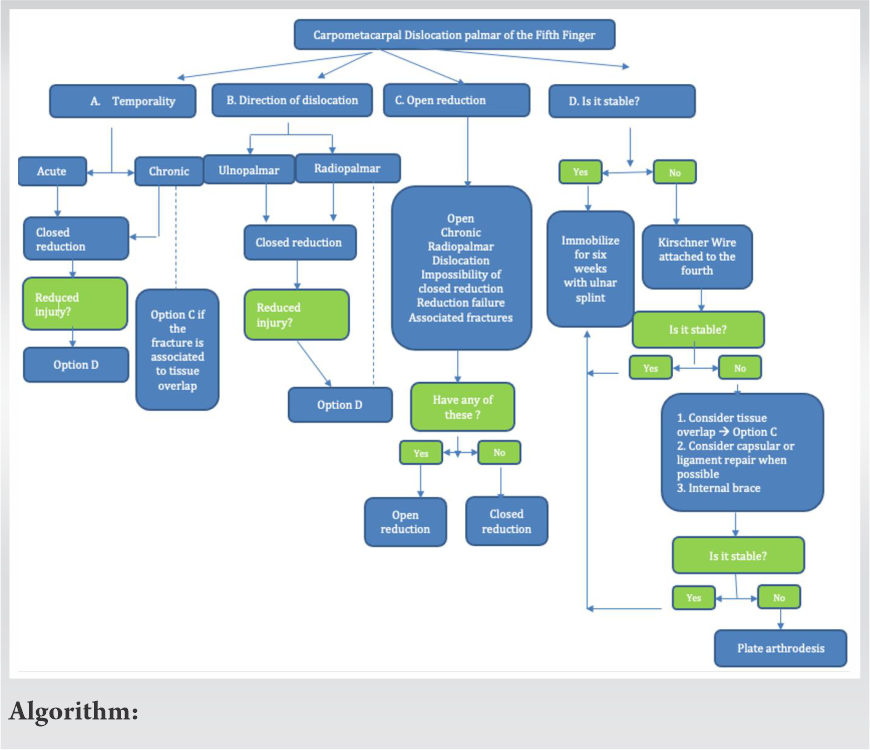
The literature agrees that the later the treatment, the more likely, it is that an open reduction will be required, repairing the capsule, and using pins to support the reduction [1, 2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17].
The reduction of these injury can be maintained with K-wire, using from one to four, fixing the fifth metacarpal to the fourth metacarpal and/or the hamate, which is usually removed between 4 and 6 weeks [1, 2, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17]. Another treatment option is the use of an internal brace (Arthrex, Naples FL); in case, it is not possible to repair the capsule and ligaments, as was the case with this patient. Suspension arthroplasty has been described in fracture dislocation of the fifth metacarpal; in cases, where the patient persists with disabling pain associated with degenerative changes at the level of the carpometacarpal joint of the fifth finger, using the extensor carpi ulnaris and passing it through bony tunnels through the fifth and fourth metacarpal to fix it to the extensor carpi radialis brevis [16]. In the case of this patient of this report, no capsule or ligament repair was performed, since these had been replaced by fibrous tissue, so the internal brace was placed, seeking to replace the function of the injured ligaments that are inserted at the base of the fifth finger.
The authors propose a treatment algorithm for isolated dislocations of the carpometacarpal joint of the fifth finger to the palmar that is not diagnosed and treated early, in the first 10 days (Algorithm).
Isolated palmar carpometacarpal dislocation of the small finger is infrequent and often goes unnoticed. The physical examination and the Figs allow to guide the treatment that can be from closed or open reduction, with or without internal fixation, which depends in part on the reduction and the stability of the joint, with speedy treatment affecting the need for an open reduction. Using this algorithm, the surgeon will have a vision of the probable best treatment option.
Isolated palmar carpometacarpal dislocation of the small finger is infrequent, and currently, we do not know algorithms reported in the literature on isolated dislocations of the carpometacarpal joint of the fifth finger to the palmar that is not diagnosed and treated early.
References
- 1.Ibn El Kadi K, Sbiyaa M, Alami B, Rabhi I, Marzouki A, Lahrach K, et al. Isolated radial volar dislocation of the fifth carpometacarpal joint: A rare injury. Pan Afr Med J 2013;16:90. [Google Scholar]
- 2.Wright AC, Muir L. A review of published radiographic indicators of carpometacarpal dislocation including their application to volar dislocations through a case study. J Emerg Med 2015;49:e69-71. [Google Scholar]
- 3.Cooney WP, Linscheid RL. Fractures and dislocations of the wrist and hand, then and now. J Hand Surg 1983;8:687-90. [Google Scholar]
- 4.Ker HR. Dislocation of the fifth carpo-metacarpal joint. J Bone Joint Surg 1955;37:254-6. [Google Scholar]
- 5.Nalebuff E. Isolated anterior carpometacarpal dislocation of the fifth finger. J Trauma 1968;8:1119-23. [Google Scholar]
- 6.Beekhuizen S, de Witte PB, Rutgers M, Ohanis D. Isolated ulnopalmar dislocation of the fifth carpometacarpal joint. BMJ Case Rep 2018;2018:bcr2018225363. [Google Scholar]
- 7.Yamakado K, Hashimoto F, Nagata S, Higuchi M. Isolated palmar dislocation of the fifth carpometacarpal joint diagnosed by stress X-rays. Arch Orthop Trauma Surg 2000;120:529-30. [Google Scholar]
- 8.Lefere M, Dallaudière B, Omoumi P, Cyteval C, Larbi A. Rare carpometacarpal dislocations. Orthop Traumatol 2016;102:813-6. [Google Scholar]
- 9.Domingo A, Font L, Saz L, Arandes JM. Isolated radial palmar dislocation of the fifth carpometacarpal joint with ulnar neuropathy associated: Successful treatment with closed reduction and internal fixation. Eur J Orthop Surg Traumatol 2009;19:101-7. [Google Scholar]
- 10.Xiao RC, Stenquist DS, Dyer GS. Volar Dislocation of the Fifth Carpometacarpal Joint Mistaken for Radial Collateral Ligament Injury; 2019. [Google Scholar]
- 11.Roberts N, Holland CT. Isolated Dislocation of the Base of the Fifth Metacarpal; . [Google Scholar]
- 12.Dennyson WG, Stother IG, Summary E. Carpometacarpal dislocation of the little finger. Hand 1976;8:161-4. [Google Scholar]
- 13.Saleemi AJ, Iqbal MJ. Ulnar dislocation of fifth carpometacarpal joint. Hand Surg 2005;10:87-90. [Google Scholar]
- 14.Nakayama M, Horiuchi Y, Kawashima H. Isolated volar dislocation of the fifth carpometacarpal joint: A case report. Hand Surg 2007;12:165-8. [Google Scholar]
- 15.Fischer MW. Ulnopalmar Dislocation of the Fifth Carpometacarpal Joint. A Rare Injury Case Report. Vol. 68; 2002. Available from: https://www.researchgate.net/publication/11322648 [Google Scholar]
- 16.Akmaz I. Delayed diagnosis of isolated ulnopalmar dislocati. Acta Orthop Traumatol Turcica 2004;38:361-5. [Google Scholar]
- 17.Hegde AS. Isolated radiopalmar dislocation of fifth carpometacarpal joint: A rare presentation. Am J Orthop 2015;44:E347-9. [Google Scholar]