Osteoid osteoma of the lumbar spine may present as a scoliotic deformity which gradually resolves once the osteoid osteoma is treated without usually requiring any further management for the scoliosis.
Dr. Kapil Lalwani, Department of Orthopaedics, MGM Hospital and Medical College, Aurangabad, Aurangabad, Maharashtra, India. E-mail: kapillalwani@hotmail.com
Introduction:Osteoid osteoma is a benign bone tumor. It characteristically presents with pain which increases in severity at night. Low back ache is a very common complaint which is relatively less common in the pediatric population. The patients are initially treated for a prolonged period of time by primary physicians with analgesics only after which they are referred to tertiary centers. These young patients can also develop secondary scoliosis which may become the primary concern of the parents and treating primary physician.
Case Report:An 8-year-old girl presented to us with chief complaints of low back ache for 1 year and back deformity for 3–4 months. She was treated initially by a primary physician with non-steroidal anti-inflammatory drugs. There was a significant reduction in her back pain with medications. The patient was further radiologically evaluated once she developed a back deformity which reported a lesion involving the posterior elements of the L3 vertebra (? Osteoid osteoma). For this, open excision with curettage was preferred over radiofrequency ablation due to its location. The patient subsequently had good pain relief and the deformity got corrected for 3 months.
Conclusion:Radiofrequency ablation or surgical excision with curettage of osteoid osteoma is required as prolonged analgesic medication has its own side effects. Once the pain subsides, the paraspinal muscle spasm reduces and the scoliosis gradually corrects.
Keywords: Osteoid osteoma, lumbar spine, spinal tumor, excision, scoliosis.
Osteoid osteoma is a rare benign bone tumor comprising 5% of all bone tumors and 11% of all benign bone tumors [1]. It is neither locally aggressive nor does it have the potential for malignant transformation. It more commonly affects the long bones and, in 10% of the cases, it involves the spine [2]. Within the spine, it most commonly involves the lumbar region followed by the cervical, the thoracic, and lastly the sacrum [3]. The common age group affected is from 5 to 25 years and the male-to-female ratio is 3:1 [4, 5]. It usually measures less than 2 cm containing a nidus of vascular osteoid which is surrounded by sclerotic bone. It is a painful condition with pain increasing at night which significantly reduces by non-steroidal anti-inflammatory drugs (NSAIDS). The cause of scoliosis is chronic muscle spasm due to pain and inflammatory reactions around the tumor [6]. The cause of the pain is the release of prostaglandins with levels as high as 100–1000 times that of the normal bones [7]. Many a times, the deformity becomes the primary center of focus for treating doctors.
An 8-year-old girl presented to us with the chief complaints of having low back ache for 1 year which was gradually increasing in magnitude. The pain was more severe at night and did not relieve on rest. The pain was significantly reduced with NSAIDS prescribed by primary treating doctors. The pain was localized to the lower back region without radiculopathy. The relatives noticed her back deformity 4 months back, as shown in (Fig. 1). The deformity progressed slowly to present magnitude for 4 months. They had been to multiple practitioners for pain, but were concerned once they noticed the deformity. She was referred to our center for scoliotic deformity correction surgery. An X-ray was advised as the primary modality which showed a scoliotic deformity, as seen in (Fig. 2).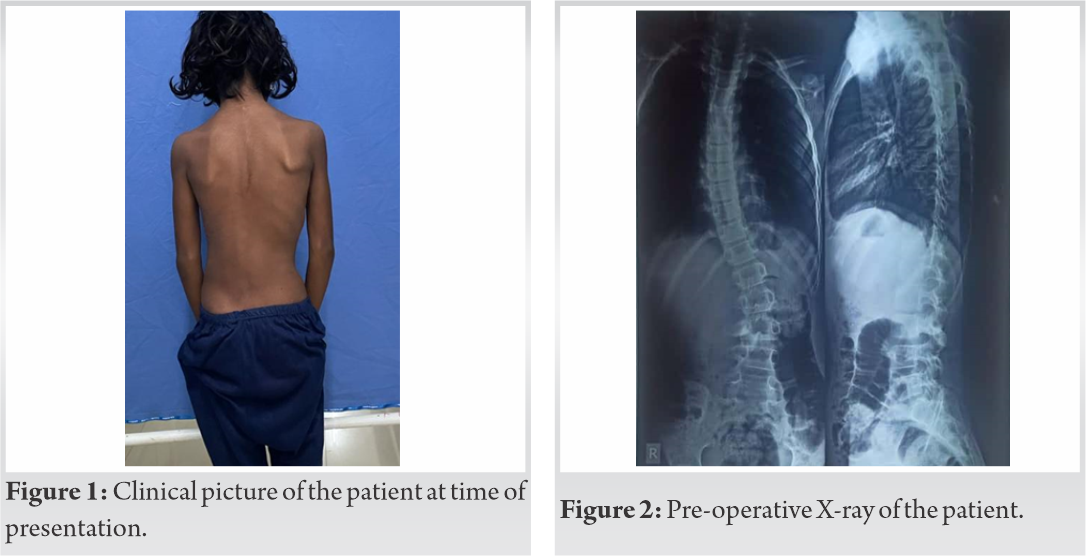
Her pre-operative cobb’s angle at level D4-D11 was 29° and at D12-L4 was 34°. Followed by this, a magnetic resonance imaging (MRI) was advised, which reported the presence of a tumor on the right side of the posterior elements of the L3 vertebra just above the inferior articular facet mostly pointing toward osteoid osteoma. Computed tomography (CT) scan was next advised to know the exact size and location of the tumor. It was reported to be ?osteoid osteoma measuring 10 × 9 mm with the nidus located in the right lamina just above the inferior articular facet and the surrounding sclerosis involving the right lamina and pedicle communicating with the spinal canal and the lateral recess, as seen in (Fig. 3).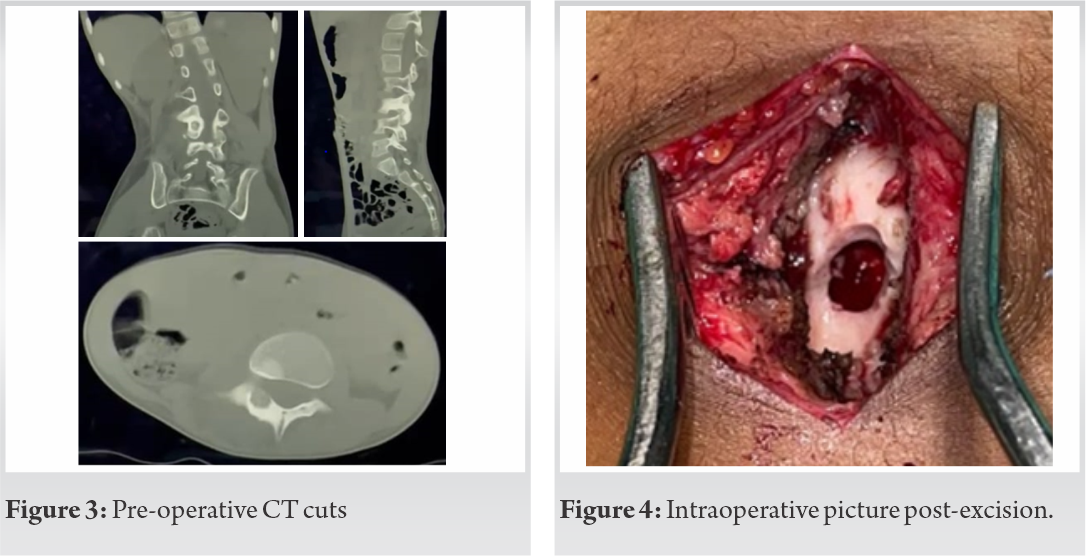
The patient would have been considered for the radiofrequency ablation of the tumor, but due to its location and extremely close proximity to the nerve roots, it was decided to opt for open excision.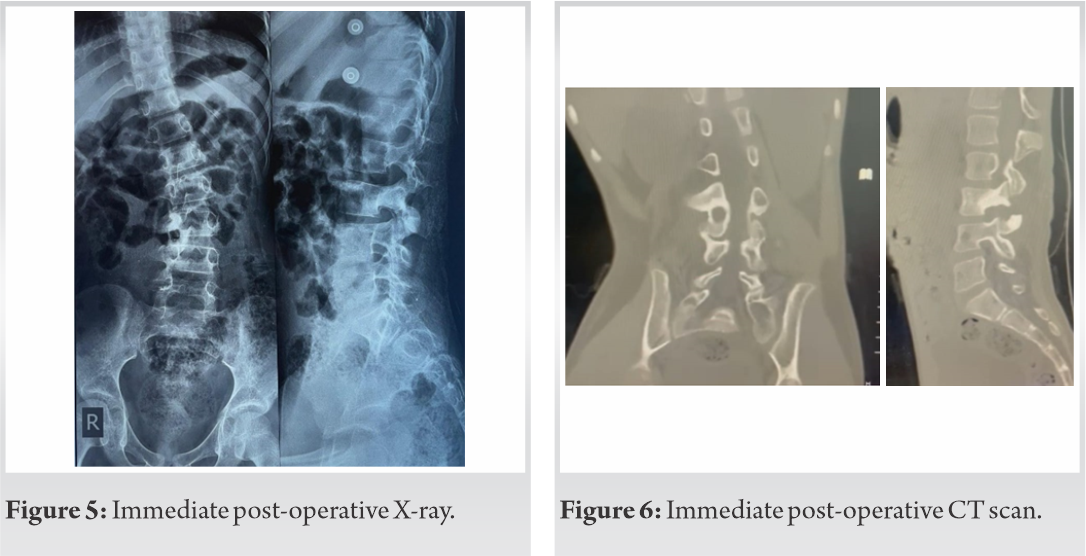
The patient was taken on the operating table under general anesthesia in prone position. Using a posterior midline incision, the right lamina of L3 vertebra was exposed preserving the midline structures. A high speed 3 mm Stryker diamond burr was used to remove the posterior part of lamina present over the tumor. Special precaution was taken to preserve the capsule, inferior articular process, and the facet joint along with a part of pars intercularis so as to not compromise the segmental stability between L3 and L4 vertebra. The affected area appeared dark brown in color. The contents were curetted out until healthy bone texture is shown in (Fig. 4). Closure was done in layers and the tissue obtained was sent for histopathological examination which confirmed it to be an osteoid osteoma. Postoperatively, an X-ray and CT scan were done which showed the area excised, as seen in (Fig. 5, 6), respectively. The patient was mobilized from the 1st post-operative day itself. On her 2nd week follow-up, there was significant reduction of pain without the use of NSAIDS. At her 3rd month follow-up, a check X-ray was done, which showed significant straightening and reduction of the scoliotic deformity, as seen in (Fig. 7) which was also clinically appreciated, as seen in (Fig. 8). Three months postoperatively, the cobb’s angle at D4-D11 level was 12.2° (which preoperatively was 29°) and at D12-L4 level was 19° (which preoperatively was 34°).
Osteoid osteoma of the lumbar vertebra in a child may present as scoliosis due to muscular spasm. The challenge is faced in both diagnosing as well as treating it. The average time for establishment of confirmed diagnosis is 15–20 months [8]. Only complete excision of the tumor ensures least risk of recurrence. Presently, CT-guided radiofrequency ablation provides a minimally invasive method and is the treatment of choice having a success rate of 90% [7] and is gaining popularity internationally for extraspinal tumors [9]. It has two limitations, first being the availability and second being the risk of injuring a nerve root if the osteoid osteoma lies in close proximity to it. The recommended safe margin for radiofrequency ablation is 1.5 cm from nerve roots and 1 cm from skin [10] which was not fulfilled in this case. Hence, in our case, we performed open excision and curettage under microscope.
A child having a long history of low backache which is not relieved on rest but relieved quite significantly on medication should arise the doubt of osteoid osteoma. X-ray can be the primary investigation, but MRI scan is the investigation of choice to diagnose any soft-tissue pathology. CT scan is done for pre-operative planning which shows the precise location and size of the lesion. Open excision provides an effective treatment without risking the surrounding structures and without compromising the posterior stability. Spinal osteoid oteoma can present with scoliosis also due to muscle spasm as a result of severe pain. Excision of tumor leads to gradual correction of scoliotic deformity too for 3–6 months.
Open excision and curettage are an effective and safe method for managing osteoid osteoma of the spine occurring in close proximity to the neural structures and the secondary scoliotic deformity associated with it, because as the pain gradually resolves, the scoliotic deformity subsides as well.
References
- 1.Kitsoulis P, Mantellos G, Vlychou M. Osteoid osteoma. Acta Orthop Belg 2006;72:119-25. [Google Scholar]
- 2.Ghanem I. The management of osteoid osteoma: Updates and controversies. Curr Opin Pediatr 2006;18:36-41. [Google Scholar]
- 3.Etemadifar MR, Hadi A. Clinical findings and results of surgical resection in 19 cases of spinal osteoid osteoma. Asian Spine J 2015;9:386-93. [Google Scholar]
- 4.Kumar R, Chandrashekhar N, Dasan JB, Ashok S, Rastogi S, Gupta V, et al. Recurrent osteoid osteoma: A case report with imaging features. Clin Imaging 2003;27:269-72. [Google Scholar]
- 5.Gökalp MA, Gözen A, Ünsal SŞ, Önder H, Güner S. An alternative surgical method for treatment of osteoid osteoma. Med Sci Monit 2016;22:580-6. [Google Scholar]
- 6.Akbarnia BA, Rooholamini SA. Scoliosis caused by benign osteoblastoma of the thoracic or lumbar spine. J Bone Joint Surg Am 1981;63:1146-55. [Google Scholar]
- 7.Nebreda CL, Vallejo R, Mayoral-Rojals V, Ojeda A. Osteoid osteoma: Benign osteoblastic tumor of the lumbar L4 transverse process associated with radicular pain: A case report. Pain Pract 2017;18:118-22. [Google Scholar]
- 8.Laurence N, Epelman M, Markowitz RI, Jaimes C, Jaramillo D, Chauvin NA. Osteoid osteomas: A pain in the night diagnosis. Pediatr Radiol 2012;42:1490-501. [Google Scholar]
- 9.Gasbarrini A, Cappuccio M, Bandiera S, Amendola L, van Urk P, Boriani S. Osteoid osteoma of the mobile spine: Surgical outcomes in 81 patients. Spine (Phila Pa 1976) 2011;36:2089-93. [Google Scholar]
- 10.Houdek MT, Wenger DE, Sherman CE, Turner NS. Osteoid osteomas of the foot and ankle: A study of patients over a 20-year period. Am J Orthop (Belle Mead NJ) 2014;43:552-6. [Google Scholar]








