TresLock is a new device and shows good anatomical compatibility for femurs.
Dr. Takafumi Hiranaka, Department of Orthopedic Surgery and Joint Surgery Center, Takatsuki General Hospital, Takatsuki-City, Osaka, Japan. E-mail: takafumi.hiranaka@gmail.com
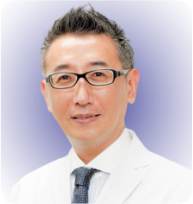
Introduction: A new device, TresLock (KISCO DIR Co., Ltd., Kobe), has been used for the treatment of unstable proximal femoral fractures and was designed based on Japanese anatomical characteristics. It has three sliding hip screws with one side plate. The angle of all screws relative to the plate has been set to 128°, and each hip screw has a short thread (15 mm) to prevent crossing of the fracture line. In this study, we evaluated the morphological compatibility of TresLock.
Methods:We treated 10 patients with hip fractures using TresLock at our institution between September 2016 and December 2017. The average age of the patients was 83.8 years (range, 73–93 years). Fractures included five proximal neck transcervical shear fractures (Orthopaedic Trauma Association [OTA] type-31B2.3, Pauwels III) and five basicervical fractures (OTA type-31B3). The clinical course and three-dimensional computed tomography were evaluated postoperatively.
Results:In all cases, all three screws were inserted within the femoral neck. The screws were inserted at an axis of 2.5 ± 1.3° varus to the femoral neck axis. The distance from the subcapital line to the three (proximal-anterior, proximal-posterior, and distal) screw thread ends was 12.0 ± 1.8 mm, 10.4 ± 2.4 mm, and 11.6 ± 4.0 mm, respectively and was sufficient to actuate compression force. However, one case (Pauwels III) required reoperation because of non-union.
Conclusion:Careful follow-up is needed, but TresLock shows good anatomical compatibility for femurs among the Japanese population.
Keywords:Proximal femoral fracture, basicervical fracture, internal fixation device.
There are many options when surgically treating proximal femoral fractures, such as cannulated cancellous hip screws [1] or Hansson pins [2]. However, secondary displacement of the femoral head can occur postoperatively, especially in cases of unstable fractures. Recently, some implants, like the dual SC screw system (KISCO DIR Co., Ltd., Kobe), have a side plate to provide varus-resistant properties [3]. This implant is suitable for simple femoral neck fractures but does not provide sufficient stability for unstable fractures, including proximal neck transcervical shear fractures (Orthopaedic Trauma Association [OTA] type-31B2.3, Pauwels III) and basicervical fractures (OTA type-31B3). Although the treatment for these fractures is difficult and a gold-standard method has not been determined, a multiple-screw fixation within the limited femoral neck space is essential. However, there is no existing device that is designed based on morphological characteristics of the femoral neck. A new device, TresLock (KISCO DIR Co., Ltd., Kobe), was used for the treatment of unstable proximal femoral fractures. Nakanishi et al. examined the morphology of the proximal femur in the Japanese population and reported that the cross section of the femoral neck was asymmetric, with an average neck-shaft angle of 128° [4]. TresLock was designed based on these anatomical data. We hypothesized that TresLock had good compatibility because it was designed based on the anatomical characteristics of the Japanese population. This study aims to investigate this hypothesis by measuring post-operative three-dimensional CT imaging results.
Description of device
TresLock has three sliding hip screws with a side plate and their angle relative to the plate is set as 128°. The arrangement of hip screws is asymmetric, with proximal-anterior, proximal-posterior, and distal positions. The offset of the proximal-anterior screw was larger than the proximal-posterior screw to fit the medullary canal shape of the femoral neck. In addition, each hip screw had a short thread (15 mm) to prevent crossing the fracture line (Fig. 1).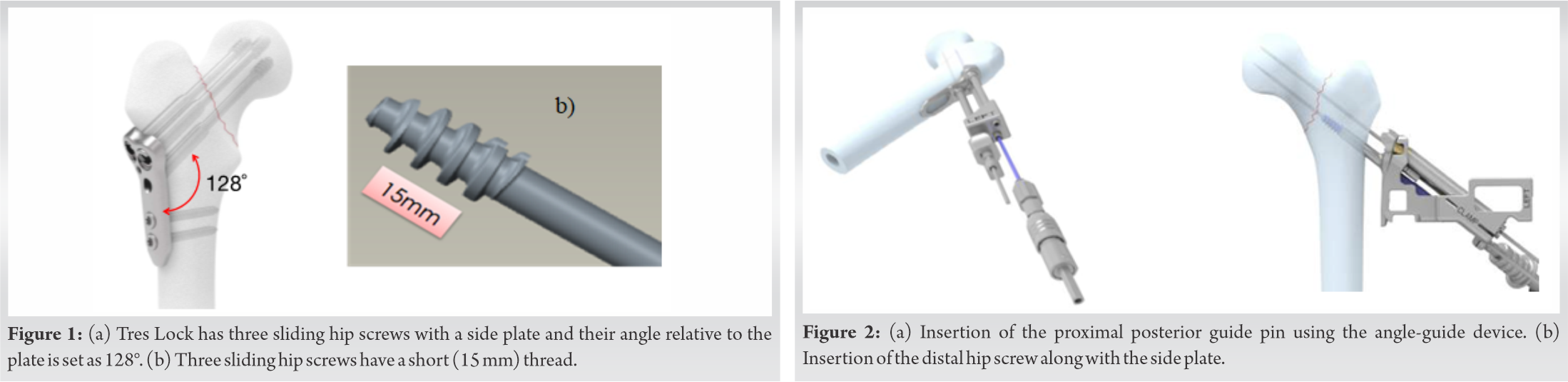
Between September 2016 and December 2017, 10 hip fractures in 10 patients were treated using TresLock in our institution. The patients included eight women and two men. The average age of the patients was 83.9 years (range, 73–93 years). Fractures included five proximal neck transcervical shear fractures (OTA type-31B2.3, Pauwels III) and five basicervical fractures (OTA type-31B3). Informed consent was obtained from all patients who participated in this study.
Operation procedures
After achieving reduction as anatomically as possible on the traction table, a distal guide pin was inserted just above the calcar femorale and a proximal posterior guide pin was inserted using the angle-guide device (Fig. 2a). The pins were advanced to just under the subchondral bone. By measuring the length of the two guide pins, the size of the TresLock plate (side plate attached to the distal screw) and proximal posterior screw was selected. After reaming, the distal hip screw along with the side plate was inserted (Fig. 2b). Care was taken to set the plate parallel to the femoral shaft, and guide wires for the proximal posterior and proximal anterior screws were inserted through sleeves fixed on the plate. After insertion of the hip screws, two distal locking cortical screws were inserted to fix the plate on the femoral shaft.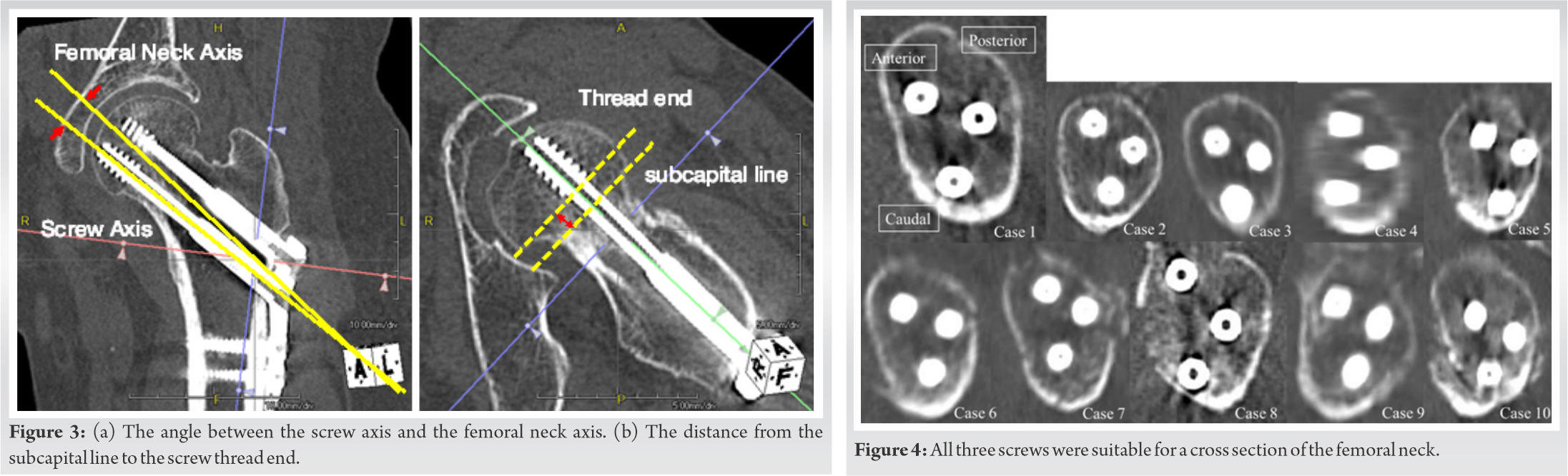
CT evaluation
A continuous full femoral bone CT scan was obtained in each patient using the Toshiba Aquilion ONE/Vision edition (Toshiba Medical Systems, Tochigi, Japan) with a slice thickness of 1 mm. Data were imported into picture archiving and communication system software (G7E Medical Systems Centricity Enterprise Web V3.0, Wisconsin, United States), and images were reconstructed using Aquarius Net Viewer V4.4.5.49 (TeraRecon, CA, USA) to analyze the desired slices.
We defined the following three evaluation items by creating standardized slices as previously reported [4]:
1. Screw positions
A slice perpendicular to the axis of the femoral neck at the narrowest level of the femoral neck was created and the positions of the three screws were evaluated.
2. Angle between screw axis and femoral neck axis
A coronal slice containing both the femoral axis and distal screw center was created and the angle between the screw axis and the femoral neck axis was measured (Fig. 3a).
3. Distance from the subcapital line to the screw thread end
An axial slice that intersected the femoral neck axis was created and the distance from the subcapital line connecting the upper and lower border of the femoral head to the screw thread of each of the three screws was measured (Fig. 3b).
Results
The detailed measurement results are shown in Table 1. In all cases, no screws were observed protruding from the femoral neck cortex and all three screws conformed to the femoral neck cross section (Fig. 4). The screw axis was set at 2.5 ± 1.3° varus inclination to the femoral neck axis. The screw direction was virtually parallel to the femoral neck axis. The distance from the subcapital line to the three (proximal-anterior, proximal-posterior, and distal) screw thread ends was 12.0 ± 1.8 mm, 10.4 ± 2.4 mm, and 11.6 ± 4.0 mm, respectively.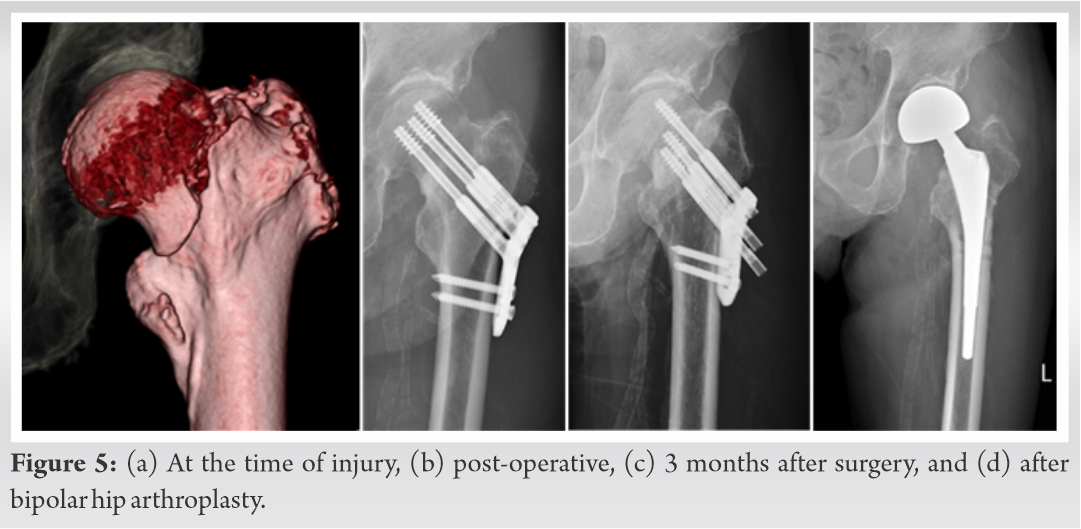
One case (Case 10) required reoperation. The patient was an 81-year-old man with a Pauwels III fracture. We had to remove the implant and perform hemiarthroplasty because of non-union 3 months after the primary operation (Fig. 5). The fracture union was obtained with neither secondary dislocation nor osteonecrosis in all but one case (Case 10).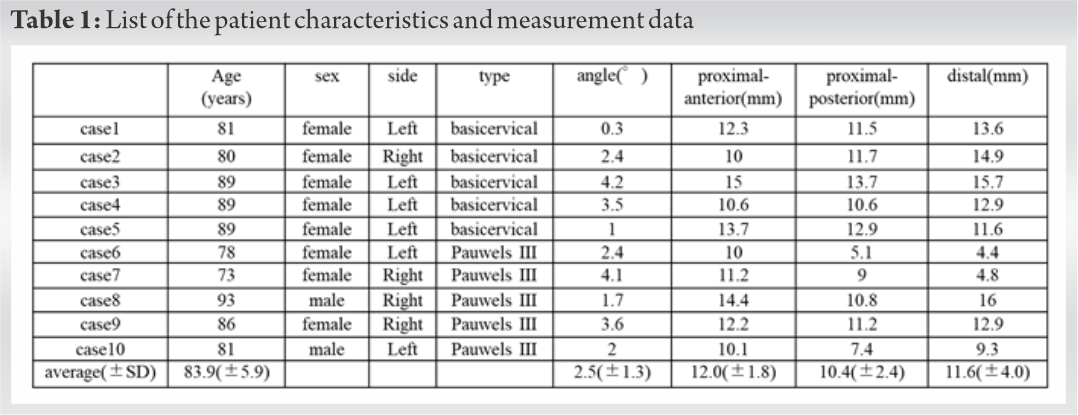
Our results demonstrate that the compatibility of hip screws in terms of both the arrangement of screws within the femoral neck cross section and the direction of screws corresponding to the femoral neck axis were excellent, as the hip screw angle should be parallel to the femoral neck axis. Despite that the anatomical neck-shaft angle in the Japanese population has been reported to be 125°–130° [5], the hip screw angle is set as 135° or greater in most devices with a side-plate. This angle is considered too steep, at least for Japanese patients. Regarding the TresLock, the hip screw angle is supposed to be parallel or slightly varus to the femoral neck axis in most cases. This is the first report to prove this clinically. In the cross-sectional CT images, all screws were located within the femoral neck and none of the screws showed an extraosseous insertion. In addition, the screw arrangement was well adapted to the morphology of the femoral neck. Nakanishi et al. measured the shape of the femoral neck cross section at the narrowest level and suggested a safe and effective arrangement of screws [4]. They recommended insertion of the distal screw just above the calcar femorale, insertion of the anterior screw at 27° anterior to the femoral axis and 14–18 mm proximal, and insertion of the posterior screw slightly posterior to the femoral axis and 10–12 mm proximal, depending on patient size. TresLock was designed based on their study and our case series suggests that their recommended screw positions are accurate.
The distance from the subcapital line to the end of the screw thread was approximately 10 mm in average and 4 mm in minimum. As the femoral neck shortening can occur after internal fixation to maintain the compression between the fragments, a sufficient distance from the screw thread to the fracture line is necessary. If a screw interferes with the fracture line, the screw sliding is disturbed and the compression force between the fragments is no longer applicable. Thanks to the short thread of the TresLock screw, a sufficient distance was preserved in all hip screws.
These results are encouraging in terms of adaptation of the device to the anatomical morphology of the Japanese population. Even in the case of Western populations, the TresLock may also be suitable because the reported neck angle in Western populations is between 129° and 135° [6, 7]. In this study, we had one case (Pauwels III) that required reoperation because of non-union. In this case, although all screws were inserted within the femoral neck, a so-called z-effect, where the penetration of a screw and the back-out of other screws occurred simultaneously, with eventual significant displacement. Although the Pauwels III fracture had a steep fracture line (>50°) [8], the most proximal screw that was most adjacent to the fracture line kept stability in the femoral head. This complication might be caused by the insufficient depth of the distal two screws [9]. In this situation, a misbalanced load transmission could have occurred. We believe that a deeper insertion of the distal two screws could prevent this complication.
Although a longer follow-up study is needed, TresLock shows good anatomical compatibility for femurs among Japanese population. Sufficient depth of the screws might be crucial to avoid complications.
TresLock is a new device and shows good anatomical compatibility for femurs.
References
- 1.Stiasny J, Dragan S, Kulej M, Martynkiewicz J, Plochowski J, Dragan SL. Comparison analysis of the operative treatment results of the femoral neck fractures using side-plate and compression screw and cannulated AO screws. Ortop Traumatol Rehabil 2008;10:350-61. [Google Scholar]
- 2.Stromqvist B, Hansson LI, Nilsson LT, Thorngren KG. Hook-pin fixation in femoral neck fractures. A two-year follow-up study of 300 cases. Clin Orthop Relat Res 1987;218:58-62. [Google Scholar]
- 3.Nishiyama D, Matsumoto T, Hamazaki H. The treatment of femoral neck fractures: Results using cephalocervical screws with sliding mechanism. Eur J Orthop Surg Traumatol 2013;23:907-11. [Google Scholar]
- 4.Nakanishi Y, Hiranaka T, Shirahama M, Uesugi M, Okimura K, Tsubosaka M, et al. Ideal screw positions for multiple screw fixation in femoral neck fractures-study of proximal femur morphology in a Japanese population. J Orthop Sci 2018;23:521-4. [Google Scholar]
- 5.Miyamoto T, Tomita M, Koseki H, Hozumi A, Goto H, Shindo H, et al. Morphology of the femoral neck in Japanese persons: Analysis using CT data. Acta Med Nagasakiensia 2013;58:119-24. [Google Scholar]
- 6.Toogood PA, Skalak A, Cooperman DR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res 2009;467:876-85. [Google Scholar]
- 7.Boese CK, Dargel J, Jostmeier J, Eysel P, Frink M, Lechler P. Agreement between proximal femoral geometry and component design in total hip arthroplasty: Implications for implant choice. J Arthroplasty 2016;31:1842-8. [Google Scholar]
- 8.Bartonicek J. Pauwels’ classification of femoral neck fractures: Correct interpretation of the original. J Orthop Trauma 2001;15:358-60. [Google Scholar]
- 9.Smeets SJ, Kuijt G, van Eerten PV. Z-effect after intramedullary nailing systems for trochanteric femur fractures. Chin J Traumatol 2017;20:333-8. [Google Scholar]