Clinicians should consider the possibility of DVT and traumatic osteonecrosis in children with persistent leg pain and swelling.
Dr. Sarah M Choi, Department of Trauma and Orthopaedic, University Hospital of Wales, Cardiff, Wales, United Kingdom. E-mail: sarah.choi@wales.nhs.uk
Introduction:Deep vein thrombosis (DVTs) in children is rare, normally linked to pathologies such as major traumatic injury, thrombophilia, and malignancy. Osteonecrosis is still poorly understood. There is growing support to include hypercoagulable states as a predisposing factor, however, no definitive correlation has been found. At present, there are no conclusive literature on the links between osteonecrosis and DVT.
Case Presentation: This report describes an unusual and rare case of osteonecrosis and idiopathic DVT in an 11-year-old girl who initially presented with a sprained left ankle. On follow-up, pain was persistent and subsequent radiological investigations revealed extensive DVT, and magnetic resonance imaging scan revealed osteonecrosis of the distal left tibia. Initial blood tests were normal, however with follow-up with hematology, a diagnosis of antithrombin deficiency was made, with the treatment of lifelong anticoagulation. Our patient had continued orthopedic input for clinical and radiographic surveillance to monitor leg length discrepancy.
Conclusion:This case highlights the need to engage in close follow-up and the cautionary care required when young children present with non-resolving severe pain, to consider osteonecrosis and DVT. Our case also highlights the need for further research into the relationship between minor injuries and DVTs and osteonecrosis in children, and the potential synergistic relationship between DVTs and osteonecrosis.
Keywords:Osteonecrosis, pediatric orthopedics, deep vein thrombosis, coagulopathy.
Deep vein thrombosis (DVTs) in children is rare. Estimates of the annual incidence range from 0.14 to 0.21 per 10,000 children [1]. This rises to up to 58 per 10,000 in hospitalized admissions [2]. Rates are higher in children with pathologies such as thrombophilia, malignancy, and cardiac disease. Major traumatic injury is also indicated as a risk factor. Studies have shown that although the risk is greater following traumatic injury, it is still substantially lower than with adult trauma patients, with rates currently reported at 0.03–0.4% [1]. Although rare, the importance of correctly diagnosing and treating DVT is paramount to prevent mortality from complications, such as pulmonary embolism, which has been reported [3].
Osteonecrosis normally arises from direct damage to the bone’s blood supply, bone, or marrow. However, in many patients, the mechanism of this pathology is not fully understood [4]. In children, osteonecrosis normally is caused by sickle cell disease, injury to bone through fracture or dislocation, and long-term corticosteroids for both non-cancer and cancer diseases such as ALL or lymphoma. At present, there is no conclusive literature on the links between osteonecrosis and DVT. To the best of our knowledge, no case reports have been published of DVT and osteonecrosis occurring in children at the same time. We present a rare and unusual case of a child who developed both osteonecrosis and bilateral DVTs following a minor ankle injury.
An 11-year-old girl was seen in A&E after spraining her left ankle while ice skating. Examination and plain radiographs showed no obvious injury (Fig. 1) and she was discharged home. She represented 3 days later, unable to weight bear on the left leg and was reviewed in fracture clinic. She was diagnosed with a soft-tissue injury, provided with a functional walking boot, for follow-up 2 weeks later. On follow-up of her left ankle, she had both lateral and medial malleolar tenderness, ankle swelling, and decreased range of movement. She was neurovascularly intact. Repeat plain films demonstrated periosteal reaction at the left distal tibia (Fig. 2). She continued with the walking boot and referred for physiotherapy.
A month following, she developed swelling and blue discoloration in the right leg; lower limb duplex confirmed a right-sided DVT. Hematological review and subsequent thrombophilia screen were deemed normal and she was started on dalteparin for 6 months. A repeat duplex scan a month later showed acute iliofemoral DVT bilaterally extending to the distal inferior vena cava. The patient was reviewed in fracture clinic, 6 weeks from the initial injury. Plain films confirmed established periosteal reactions in the left distal tibia (Fig. 3). Magnetic resonance imaging (MRI) confirmed associated osteonecrosis of the left distal tibia (Fig. 4).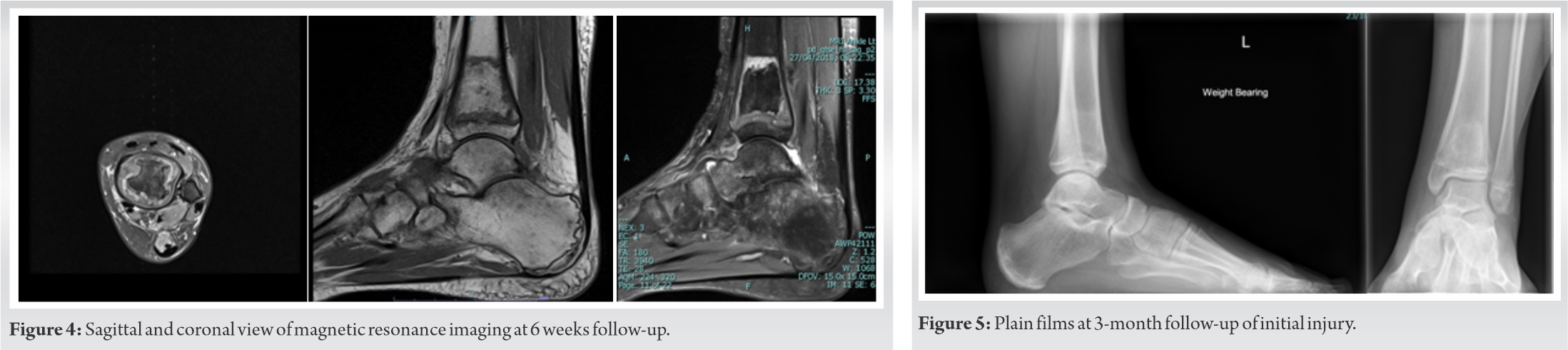
This is a rare and unusual case of a child who developed bilateral DVTs and osteonecrosis following a minor injury. DVTs in children are rare, with an increased risk in children with other conditions. An analysis of the Canadian registry of DVT and PE in children, highlighted conditions associated with DVT. These included: Inherited pre-thrombotic disorder, systemic infection, cancer, congenital heart disease, central venous catheters, trauma, total parenteral nutrition due to short gut syndrome, nephrotic syndrome, surgery, oral contraceptives, obesity, SLE, sickle cell anemia, and liver failure [5]. 137 children were included in study and 132 had identifiable associated conditions. The study found that 8.8% of the children were found to have inherited prothrombotic disorders. The authors added that only 45 children out of the 137 were evaluated for prothrombotic disorders, and therefore, thrombophilia could be more prevalent than their findings. The same study showed that DVT without any associated condition is extremely rare.
During a 7-year study, Raffini et al. found that the annual rate of VTE had increased by 70% from 34 to 58 cases per 10,000 hospital admissions at Children’s Hospital of Philadelphia [2]. The authors state that it is difficult to argue whether there is a true increase in pediatric VTEs or whether there is an increase in detection of previously undiagnosed VTE due to heightened awareness of VTE. Other authors have hypothesized that progress in radiological imaging and increased survival of children with previously incurable diseases due to medical and surgical advances, could add to the rise of pediatric VTE cases [6]. Although DVTs are rare in children, diagnosis and subsequent treatment should be carried out promptly. This is to prevent the complication of PE [7] and potential fatalities which have been reported in children. Sridhar et al. described a case of 6 years old with a fatal PE following DVT of the lower extremity where the initial diagnosis was irritable hip and pneumonia [3]. Our patient had no family history of coagulopathy or any medical history. Preliminary hematological investigations were considered normal and the initial diagnosis was of an idiopathic DVT. However, further review by hematologists suggested that our patient most likely had a new mutation of antithrombin deficiency. Antithrombin deficiency disorder is characterized by a tendency to form clots in the veins. Antithrombin is an important glycoprotein in the coagulation cascade (Image 1). It inhibits thrombin and factor Xa and IXa which are required to form thrombin. With reduced levels of antithrombin, more thrombin is activated, leading to increased likelihood of clot formation. Antithrombin deficiency is diagnosed by detecting low antithrombin levels in the blood. The initial antithrombin level for our patient was below the normal range (51.9 iu/d). This was not initially considered to be abnormal, as acute clots can consume antithrombin, reducing its levels. The diagnosis of antithrombin deficiency was later made as antithrombin levels persistently stayed low (49 iu/d) despite treatment. It is, therefore, imperative that antithrombin levels are checked post-treatment, to make the definitive diagnosis of antithrombin deficiency disease. de la Morena-Barrio et al. looked at 968 patients known to have antithrombin deficiency. They found 7.5% of their subjects formed a thrombus before the age of 19. They also noted that the peak incidence to form a thrombus was during neonatal and adolescent periods [8].
Other authors have stressed the need to carefully investigate children with thrombosis to find an underlying cause due to the high recurrence rate [9].
Osteonecrosis arises due to direct damage to the bone’s blood supply, however, in many patients, the mechanism of osteonecrosis is not fully understood. Prevalence for osteonecrosis varies widely in literature, this may reflect the differences in the definition and cause of osteonecrosis. It is thought that several factors could cause osteonecrosis, such as glucocorticoids, alcohol, SLE, antiphospholipid antibodies, trauma, sickle cell disease, Gaucher disease, ALL, decompression disease, transplantation, inherited thrombophilia, radiation therapy, and HIV infection [13]. It is pertinent to mention that in children, in addition to the factors mentioned, many conditions within the osteochondrosis family (such as Legg-Calve-Perthes and Kohler disease) can present with osteonecrosis but with elements of reossification [4].
The classic MRI appearance of osteonecrosis is that of a segmental area of low signal intensity in the subchondral bone, surrounded by a low signal intensity border. A double line sign can be present. When osteonecrosis presents as an area of diffuse low signal intensity, it can be difficult to differentiate it from tumors. With calcifications, osteonecrosis can also simulate those of chondroid lesions [10]. We would like to note that differentiating a bone infarct from an enchondroma or low-grade chondrosarcoma on plain films is difficult. Cartilaginous tumors such as chondrosarcoma may show endosteal scalloping which would not be present in osteonecrosis. A case reported by Shimizu et al. discusses the difficulty of differentiating osteonecrosis from chondrosarcoma from T1-weighted MRI and that contrast-enhanced T1 MRI played an important role in diagnosis [11]. It is important for clinicians to be aware of other pathologies that can give a similar MRI image to osteonecrosis. Our patient’s MRI images and clinical picture gave us a confident diagnosis of osteonecrosis.
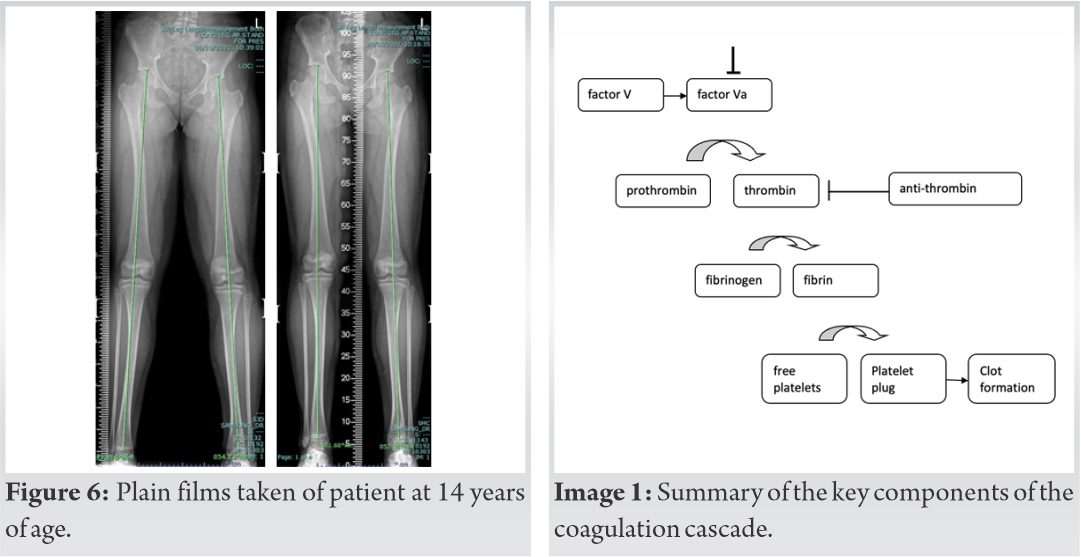
It has been hypothesized for over 50 years that increased intravascular coagulation could be a pathogenetic mechanism that contributes to osteonecrosis [11, 12, 13, 14, 15]. However to date, there is no definitive correlation. Lykissas et al. discussed the theories behind the hypothesis, exploring both primary factors of hypercoagulability, such as protein C and protein S deficiency, and secondary factors such as pregnancy, systemic lupus erythematosus, and sickle cell disease. The authors stressed that with the growing support for the hypothesis, there is a need for research to demonstrate definitive correlation [15]. At present, there is no evidence to suggest any correlation between minor injuries (no fractures) and osteonecrosis. A case report in the journal of pediatric orthopedics, discussed a 5-year-old boy developing osteonecrosis 2 years after sustaining an ankle sprain [16]. The osteonecrosis in the distal fibular epiphysis required surgical treatment. This patient was healthy with no previous medical history. Further research in this area would be beneficial, to see whether minor injuries could be a trigger for osteonecrosis. Our patient’s osteonecrosis in the left distal tibia extended to her physis. Leg length discrepancy and growth were, therefore, monitored. When children have not reached skeletal maturity, it is being advised that observation is undertaken until growth is complete. When leg length discrepancy is >2 cm, simple non-surgical interventions such as shoe lifts could be offered or surgical options can be explored. Our patient required no treatment for her osteonecrosis as there was so evidence of bone collapse or instability. Our patient is left with an anatomical leg length discrepancy of 15 mm, but functionally asymptomatic pursuing activities, she was able to enjoy, before her injury. At present, there is no conclusive literature on the links between DVT and osteonecrosis. We have two hypotheses to explain how our patient developed both DVT and osteonecrosis at the same period of time. Our first hypothesis is that the initial ankle injury triggered osteonecrosis. With the pain, reduced mobility, and underlying antithrombin deficiency, this promoted the development of the DVT. Our second hypothesis is that the pain from the initial ankle injury and resultant reduced mobility, with the underlying antithrombin deficiency triggered the DVT. The formation of the DVT subsequently compromised the blood supply to the left distal tibia causing osteonecrosis.
We have presented a rare and unusual case of a child who developed both osteonecrosis and bilateral DVTs. The main cause for the formation of the DVT was our patient’s antithrombin deficiency, however, we are unable to definitively confirm the cause of her osteonecrosis. Our case highlights that further research is required to look at whether there is a pathological link between DVTs and osteonecrosis, and whether there is a definitive correlation between hypercoagulative states and osteonecrosis. The case also highlights the need for further research on the relationship between minor injuries, DVT, and osteonecrosis. In those diagnosed with DVT, it is imperative that risk factors such as thrombophilia are considered and antithrombin levels are checked post-treatment to make a definitive diagnosis.
Both DVT and traumatic osteonecrosis are rare in children. Clinicians should consider the possibility of theses diagnoses in children with persistent leg pain and swelling. Further research is required to look at the relationship between DVTs and osteonecrosis, and other factors such as minor injuries. Injuries near the physis require follow-up to monitor growth and leg length discrepancy. Complex cases require a multispecialty approach.
References
- 1.Albisetti M, Chan A. Venous Thrombosis and Thromboembolism in Children: Risk Factors, Clinical Manifestations, and Diagnosis. Available from: https://www.uptodate.com/contents/venous-thrombosis-and-thromboembolism-in-children-risk-factors-clinical-manifestations-and-diagnosis [Last accessed on 2019 Dec 02]. [Google Scholar]
- 2.Raffini L, Huang YS, Witmer C, Feudtner C. Dramatic increase in venous thromboembolism in children’s hospitals in the United States from 2001 to 2007. Pediatr 2009;124:1001-8. [Google Scholar]
- 3.Sridhar A, Rao NK, Chakraborty S. A six-year old with fatal pulmonary embolism. Acta Paediatr 2007;94:977-9. [Google Scholar]
- 4.Jones L, Mont M. Osteonecrosis (Avascular Necrosis of Bone). Available from: https://www.uptodate.com/contents/osteonecrosis-avascular-necrosis-of-bone#H17 [Last accessed on 2019 Dec 02]. [Google Scholar]
- 5.Andrew M, David M, Adams M. Venous thromboembolic complications (VTE) in children: First analyses of the Canadian registry of VTE. Blood 1994;83:1251-7. [Google Scholar]
- 6.Klaassen LM, van Ommen CH, Middeldorp S. Manifestations and clinical impact of pediatric inherited thrombophilia. Blood 2015;125:1073-7. [Google Scholar]
- 7.van Ommen CH, Heijboer H, Büller HR, Hirasing RA, Heijmans HS, Peters M. Venous thromboembolism in childhood: A prospective two-year registry in the Netherlands. J Pediatr 2001;139:676-81. [Google Scholar]
- 8.de la Morena-Barrio B, Orlando C, de la Morena-Barrio ME, Vicente V, Jochmans K, Corral J. Incidence and features of thrombosis in children with inherited antithrombin deficiency. Haematologica 2019;104:2512-8. [Google Scholar]
- 9.Celkan T, Dikme G. Thrombosis in children: Which test to whom, when and how much necessary? Turk Pediatri Arsivi 2018;53:1-9. [Google Scholar]
- 10.Mhuircheartaigh JN, Lin YC, Wu JS. Bone tumor mimickers: A pictorial essay. Indian J Radiol Imaging 2014;24:225-36. [Google Scholar]
- 11.Shimizu J, Emori M, Nagoya S, Sasaki M, Tateda K, Yamashita T. Chondrosarcoma mimicking MRI of the osteonecrosis of the femoral head: A case report. BJR Case Rep 2018;4:20170098. [Google Scholar]
- 12.Boettcher WG, Bonfiglio M, Hamilton HH, Sheets RF, Smith K. Non-traumatic necrosis of the femoral head: Part I. Relation of altered hemostasis to etiology. J Bone Joint Surg Am 1970;52:312-21. [Google Scholar]
- 13.Bonfiglio M, Lambertsen CJ. Underwater Physiology V: Proceedings Fifth Symposium Underwater Physiology. Bethesda, MD: FASEB Development of Bone Necrosis Lesions; 1976. p. 117-32. [Google Scholar]
- 14.Jones JP Jr., Sakovich L, Anderson CE. Beckman EL, Elliot D, Smith EM. Experimentally Produced Osteonecrosis as a Result of Fat Embolism, Dysbarism-related Osteonecrosis. Washington, DC: US Government Printing Office; 1974. p. 117. [Google Scholar]
- 15.Lykissas M, Gelalis I, Kostas-Agnantis I, Vozonelos G, Korompilias A. The role of hypercoagulability in the development of osteonecrosis of the femoral head. Orthop Rev 2012;4:e17. [Google Scholar]
- 16.Villas C, Schweitzer D. Avascular necrosis of the distal fibular epiphysis: A new condition? J Orthop 1996;16:497-9. [Google Scholar]