It is important to diagnose Parsonage-Turner syndrome accurately and efficiently as it may lead to uncovering other autoimmune diseases.
Dr. Sean C Clark, Department of Orthopaedic Surgery, Tulane University School of Medicine, 1430 Tulane Avenue, New Orleans, Louisiana, United States. E-mail: sclark19@tulane.edu
Introduction: Parsonage-Turner syndrome is a rare condition that is often misdiagnosed by physicians due to the overlapping symptoms with other conditions such as rotator cuff injury and cervical radiculopathy. The etiology of the Parsonage-Turner syndrome is unknown, but has been associated with an immune-mediated response to rheumatic disease, infection, surgery, and immunizations.
Case Presentation: A 18-year-old female former tennis player with a history of complex regional pain syndrome (CRPS), Ehler-Danlos syndrome (EDS), and two prior right shoulder surgeries presented to the orthopaedic clinic with bilateral shoulder pain. After a third surgery on the right shoulder, the patient later developed constant burning and sharp pain around the right shoulder that radiated toward the chest. She also experienced numbness, tingling, and weakness in the right shoulder along with pain and weakness in the left shoulder. The patient was tender over the right musculocutaneous nerve and both shoulders were inflamed on ultrasound. Electromyography (EMG) and nerve conduction studies were performed, which were consistent with a bilateral subacute on chronic brachial plexopathy, suggestive of Parsonage-Turner syndrome. Rheumatology was consulted due to an extensive family history of autoimmune diseases, leading to an additional diagnosis of ankylosing spondylitis. The patient’s bilateral shoulder pain slowly improved over the following year with physical therapy and prolotherapy treatments.
Conclusion: The case described, herein, represents a unique patient who presents with the rare conditions of ankylosing spondylitis, CRPS, EDS, and Parsonage-Turner syndrome. EMG was critical to differentiate Parsonage-Turner syndrome from the overlapping CRPS symptoms and without this, the diagnosis of ankylosing spondylitis may have been delayed. It is imperative physicians take a thorough history, include uncommon or rare conditions as a potential diagnosis, and undergo thorough testing while evaluating a patient to avoid unnecessary treatment therapies and patient dissatisfaction.
Keywords: Parsonage-Turner syndrome, Ankylosing spondylitis, Ehler-Danlos syndrome, Complex regional pain syndrome.
Parsonage-Turner syndrome, also known as brachial neuritis, neuralgic amyotrophy, or idiopathic brachial plexopathy, is a rare condition with an incidence of roughly 2–3 in 100,000 [1, 2]. The brachial plexus, which comprises nerves C5, C6, C7, C8, and T1, undergoes inflammation either partially or completely resulting in a rapid onset of neuropathic pain. The typical presentation involves inflammation of the upper trunk of the brachial plexus including the long thoracic, suprascapular, and axillary nerves [3]. Other trunks within the brachial plexus and peripheral nerves can be affected, leading to a diversity of presented symptoms. The pain is continuous rather than intermittent and is generally followed by muscle weakness and paralysis. Patients often present with unilateral shoulder pain and weakness, but, less frequently, bilateral symptoms may also occur [3]. This condition was detailed extensively by Parsonage and Turner in 1948, which led to the condition later being named Parsonage-Turner syndrome, even though similar symptoms were described in literature much earlier [4, 5]. Herein, we report a unique case of a patient with bilateral shoulder pain and weakness, along with a history of complex regional pain syndrome (CRPS) and Ehler-Danlos syndrome (EDS).
An 18-year-old right hand dominant female, who is a former avid tennis player, presented to the orthopaedic clinic with bilateral shoulder pain. She had two prior surgeries on the right shoulder by an outside orthopaedic surgeon and unfortunately developed CRPS shortly after the second surgery. Nerve blocks were ineffective, and a constant burning sensation was felt over the right shoulder. In addition, the patient scored 9 out of 9 on the Beighton Scoring System and was diagnosed with EDS. Physical examination revealed bilateral scapular dyskinesia and multiple scars on her anterior right shoulder, along with hyperesthesia. Palpation of the scars reproduced local and referred pain down the right arm. The treatment included scapular bracing and physical therapy for the left shoulder, while the right shoulder underwent extensive debridement, posterior capsule plication, and anteroinferior glenohumeral ligament reconstruction with a gracilis allograft. The patient was progressing well until 16 months postoperatively when she returned to the clinic with a complaint of constant burning and sharp pain around the right shoulder that radiated toward the chest. She also experienced numbness, tingling, and weakness in the right shoulder along with pain and weakness in the left shoulder. The patient was tender over the right musculocutaneous nerve and both shoulders were inflamed on ultrasound. She had trouble sleeping and woke up frequently throughout the night due to the severe pain.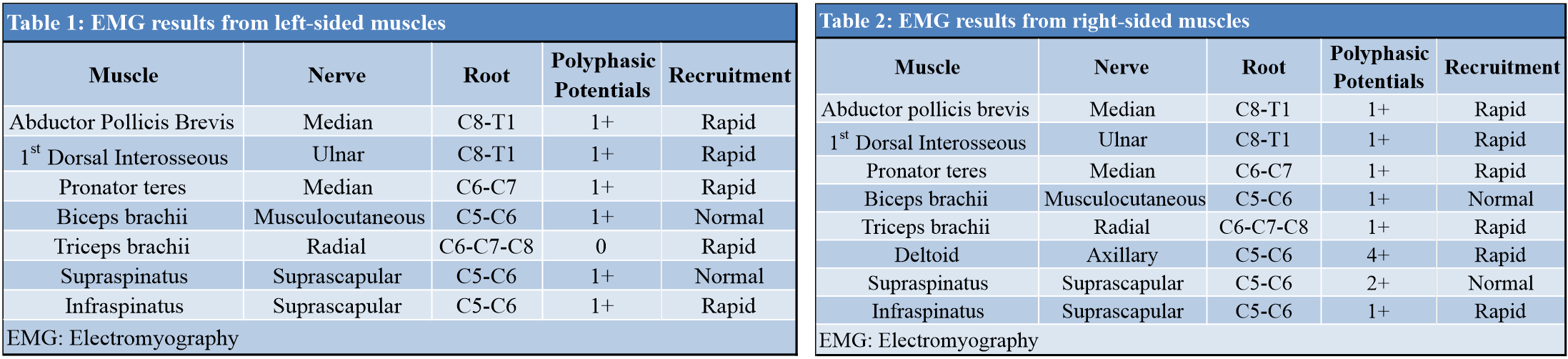
Physiatry was consulted and electromyography (EMG) and nerve conduction studies were performed (Tables 1, 2). Abnormal EMG findings were consistent with a bilateral subacute on chronic brachial plexopathy, suggestive of Parsonage-Turner syndrome. She had full neck flexion and extension with a negative Spurling’s maneuver and unremarkable MRI of the cervical spine. Interestingly, after this diagnosis, it was discovered that the patient had a family history of autoimmune conditions as her mother had fibromyalgia and was an HLA-B27 carrier, her brother had spondyloarthropathy, and her aunt had rheumatoid arthritis. She was then referred to rheumatology who noted that the patient reported morning stiffness in her upper back for 2 h every day for the past year. A laboratory workup of autoimmune diseases was conducted, and the patient tested positive for the HLA-B27 allele. She was then diagnosed with ankylosing spondylitis. The patient’s bilateral shoulder pain continued to improve over the following year with physical therapy and prolotherapy treatments. During this time, she also underwent medial patellofemoral ligament reconstruction with allograft due to chondromalacia patella and recurrent patellar dislocations, which may have been partially due to the patient’s EDS. The current treatment regimen is to continue with regular physical therapy and prolotherapy treatments for the Parsonage-Turner syndrome and EDS, pain management for the CRPS, and follow-up with rheumatology for the ankylosing spondylitis.
Parsonage-Turner syndrome, brachial neuritis, neuralgic amyotrophy, or idiopathic brachial plexopathy is an uncommon condition that can elude the diagnosis of physicians. The previous literature suggests that this condition may actually be more common than previously reported due to misdiagnosis or late diagnosis [6, 7]. For example, a prior study tracked all new cases of neck, shoulder, or arm complaints in 1 year from two large primary care centers serving a population just over 14,000 [7]. Of the 492 patients with these complaints, 14 were diagnosed with neuralgic amyotrophy. This accounts for a 1-year incidence rate of 1/1000, which is 30–50 times higher than previously suggested [7]. The etiology of the Parsonage-Turner syndrome is unknown, but has been associated with an immune-mediated response to rheumatic disease, infection, surgery, immunizations, and stressful exercise [8, 9, 10]. Duplications of the septin 9 gene have been found to be a causative factor for neuralgic amyotrophy in the hereditary form, but this is far less common than the sporadic or idiopathic form [11]. This condition is roughly twice as common in men than in women and onset usually presents when a patient is in their forties [12]. The prognosis is favorable as most patients recover from Parsonage-Turner syndrome over a period of months to 2–3 years depending on the severity of the nerves affected [6, 13]. Due to the anatomic location of the brachial plexus and clinical symptoms presented, diagnosis can be challenging for physicians as other conditions, such as rotator cuff damage or cervical radiculopathy, may present similarly. Early diagnosis of Parsonage-Turner syndrome is important as misdiagnosis can lead to unnecessary therapeutic intervention, diagnostic testing, and patient dissatisfaction. EMG, nerve conduction studies, magnetic resonance imaging (MRI), and cerebrospinal fluid examination can help support the diagnosis and rule out other conditions, but a thorough clinical history and physical examination are most pertinent. EMG and nerve conduction studies can also help isolate and determine the rate and severity of denervation, while MRI can be helpful in ruling out tumors and disc herniations.
In the presented case, an 18-year-old female presented to the clinic and later developed bilateral Parsonage-Turner syndrome in addition to her already disabling CRPS and EDS. A study by van Alfren and van Engelen found that out of 115 patients with antecedent events (infection, surgery, autoimmune diseases, etc.) before the onset of neurologic amyotrophy, 16 (13.9%) had surgery before the diagnosis [6]. It is unclear if there was an antecedent event resulting in the onset of Parsonage-Turner syndrome in this patient, but it is unlikely that it was caused by the patient’s prior surgeries as the most recent operation was sixteen months before the onset of symptoms. In contrast, it is more probable that the antecedent event could have been rheumatologic in origin due to the patient’s latest diagnosis of ankylosing spondylitis. The previous studies have shown other rheumatologic diseases to be associated with Parsonage-Turner syndrome including systemic lupus erythematous and polyarteritis nodosa [8, 14]. However, this is the first report of a potential relationship between Parsonage-Turner syndrome and ankylosing spondylitis. A final potential cause of the patient’s Parsonage-Turner syndrome is the prior diagnosis of EDS, which has been evidenced in multiple case reports [9, 10]. van Alfren and van Engelen found that the infraspinatus, supraspinatus, biceps brachii, pronator teres, deltoid, triceps brachii, and dorsal interosseous muscles were affected 71.8%, 65.7%, 61.0%, 52.3%, 46.0%, 43.4%, and 30.0% of the time, respectively [6]. These muscles were also affected in the presented case suggesting a more typical presentation of Parsonage-Turner syndrome (Tables 1, 2). Interestingly, the serratus anterior muscle was affected 70.0% of the time [6], but was not affected in this patient as serratus anterior abnormalities on the EMG were not found. Rotator cuff damage was excluded due to physical examination along with the sudden onset of shoulder pain rather than a gradual onset of symptoms. Cervical radiculopathy was excluded due to symptoms not worsening with a change in neck positioning, normal findings on the EMG and nerve conduction studies, and no significant abnormalities found on the cervical spine MRI. Interestingly, the patient was previously diagnosed with CRPS and EDS, which made the diagnosis of Parsonage-Turner syndrome more challenging as both conditions can cause pain and weakness around the shoulder [3]. Since CRPS is a diagnosis of exclusion, abnormalities on an EMG or nerve conduction study would commonly not be seen [15]. Thus, these tests were critical to differentially diagnose Parsonage-Turner syndrome. Unexpectedly, the diagnosis of Parsonage-Turner syndrome ultimately led to uncovering the patient’s lengthy family history of autoimmune diseases and later a diagnosis of ankylosing spondylitis. Without the diagnosis of Parsonage-Turner syndrome, the diagnosis of ankylosing spondylitis may have been delayed.
The case described herein represents a unique patient who presents with the rare conditions of ankylosing spondylitis, CRPS, EDS, and Parsonage-Turner syndrome. EMG was critical to differentiate Parsonage-Turner syndrome from the overlapping CRPS symptoms and without this, the diagnosis of ankylosing spondylitis may have been delayed. It is imperative physicians take a thorough history, include uncommon or rare conditions as a potential diagnosis, and undergo thorough testing while evaluating a patient to avoid unnecessary treatment therapies and patient dissatisfaction.
EMG is critical to differentially diagnose Parsonage-Turner syndrome from other overlapping conditions such as CRPS. It is important to diagnose Parsonage-Turner syndrome accurately and efficiently as it may lead to uncovering other autoimmune diseases, such as ankylosing spondylitis, in this case.
References
- 1.Beghi E, Kurland LT, Mulder DW, Nicolosi A. Brachial plexus neuropathy in the population of Rochester, Minnesota, 1970-1981. Ann Neurol 1985;18:320-3. [Google Scholar]
- 2.MacDonald BK, Cockerell OC, Sander JW, Shorvon SD. The incidence and lifetime prevalence of neurological disorders in a prospective community-based study in the UK. Brain 2000;123:665-76. [Google Scholar]
- 3.Smith CC, Bevelaqua AC. Challenging pain syndromes: Parsonage-Turner syndrome. Phys Med Rehabil Clin N Am 2014;25:265-77. [Google Scholar]
- 4.Allen IM. The neurological complications of serum treatment: With report of a case. Lancet 1931;218:1128-31. [Google Scholar]
- 5.Parsonage MJ, Turner JW. Neuralgic amyotrophy; the shoulder-girdle syndrome. Lancet 1948;1:973-8. [Google Scholar]
- 6.van Alfen N, van Engelen BG. The clinical spectrum of neuralgic amyotrophy in 246 cases. Brain 2006;129:438-50. [Google Scholar]
- 7.van Alfen N, van Eijk JJ, Ennik T, Flynn SO, Nobacht IE, Groothuis JT, et al. Incidence of neuralgic amyotrophy (parsonage turner syndrome) in a primary care setting – A prospective cohort study. PLoS One 2015;10:e0128361. [Google Scholar]
- 8.Bloch SL, Jarrett MP, Swerdlow M, Grayzel AI. Brachial plexus neuropathy as the initial presentation of systemic lupus erythematosus. Neurology 1979;29:1633-4. [Google Scholar]
- 9.Kayed K, Kåss B. Acute multiple brachial neuropathy and Ehlers-Danlos syndrome. Neurology 1979;29:1620-1. [Google Scholar]
- 10.De Graaf AS. Neuralgic amyotrophy in identical twins with Ehlers-Danlos syndrome. Eur Neurol 1973;9:190-6. [Google Scholar]
- 11.Collie AM, Landsverk ML, Ruzzo E, Mefford HC, Buysse K, Adkins JR, et al. Non-recurrent SEPT9 duplications cause hereditary neuralgic amyotrophy. J Med Genet 2010;47:601-7. [Google Scholar]
- 12.Martínez-Salio A, Porta-Etessam J, Berbel A, Alonso A, Gutiérrez-Rivas E, Trueba J. Amyotrophic neuralgia: Review of 37 cases. Rev Neurol 1998;27:823-6. [Google Scholar]
- 13.Cruz-Martínez A, Barrio M, Arpa J. Neuralgic amyotrophy: Variable expression in 40 patients. J Peripher Nerv Syst 2002;7:198-204. [Google Scholar]
- 14.Allan SG, Towla HM, Smith CC, Downie AW, Clark JC. Painful brachial plexopathy: An unusual presentation of polyarteritis nodosa. Postgrad Med J 1982;58:311-3. [Google Scholar]
- 15.Cutts S, Gangoo S, Srinivasan SH, Modi N, Pasapula C, Power D. Complex regional pain syndrome: An evolving perspective. Postgrad Med J 2021;97:250-5. [Google Scholar]








