A single intramedullary implant is a better choice for double segmental fractures.
Dr. Harmeet Kaur, Department of Radiodiagnosis, All India Institute of Medical Sciences, Bathinda, Punjab, India. E-mail: kaurh28@yahoo.com
Introduction:A “double segmental” fracture is an injury pattern that has three fracture sites and four fracture segments in a single bone. It is extremely rare, with only three “Double segmental femoral fracture” and only four “double segmental tibia fracture” cases reported in the literature. These fractures are associated with difficulty in deciding the implant for fixation, segment reduction, maintenance of reduction, maintaining blood supply of segment during fixation, and the high risk of post-operative complications.
Case Report:We present two unique cases, one of “double segmental femur fracture” and the other of “double segmental tibia fracture,” fixed with intramedullary nailing. When Schanz screw or Steinman pins were used to reduce the intermediate fragments and hold them in place, they interfered with the reaming due to the protruding part in the narrow canal. This problem could be solved using weber clamps to hold reduction as they do not obscure the canal. All the fractures united uneventfully at 9 months follow-up.
Conclusion: A “single intramedullary device” to fix “all the segments” can help provide stabilization without compromising soft-tissue attachments and viability of the intermediate fracture segments in “double segmental” fractures.
Keywords: Double segmental fracture, intramedullary nailing, trifocal fracture, femur, tibia, fracture.
“Double segmental” fractures are unique as there are three fracture segments, two individual intermediate fracture segments, each surrounded by at least two fracture lines, between the proximal and distal fragments. These fracture segments have their own cortex and medullary cavity, along with blood supply from surrounding soft-tissue attachments, making them true segments [1]. Thus, they differ from “trifocal fractures,” in which the intermediate fragments may not be complete segments.
These fractures are associated with difficulty in deciding the implant for fixation, segment reduction, maintenance of reduction, maintaining blood supply of segment during fixation, and the high risk of post-operative complications.
We present two cases, one each of femur and tibia, and their subsequent management technique.
Case 1
A 63-year-old male presented to emergency with a history of a road traffic accident, in which the patient was riding pillion and was struck by a car moving at high velocity. After emergency stabilization and application of skeletal traction in the trauma bay, he was transferred to the orthopedic unit. The radiographs revealed a “double segmental” fracture of the right femur with no other associated injuries (Fig. 1a-d). The patient was taken up for intramedullary fixation with a cephalomedullary nail the next day. Initially, we tried using Schanz screw to reduce the intermediate fragments and hold them in place, but they interfered with the reaming due to the protruding part in the narrow canal. Subsequently, weber clamps were used on the proximal and intermediate fragments to correct their respective displacements and hold the fracture fragments in reduced positions. The use of a polar screw helped in centering the guidewire in the distal fragment.
The patient was mobilized with toe-touch weight-bearing on the affected limb from the 3rd day to 4 weeks. After 4 weeks, the patient was allowed weight-bearing as tolerated. All the fractures united uneventfully at 9 months follow-up with good hip and knee range of motion.
Case 2
A 60-year-old female presented to us after a road traffic accident. She was a rear seat passenger in a car that hit another car moving at a high velocity. The patient suffered blunt trauma to the left side of the chest with a rib fracture and hemothorax, along with injury to her right leg. A chest tube was placed, the leg splinted and elevated over a Bohler-Braun splint. The radiographs revealed that she had a “double segmental” fracture of the right tibia and segmental fracture of the fibula (Fig. 2a-d). The patient was taken up for closed intramedullary nailing of the tibia after 15 days when her condition stabilized. Meticulous entry was made with particular emphasis to avoid flexion and valgus deformity. The reduction was maintained using a Schanz screw in the proximal fragment and weber clamps on the intermediate and distal fragments. Post-operatively, a splint was applied for 2 weeks till suture removal.
She was kept on toe-touch weight-bearing walking till 6 weeks and from there onward on weight-bearing as tolerated. She was followed up monthly for 3 months. Unfortunately, the patient was lost to follow-up after that due to the ongoing COVID pandemic.
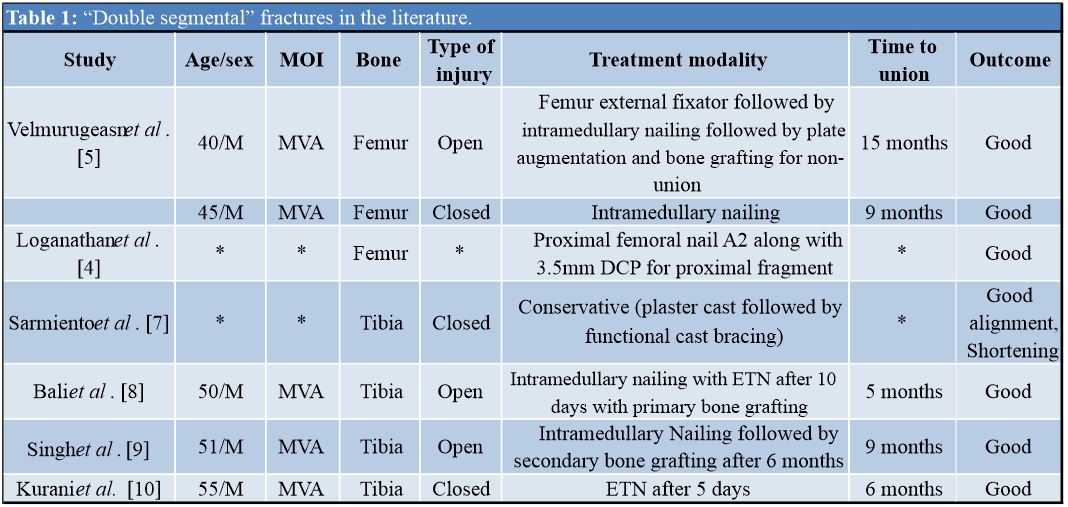
“Double segmental” fractures are extremely rare, with only three femoral cases reported in the literature [2, 3, 4], and there are a total of four reported cases of double segmental tibia fracture [5, 6, 7, 8] (Table 1).
These fracture patterns are depictive of severe mechanisms of injury. A direct blow to bone at three different sites simultaneously or the phenomenon of direct and indirect injury, wherein two direct forces exerted at the bone are countered by a third indirect force that acts as a fulcrum between the forces, further leading to segmentation of the large intermediate segment [6].
A significant challenge in all such cases is the choice of implant for internal fixation. An extramedullary implant can help in easier and anatomical reduction through open reduction of the fractured fragments. However, it leads to excessive soft-tissue dissection, subsequently compromising bone vascularity and leading to an excessive stress riser at the junction of the plates [1].
These issues can be addressed using an intramedullary implant [1, 2, 4, 7, 8]. Furthermore, separate versus single implants have been debated in the literature.
Arastu et al., in their cadaveric study, found that reaming was a major risk factor for rotational displacement and subsequent devascularization, with long segments rotating more than shorter segments. They strongly recommended clamping the fracture fragments during reaming [9]. This technical issue is more pronounced in double segmental fractures due to the existence of 2 intermediate fragments, which both need to be held individually.
It can be managed using Schanz screw, Steinmann pins, Weber clamps, Farabeuf clamp, and reduction forceps through mini-open incisions and temporary unicortical plating to reduce fracture fragments and maintain reduction during reaming and insertion of nail [9, 10].
The problem of the prominence of Schanz screws, Steinmann pins into the medullary canal leading to further obliteration of a narrow canal may arise, as was the case in our patients. This can be avoided using weber clamps to hold reduction as they do not obscure the canal.
There are higher chances of malunion and non-union between the various fragments, in which union happens at one or two sites. Non-union can be managed using bone grafting with plate augmentation or revision nailing. Primary and secondary bone grafting has been used in three of the reported cases, with union achieved in all cases.
The primary use of Ilizarov for tibial segmental fractures has also been described in the literature, but the authors believe that it may be better used as a secondary procedure in case of septic and gap non-union.
Skillful reduction, minimal soft-tissue disruption, maintaining the vascularity of intermediate segments, and meticulous post-operative care form the cornerstone to successfully treating these complicated injuries. Single implant in form of an intramedullary nail has given desired results in our patients.
The choice of the implant in “segmental” fractures has been debated for long. Intramedullary versus extramedullary, as well as, single versus separate implant, for each fracture segment, have been suggested. The situation becomes even more tricky in “double segmental” fractures. The use of weber clamps to hold the intermediate segments during reaming prevents their rotation and maintains vascularity. Single implant in form of an intramedullary nail can give desired results even in “double segmental” fractures if done skillfully.
References
- 1.Howe TS. Double level fractures of the femur treated with closed intramedullary nailing. Ann Acad Med Singap 1998;27:188-91. [Google Scholar]
- 2.Loganathan S, Thiyagarajan U. Multilevel segmental femur fracture in young individuals treated by a single step-all in one intramedullary device-a prospective study. Biomedicine 2020;40:488-91. [Google Scholar]
- 3.Velmurugeasn D, Prasad VD, Dheenadhayalan J, Rajasekaran S. Double segmental femur fracture: Two case reports with a technical note and perioperative illustration. Int J Orthop Sci 2020;6:618-21. [Google Scholar]
- 4.AnilBabu P, Sudhakar K, VenkateswaraRao D, RajaSekhar P. A prospective study on segmental fractures of femur treated with inter Lockingnails. IOSR J Dent Med Sci 2020;19:47-50. [Google Scholar]
- 5.Sarmiento A, Latta LL. The Nonsurgical Treatment of Fractures in Contemporary Orthopedics. 1st ed. United States: McGraw Hill Education; 2011. [Google Scholar]
- 6.Bali K, Kumar V, Patel S, Aggarwal S. Double segmental tibial fractures--an unusual fracture pattern. Chin J Traumatol 2011;14:247-9. [Google Scholar]
- 7.Singh D, Awasthi B, Padha V, Negi V. Double segmental tibial fracture: Case report with review of literature. J Case Rep 2016;6:243-6. [Google Scholar]
- 8.Kurani MM, Sanikop ST, Patil MY, Ingalagi AA. Double segmental tibial fracture-a rare case report. Int J Orthop Sci 2017;3:1129-31. [Google Scholar]
- 9.Sohn HS, Chung JY, Song HK. Analysis of complications and clinical outcomes in the treatment of segmental tibial fractures according to the method of internal fixation. Asian J Surg 2019;42:740-5. [Google Scholar]
- 10.Zheng ZL, Yu X, Xu GQ, Chen W, Zhang YZ, Jiao ZQ. Four pins assisted reduction of complex segmental femoral fractures: A technique for closed reduction (in Chinese). J Huazhong Univ Sci Technol Med Sci 2014;34:912-6. [Google Scholar]