The infected non-union of ulna is a rare occurrence in pediatric population and can be managed with simple low-cost technique with end result of full restoration of function and preventing chronic osteomyelitis and associated disabilities.
Dr. Ajay M Wankhade, Department of Orthopaedics, Seth GS Medical College and KEM Hospital, Mumbai, Maharashtra, India. E-mail: drajaywankhade@gmail.com
Introduction:Infected non-union is rare in pediatric patients. Various methods have been described in the literature to manage such cases. We present a familiar and simple technique to treat a non-union in pediatric population.
Case Presentation:A 4-year-old boy came to us with a right-sided proximal forearm swelling and tenderness. Clinical and radiological features suggestive of osteomyelitis of ulna with a history of the right-sided forearm cellulitis when he was 4 months of age which was managed with incision and drainage at that time. The patient underwent surgery for surgical debridement with drilling of ulnar cortex for pus evacuation. Postoperatively, the patient developed a stress fracture at drilling site which eventually went into a non-union. In second surgery, bony union achieved with the help of non-vascularized fibular strut graft and iliac cancellous graft.
Conclusion:There are numerous complications of osteomyelitis in pediatric patients and their management has been previously highlighted throughout literature. Here, we present a rare occurrence case report highlighting management of pediatric atrophic infected gap non-union of ulna by non-vascularized fibula strut stabilized by Titanium Elastic nail which offers a simple yet an elegant solution in a low-cost setting with complete bony union and restoration of function.
Keywords:Ulna osteomyelitis, non-union, pediatric, orthopedic, fibula graft.
Reports of non-union in children are rare [1]. A literature review of various surgical techniques of managing forearm fractures with particular emphasis on non-union following surgical intervention in ulna revealed a variety of methods [2, 3, 4]. The use of non-vascularized fibular graft as a biological bridging device proved to be a solution.
This case report aims to highlight a uncommon case which was successfully treated with this simple technique and also is an effort to gain some insight into the infrequent problem of non-union of diaphyseal bone of forearm in children.
A 4-year-old boy, with no known medical illness, came to us in our out-patient department with a gross swelling over the right forearm. He had a history of the right forearm cellulitis associated with suspected compartment syndrome at 6 months of age which was treated with incision, drainage, and fasciotomy. Fasciotomy site healed completely with secondary intention.
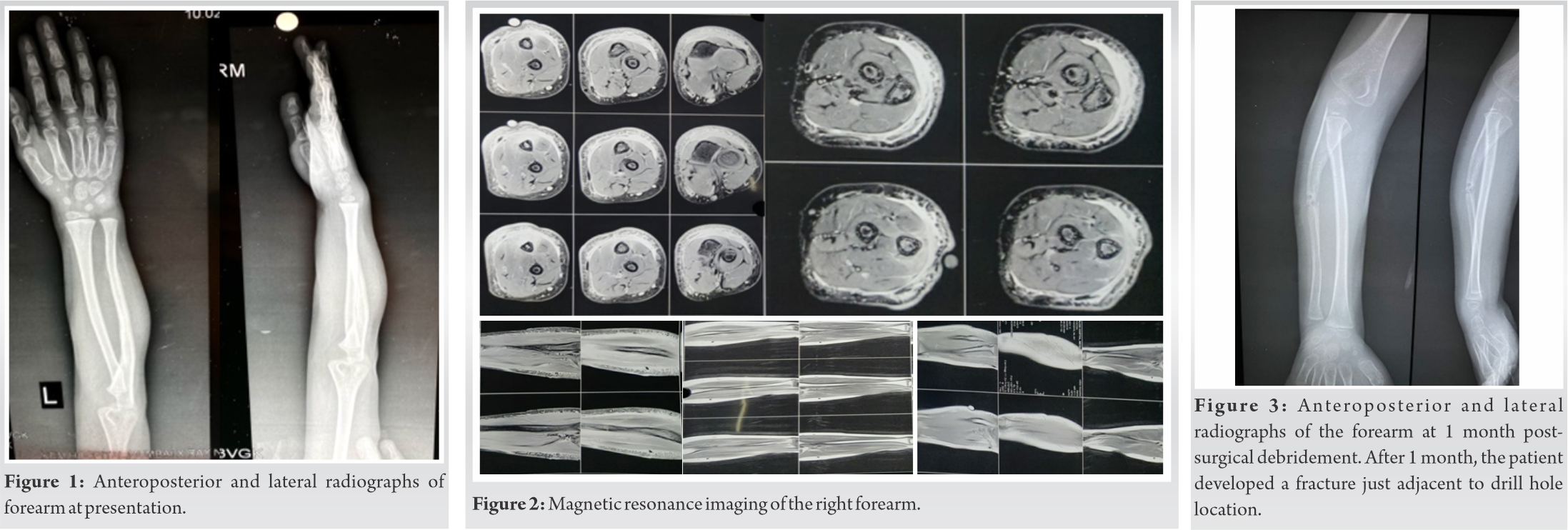
On examination, the patient had swelling and tenderness on the dorsal ulnar surface over the underlying bone with no local rise of temperature. Motion ranging from 70° supination, 80 degrees pronation, and elbow flexion from 0 to 130°. X-ray examination revealed focal opacity with periosteal reaction in proximal one-third of ulna (Fig. 1). MRI findings were suggestive of periosteal elevation with underlying abscess (Fig. 2).
After that, the patient was taken for surgical debridement and evacuation of pus under general anesthesia. Ulna was exposed in the internervous plane between flexor carpi ulnaris (FCU) and extensor carpi ulnaris (ECU). Intraoperatively, the proximal ulna failed to show any osteomyelitic changes. Ulnar cortex was drill holed by 2 mm k-wire, no pus discharge was noted indicating absence of medullary collection at that time. Localized opacities were seen in ECU and FCU, from which sample was sent for culture sensitivity and histopathology. Methicillin resistant coagulase negative Staphylococci (MRCONS) was isolated and cultured. Antibiotics (Inj. Linezolid as per weight) were given and limb was protected and immobilized in an above elbow (AE) cast for 6 weeks. Postoperatively after 1 month, the patient developed a fracture just adjacent to drill hole location with AE cast in situ (Fig. 3).
Further, fracture was managed with immobilization in AE cast for 6 weeks. Subsequently, fracture failed to unite and a diagnosis of frank non-union was made at the drill hole induced fracture site (Fig. 4) after a period of 6 months. At the time, white blood cell count and ESR (Erythrocyte sedimentation rate) were 5100/mm3 and 7 mm/h, respectively, with no other signs of infection.
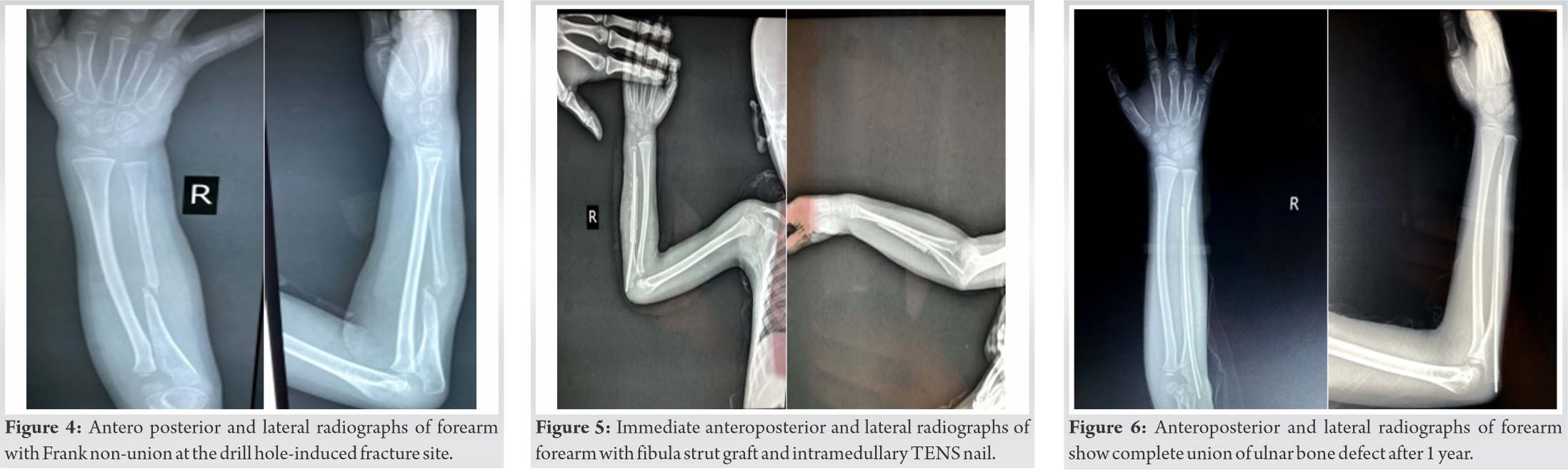
With persistent non-union for 6 months, the patient was taken up for surgery, where the non-union site was exposed and canal opened. No granulation tissue or other signs of inflammation were noted. Proximal end of distal fragment at the non-union site was thin and conical in shape with a gap of around 1 cm. 6.5 cm of fibula was excised with from the right leg, split, and wrapped around the non-union site. 6.5 cm of fibula was excised using minimally invasive technique [5] and split which were wrapped around non-union site. The site of osteotomy for fibula was marked 8 cm from distal fibula and 6 cm from proximal end. Two incisions were taken. Spatula was passed between the soleus and fibular muscles and step by step subperiosteal detachment performed cautiously. Then, the osteotomy was performed proximally and distally using oscillating saw. The graft was grasped with clamps and then the graft was mobilized on its axis by rotating it and the bone graft extracted. Iliac crest cancellous bone graft was harvested and placed at the non-union site to enhance union. To hold fibula in place, vicryl cerclages were taken. The construct was stabilized by a 2 mm intramedullary Titanium Elastic Nailing System (TENS) nail. Postoperatively, AE slab was given for 4 weeks for immobilization. Two doses of IV antibiotics (inj. Cefuroxime as per weight) were given postoperatively. Post-operative X-ray is shown in (Fig. 5).
Here, (Fig. 6) shows complete union of ulnar bone defect after 1 year.
The TENS nail was removed 1.5 years postoperatively with a both clinical and radiographic examination demonstrating complete bony union (Fig. 7).
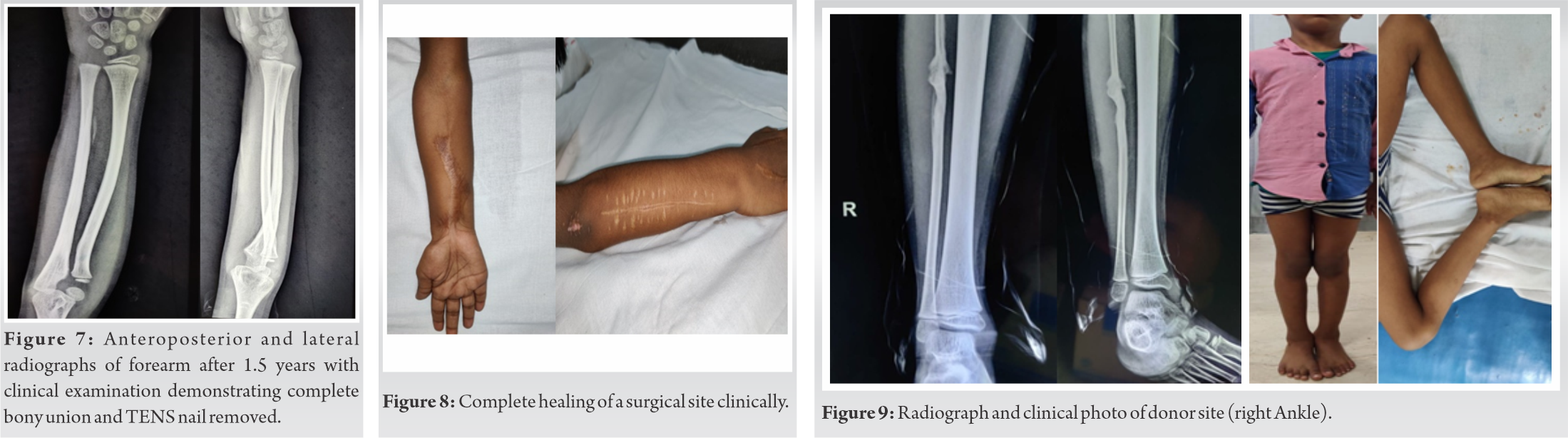
Active range of motion at that time was full, unrestricted and the wound had completely healed (Fig. 8). At a follow-up of 1.5 years, there was no donor site morbidity at ankle noted (Fig. 9).
Non-union is a rare entity in pediatric population. Non-union is defined as a failure of a fracture to unite 9–12 months after the initial insult. Factors responsible for non-union in children are mainly either surgical or infective. In cases involving infection, formation of necrotic/lytic bone with pus hampers union. Mechanical factors such as distracted fracture fragments, interposition of soft tissue, or excessive movement at fracture site are other well documented causes of non-union [6, 7].
In this patient, we feel different factors played a role at various points of time, infection being the predominant one. Staphylococcus aureus is the most common organism responsible for chronic osteomyelitis [8]; in our case, it was MRCONS. The initial drill hole during first surgery created a stress point for the fracture. It ultimately went into atrophic non-union over a period of time.
Although various techniques to manage atrophic non-union have previously been reported, this rare case report aims to highlight the outcome and technique of using fibula with cancellous bone graft to achieve union in a pediatric case. Due to its accessibility, expendibility, strength, and shape, the fibula is more suitable for use in the forearm compared to a rib or iliac crest bony strut graft [9]. Success rate with regards of autograft is known to be high as long as harvested bone is of good quality and recipient site is clean [10]. In this technique, an autologous fibular graft was used as a strut, while iliac crest cancellous graft filled the defect and helped in union. The fibular bone graft in this case was harvested with a purpose to eventually function as an on-lay graft and biological bridging device; being mechanically stronger and providing compressive bone to bone contact. Another important step was to drill the atrophied end with 2 mm k-wire and stabilizing the construct with a 2 mm TENS nail. This was to stimulate the release of osteoinductive factors and migration of osteoprogenitor cells from bone marrow to aid in reparative process. The use of AE cast is the final important step to protect the fragile graft for the immobilization period. A review of the literature showed that while this technique has been used for tibia and radius, it has not been reported for the treatment of infected gap nonunion of proximal ulna in pediatric population.
Management of pediatric atrophic gap non-union of ulna with on-lay split fibula strut graft as a composite bridge envelope along with osteoinducive effects of iliac crest cancellous bone graft stabilized with an intramedullary TENS nail offers a low-cost technique with a low learning curve providing satisfactory results with no complications observed at follow-up.
Here, we would like to emphasize on the fact that though infected non-union of ulna is a rare occurrence in pediatric population, orthopedic surgeons should be equipped to handle such cases in a low-cost setting with the end result of restoration of function and prevention of disability which inadvertently follows cases of chronic osteomyelitis.
References
- 1.Arslan H, Subaşý M, Kesemenli C, Ersuz H. Occurrence and treatment of nonunion in long bone fractures in children. Arch Orthop Trauma Surg 2002;122:494-98. [Google Scholar]
- 2.Ring D, Jupiter JB, Gulotta L. Atrophic nonunions of the proximal ulna. Clin Orthop Relat Res 2003;409:268-74. [Google Scholar]
- 3.Egol KA, Tejwani NC, Bazzi J, Susarla A, Koval KJ. Does a Monteggia variant lesion result in a poor functional outcome? A retrospective study. Clin Orthop Relat Res 2005;438:233-8. [Google Scholar]
- 4.Rotini R, Antonioli D, Marinelli A, Katusić D. Surgical treatment of proximal ulna nonunion. Chir Organi Mov 2008;91:65-70. [Google Scholar]
- 5.ScienceDirect. Minimally invasive harvesting of non-vascularized fibular graft in children. Elsevier ScienceDirect. Available from: https:www//linkinghub.elsevier.com/retrieve/pii/S1877056815000900 [Last accessed on 2015 Jun 01]. [Google Scholar]
- 6.Zura R, Mehta S, Della Rocca GJ, Steen RG. Biological risk factors for nonunion of bone fracture. JBJS Rev 2016;4:e5. [Google Scholar]
- 7.Zura R, Xiong Z, Einhorn T, Watson JT, Ostrum RF, Prayson MJ, et al. Epidemiology of fracture nonunion in 18 human bones. JAMA Surg 2016;151:e162775. [Google Scholar]
- 8.Del Pozo EG, Collazos J, Cartón JA, Camporro D, Asensi V. Bacterial osteomyelitis: microbiological, clinical, therapeutic, and evolutive characteristics of 344 episodes. Rev Esp Quimioter 2018;31:217-25. [Google Scholar]
- 9.Al-Zahrani S, Harding MG, Kremli M, Khan FA, Ikram A, Takroni T. Free fibular graft still has a place in the treatment of bone defects. Injury 1993;24:551-4. [Google Scholar]
- 10.Borrelli J, Prickett WD, Ricci WM. Treatment of nonunions and osseous defectz with bone graft and calcium sulfate. Clin Orthop Relat Res 2003;411:245-54. [Google Scholar]