Thorough pre-operative planning regarding implants, templating, bone grafting and surgical approach is paramount while fixing a poliotic bone.
Dr. Vivek Shetty, Department of Orthopaedics, P D Hinduja Hospital and MRC, Veer Savarkar Marg, Mahim (West), Mumbai - 400 016, Maharashtra, India. E-mail: vivshetty7777@gmail.com
Introduction:Although poliomyelitis is on the verge of eradication, the survivors of this disease are still living with its complications. Polio survivors with its musculoskeletal complications will continue to be a part of our population for many more decades’. Although poliomyelitis in itself is not common today, fractures in polio affected patients’ limbs are a common entity and are difficult to manage with common fracture management protocols.
Case Presentation: This study presenting a case of 58-year-old male with alleged history of twisting of the right lower limb while walking. X-rays suggested fracture right shaft femur. Patient had a history of poliomyelitis with the right lower limb affection and had a fixed flexion deformity of 15 at the right knee joint. The patient had to undergo two surgeries. In the first procedure, distal femur plating was done through lateral approach. Due to radiological signs of non-union, in the next procedure, additional medial plate was added and bone grafting was done to ensure stable fixation and union.
Conclusion:Treating a fracture in a polio affected limb is a challenging task taking into consideration the previous bony deformity as well as the myopathy. Knowledge of treating these fractures as well as pre-operative planning is important to a trauma surgeon as such scenarios are not very rare.
Keywords:Poliomyelitis, distal femur fracture, plating, bone grafting, PRPP.
Poliomyelitis was a rampant disease in India a few decades ago. In a study by Groce et al., it was found that the number of polio cases declined from 3,50,000 annual cases in 125 countries in 1988 to only 233 cases in three countries in 2012 [1]. However, some developing countries are still reporting new cases [1]. Patients with post-polio residual paralysis (PPRP) are still found in orthopedic clinics.
Poliomyelitis causes muscle atrophy and the sequelae causes bony deformity, thus reducing the stability and mobility, alters the gait pattern, and predisposes to falls [3]. The lower limb involvement in polio affects quadriceps, leading to weakness and buckling of knee in stance phase of the gait cycle, and thus is a risk factor for falls and fractures.
Failure to clear the foot off the ground during swing phase due to ankle dorsiflexor or hip flexor paralysis is another reason of falls and fractures in polio [3]. Bickerstaffe et al. in 2010 studied the frequency of fall in 305 polio subjects. They found that 74% had at least one fall in the past 1 year and 60% had two or more falls [3]. Poliomyelitis is also a risk factor for regional osteoporosis [4]. The incidence was up to 96% with reported fracture incidence of 38% [3]. The deformity with osteoporosis further increases the surgeon’s difficulties while fixation of such type of fractures.
A 58-year-old male with PPRP using a 5 cm shoe raise and an above knee ischial weight bearing caliper had a history of twisting injury to the right lower limb. Clinical examination revealed swelling, pain, and inability to bear weight. Radiographs showed the right distal third femur fracture with severe arthritic changes in the knee (Fig. 1).
Patient was taken up for surgical fixation with an interfragmentary screw and a 7-hole Distal Femoral Locking Plate (DFLP) as a neutralization plate through direct lateral approach in lateral position (Fig. 2). The osteophytes from the femoral condyles were used as bone graft at the fracture site. The difficulties and challenges faced during the surgery were the short size of femur due to short stature, fixed flexion deformity at the knee, and abnormal contour of the osteoporotic bone.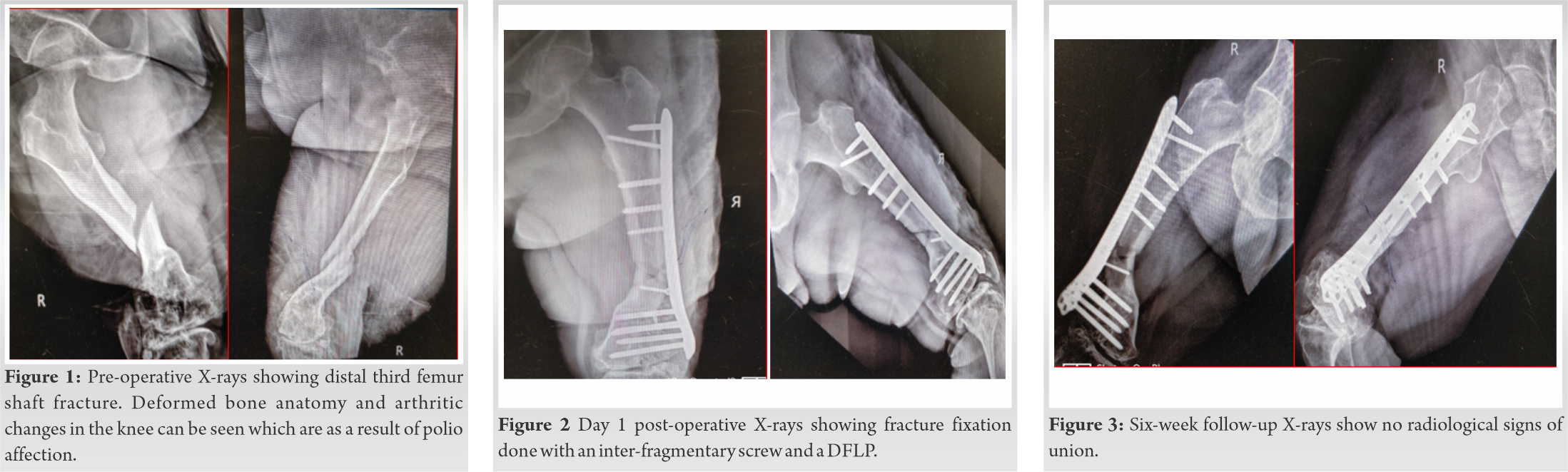
On follow-ups at interval of 6 weeks, at the end of 6 months (Fig. 3, 4), the fracture showed signs of non-union. A decision of supplementary fixation and bone grafting was made. Keeping the lateral plate in-situ, an additional pre-bent 4.5 narrow Dynamic Compression Plate (DCP) was applied on the medial side and bone grafting from the right iliac crest was done at the fracture non-union site (Fig. 5).
Patient was kept non-weight bearing for 6 weeks post the second surgery, following which gradual weight bearing was promoted as tolerated by the patient.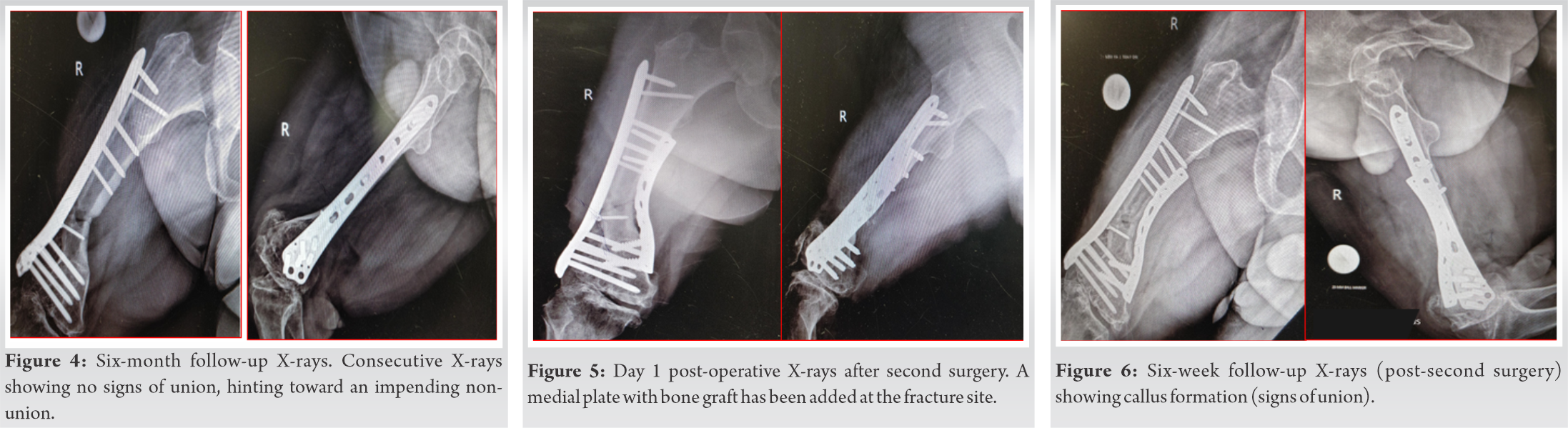
Follow-up X-rays at 6 weeks (Fig. 6) and 5 months (Fig. 7) post-second surgery showed good amount of callus and consolidation, proving that the intervention was a right decision. After 2½ years, the present X-rays (Fig. 8) show fracture completely consolidated and no implant-related problems. Patient is able to walk without support and without the caliper. He uses the same shoe raise and has good knee range of movements of 0–100o (Fig. 9). There are no pain or any other local complaints.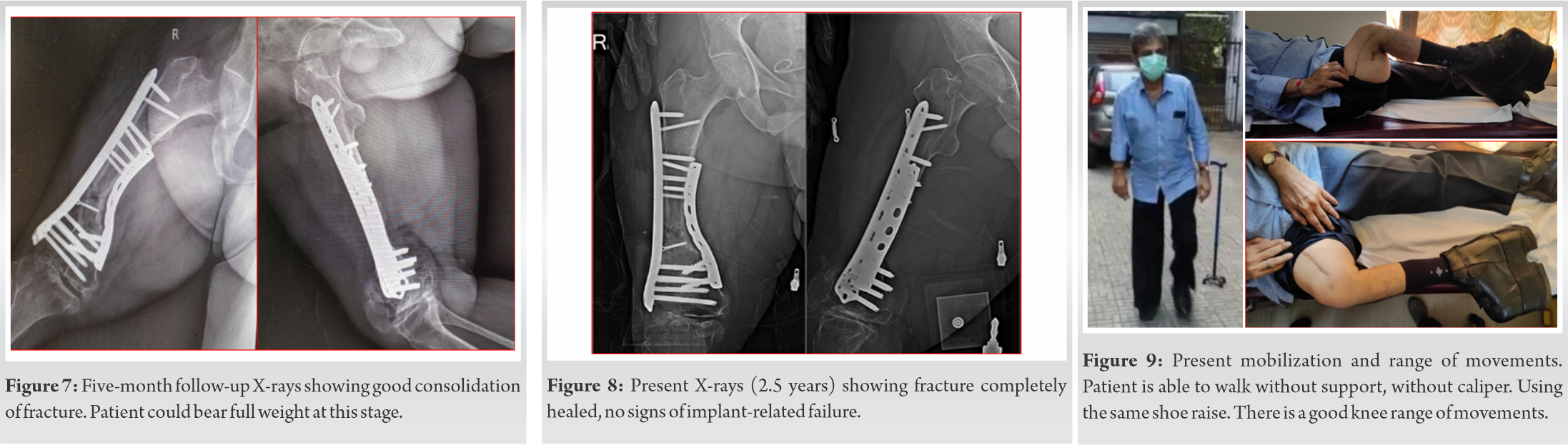
Poliomyelitis causes acute flaccid paralysis of the affected limb. This condition leads to wasting of the surrounding muscles as well as osteoporosis due to chronic disuse. A fracture in such a compromised and deformed limb leads to great challenges especially during fracture fixations.
Postoperatively, fracture healing is compromised due to low blood supply from the wasted peripheral muscles surrounding the fracture as was the case in our patient. Poor post-operative mobilization and compromised limb function cause a marked delay in healing and must be supplemented with bone grafts preferably in the index surgery.
However, the literature suggests that bone healing in certain active individuals with polio affected limbs is fairly normal [13]. The surgeon’s due vigilance and dedicated follow-up studies along with the knowledge of polio limb fracture management proved to be of great use in bringing out the final outcome. Because of deformed bone, narrow medullary canal, and knee flexion deformity, access to correct entry point and nail insertion would be difficult. In addition, positioning of the patient over a fracture table for nailing and applying traction is difficult because of flexion deformity at knee [16]. Locked compression plates are one of the gold standard treatment options in distal femur fractures [17] which was also proved to be true in poliotic distal femur fractures [7]. Since poor blood supply and bone healing capacity were anticipated, absolute stability rather than relative was given preference. Due to all these aforementioned reasons, extramedullary fixation in the form of plate was preferred over standard or custom made nails. Locking plates were preferred over non-locking plates as non-locking plates have a higher chance of failure because of osteoporosis, altered biomechanics due to asymmetrical muscle paralysis, and abnormal load applied on the deformed bone. The screw purchase in porotic bone is usually inadequate. Therefore, adequate number of screws should be applied on each side of fracture. In a study by El-Sayed Khalil in 2010, femur fractures of polio patients were fixed with locking plates successfully and only one out of 13 showed non-union after 28 weeks [15].
The problem faced during this case was that of contouring the plate to fit the altered bone anatomy [15], which could lead to plate weakening due to formation of stress risers and might also change the direction of the locking screws .Wei’Jun Wang et al. in 2013 concluded that LCP provides stable fixation of distal femur fractures in post-polio patients. Bony union and good functional outcomes were achieved with only one case showing delayed union [7]. Raju et al. in 2020 in a study of surgical fixations and the encountered challenges seen in the lower limb fractures of polio patients concluded having only one non-union out of 20 patients [16]. Given poor soft-tissue envelope and hypovascularized bone in a poliotic limb, soft-tissue handling is the key to fracture union. Furthermore, low contact plate was used to avoid contact necrosis. To minimize the chances of non-union in the primary surgery; the measures that could have been taken are: A more stable and rigid fixation and bone grafting.
One needs to anticipate the intraoperative problems in poliotic limb fractures. Furthermore, thorough pre-operative planning regarding the type of implants, pre-operative templating and pre-bending of the plates, bone grafting, and correct surgical approach are a must. Such cases prove that there is a need to have customized implants based on the bone geometry of such patients with short and deformed limbs. This could be done by computer assisted designing or 3D printing. Use of a navigation system for perfect implant positioning in a minimally invasive manner is another future possibility. A learning point from this case is that delayed union and even non-union should always be anticipated in all fractures in poliotic limbs as seen in this case; and precautions to avoid the same should be taken in the primary surgery itself. Another important point is to take the decision of early and appropriate intervention whenever in doubt of an impending non-union in such cases. It is also worth contemplating that precautionary bracing should be considered as treatment or preventive measure since post-polio patients are a high-risk group for fall and fractures [6, 9].
There can be various intra-operative challenges while treating fractures in a poliotic limb. Certain points that should be kept in mind during these surgeries are.
Pre-operative planning along with a thorough knowledge of poliotic surgeries is a must. Minimum soft-tissue stripping and devascularization should be practiced. Pre-bending of plates according to the altered anatomy of the poliotic limb should be considered to save the surgical time. Open reduction is preferred over closed reduction as we would want absolute stability in such fractures. Customized 3D printed implants, especially for the lower limb fractures, can be a future revolution. Fall prevention strategies should be implemented as a precautionary method in polio patients. Supplementary fixation and bone grafting to avoid non-union. Doing a pre-operative BMD is worth giving a thought.
References
- 1.Groce NE, Banks LM, Stein MA. Surviving polio in a post-polio world. Soc Sci Med 2014;107:171-8. [Google Scholar]
- 2.Bhandari N. After eradication: India’s post-polio problem. BMJ 2014;348:g2275. [Google Scholar]
- 3.Bickerstaffe A, Beelen A, Nollet F. Circumstances and consequences of falls in polio survivors. J Rehabil Med 2010;42:908-15. [Google Scholar]
- 4.Haziza M, Kremer R, Benedetti A, Trojan DA. Osteoporosis in a postpolio clinic population. Arch Phys Med Rehabil 2007;88:1030-5. [Google Scholar]
- 5.Genêt F, Schnitzler A, Mathieu S. Orthotic devices and gait in polio patients. Ann Phys Rehabil Med 2010;53:51-9. [Google Scholar]
- 6.Silver JK, Aiello DD. Polio survivors: Falls and subsequent injuries. Am J Phys Med Rehabil 2002;81:567-70. [Google Scholar]
- 7.Wang WJ, Shi HF, Chen DY. Distal femoral fractures in post-poliomyelitis patients treated with locking compression plates. Orthop Surg 2013;5:118-23. [Google Scholar]
- 8.Goerss JB, Atkinson EJ, Windebank AJ, O’Fallon WM, Melton LJ 3rd. Fractures in an aging population of poliomyelitis survivors: A community-based study in Olmsted County, Minnesota. Mayo Clin Proc 1994;69:333-9. [Google Scholar]
- 9.Mohammad AF, Khan KA, Galvin L, Hardiman O, O’Connell PG. High incidence of osteoporosis and fractures in an aging post-polio population. Eur Neurol 2009;62:369-74. [Google Scholar]
- 10.Chang KH, Lai CH, Chen SC. Femoral neck bone mineral density in ambulatory men with poliomyelitis. Osteoporos Int 2011;22:195-200. [Google Scholar]
- 11.Headley JL. More research about bisphosphonate treatment in polio survivors. Post Polio Health 2012;28:3. [Google Scholar]
- 12.Alvarez A, Kremer R, Weiss DR, Benedetti A, Haziza M, Trojan DA. Response of postpoliomyelitis patients to bisphosphonate treatment. PM R 2010;2:1094-103. [Google Scholar]
- 13.Onuba O. Outcome of limb fractures in poliomyelitis. Indian J Orthop 1986;20:214-6. [Google Scholar]
- 14.Naude RJ, Spencer RF. Late effects of poliomyelitis--a review of osteogenic capacity. S Afr Med J 1990;77:575-6. [Google Scholar]
- 15.El-Sayed Khalil A. Locked plating for femoral fractures in polio patients. Arch Orthop Trauma Surg 2010;130:1299-304. [Google Scholar]
- 16.Raju S, Singhi PK, Thangamani V, Muthu C. A study of surgical intervention in fractures of post-polio residual paralytic lower limb, challenges encountered, and outcome analysis. J Orth Joint Surg 2020;2:10-6. [Google Scholar]
- 17.Xing W, Lin W, Dai J, Kong Z, Wang Y, Sun L, et al. Clinical effect of locking compression plate via posterolateral approach in the treatment of distal femoral fractures: A new approach. J Orthop Surg Res 2018;13:57. [Google Scholar]










