While dealing with major bone fracture associated with vascular malformation a multispecialty approach should be consider.
Dr. S K Rai, Department of Orthopaedics, Base Hospital, Guwahati, Assam - 781029, India. E-mail: skrai47@yahoo.com
Introduction:Extremities arteriovenous malformations are uncommon vascular lesions that usually go unnoticed until a fracture occurs or imaged for other medical problems. The lesion is invariably quiescent, infiltrative in nature, and leads to the destruction of soft tissue and bone. Worldwide 20-30 % incidence of arteriovenous malformations has been noted in bones. This arteriovenous malformation greatly affects bone growth as compared to the normal side and leads to pathological fracture. However, few reports on the management of such pathologic fractures associated with AVM have been published in the literature. The main problem is to decide the types of implants and whether open or closed reduction. Here, we present a case series of pathologic femoral shaft fracture associated with multiple hemangiomas in the thigh that was treated successfully by minimally invasive distal femoral locking plate fixation and teriparatide.
Case presentation:We are describing our one index case. A 39-year-old woman, otherwise healthy, sustained a fall and developed a left femoral shaft fracture. At the time of admission, she had swelling and venous varicosities and non-itchy, blanchable violet patches over the left thigh. Plain radiography of the left thigh revealed Hypoplastic femoral shaft with a markedly obliterated medullary canal with distal 1/3 rd fracture with calcification of soft tissue. We planned open reduction and distal locking femoral plating because medullary canal was very small to accommodate intramedullary nail following embolization of the feeding artery. While performing open reduction, a considerable amount of bleeding (1300 ml) after incision of subcutaneous tissue occurred. After successful fracture fixation, union was achieved with administration of teriparatide 12 months postoperatively. At present patient is able to walk using elbow support.
KeywordsArteriovenous hemangiomas, pathological fracture femur, bleeding.
Arteriovenous hemangiomas are now known as arteriovenous malformations (AVMs), are uncommon congenital vascular lesions. Two forms exist firstly, vascular tumors (hemangiomas), and secondly, vascular malformations, according to The International Society for the Study of Vascular Anomalies. Latter is further divided into venous malformations, capillary malformations, lymphatic malformations, arteriovenous malformations (AVMs), and combined lesions. AVMs contain abnormal shunts between arteries and veins with high-flow malformations [1, 2]. AVMs most commonly occur in the extremities, facial bone, and pelvis and are usually goes unnoticed, which leads to late expansion and ultimately, infiltration and destruction of local soft tissue and bone [3]. AVMs can also lead to local bony changes by weakening them and finally pathologic fracture [4, 5, 6]. There are several treatment options for AVM, including conservative therapy with fitted pressure corticosteroids [7], garments systemic [8], embolization [9], radiation [10, 11], sclerotherapy [12], and surgical removal [13], or a combination of these modalities [14, 15]. The incidence of skeletal involvement especially long bones by AVM has been reported to be 20 to 31% [13, 16]. In the present literature, few reports on the management of pathologic fracture associated with AVM has been reported [5, 17, 18]. Teriparatide, a parathyroid hormone (PTH) analogue of PTH, which is used in treatment of osteoporosis [19]. Recently, many studies have shown its use in fracture healing [20, 21, 22]. Here, we present five cases of pathologic femoral shaft fracture associated with extensive AVMs that achieved fracture union using a minimally invasive distal femoral locking plate fixation and teriparatide therapy.
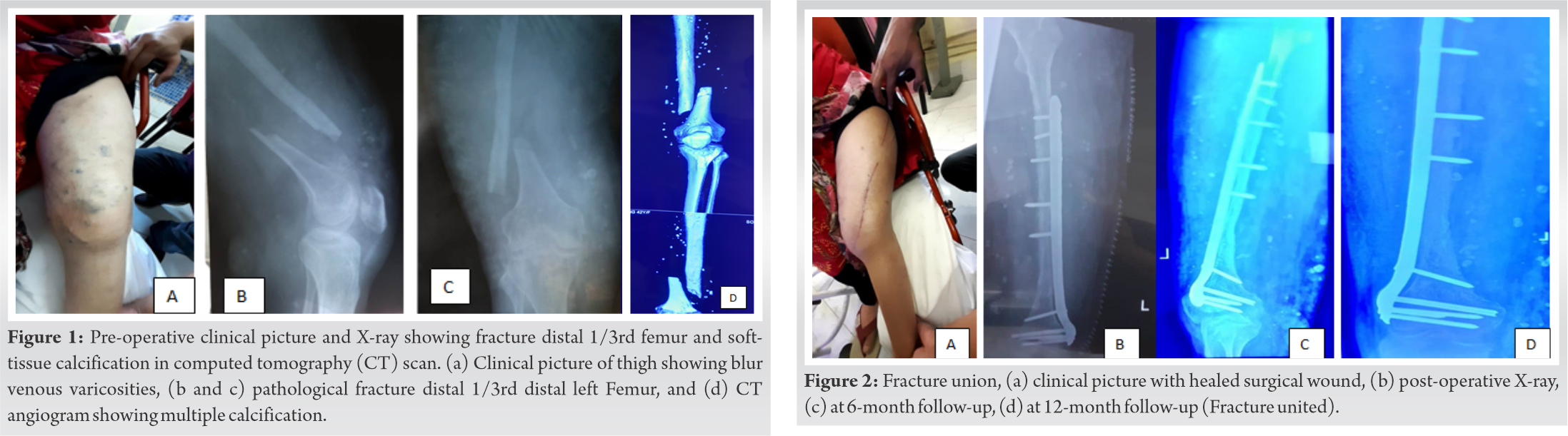
We are describing our one index case. A 39-year-old woman, otherwise healthy, sustained a fall and developed a fracture distal third femur shaft on the left side. At the time of admission, she had swelling and bluish venous varicosities and non-itchy, blanchable violet patches over mid, and distal aspect of the left thigh. Plain X-ray of the left thigh revealed hypoplastic femoral shaft with a markedly obliterated medullary canal with distal 1/3rd fracture with multiple soft-tissue calcification (Fig. 1). We planned open reduction and distal locking femoral plating because medullary canal was very small to accommodate intramedullary nail after feeding artery embolization. While performing open reduction, a considerable amount of bleeding (1300 mL) after incision from subcutaneous tissue took place and hemostasis was achieved. After successful fracture fixation, patient was put on inj teriparatide for 3 months and union was achieved with 12-month postoperatively. At present, patient is walking full weight bearing with the help of elbow support.
We present five cases of pathologic fracture with hypoplasia of bone and associated with extensive hemangiomas that achieved fracture union using limited open reduction and distal femoral locking plate fixation and supplementation with teriparatide.
Arteriovenous hemangiomas, often called arteriovenous malformations (AVMs), are a type of congenital vascular abnormality. The International Society for the Study of Vascular Anomalies described two forms first, vascular tumors known as (hemangiomas); and second, vascular malformations. Latter is further subdivided into capillary, venous, lymphatic, and AVMs. These abnormalities have erroneous shunts between arteries and veins [1, 2]. These lesions are commonly seen in extremities, facial bone and pelvis, and usually goes unnoticed, which leads to expansion, infiltration, and ultimately destroy underlying tissue and bone [3]. AVMs can also lead to local bony changes by causing improper growth and hypoplasia that weakens them and finally leads to pathologic fracture [4, 5, 6]. Many treatment modalities are available for AVM management, including non-surgical therapy like fitted pressure corticosteroids [7], garments systemic [8], embolization [9], radiation [10, 11], sclerotherapy [12], and surgical removal [13], or a combined approach [14, 15]. The incidence of skeletal involvement especially long bones by AVM has been reported to be 20 to 31% [13, 16]. In the existing literature, few similar cases reported on the management of pathologic fracture that coexisted with AVM [5, 17, 18]. Teriparatide is widely used in the treatment of osteoporosis [19]. Recently, many studies have shown its use in fracture healing as well [20, 21, 22]. We would like to present our experience of five cases of pathologic fracture of hypoplastic femur associated with extensive AVMs in which fracture union took place by limited open reduction and internal fixation by distal femoral locking plate and teriparatide therapy.
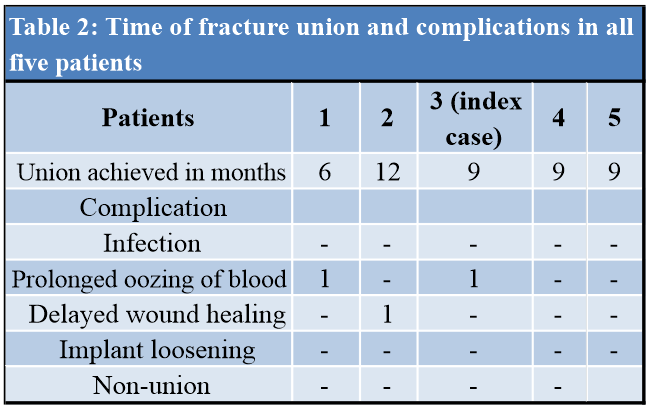
We managed five patients of AVMs with hypoplastic femur fracture between January 2005 and March 2019; details are shown in (Table 1). We are here describing one index case. A 39-year-old otherwise healthy woman sustained accidental fall and developed femur shaft fracture on the left side. On X-ray, she was detected to have a long-standing AVM in the left thigh with hypoplastic femur with a fracture. Before this recent injury, she was normal and was totally unaware of underlying AVMs. Three out of five patients were asymptomatic and unaware that they were having underlying AVMs in their thigh. However, two patients were aware of their AVMs as they were diagnosed in childhood. All included patients did not take any kind of medical or surgical treatment for AVMs.
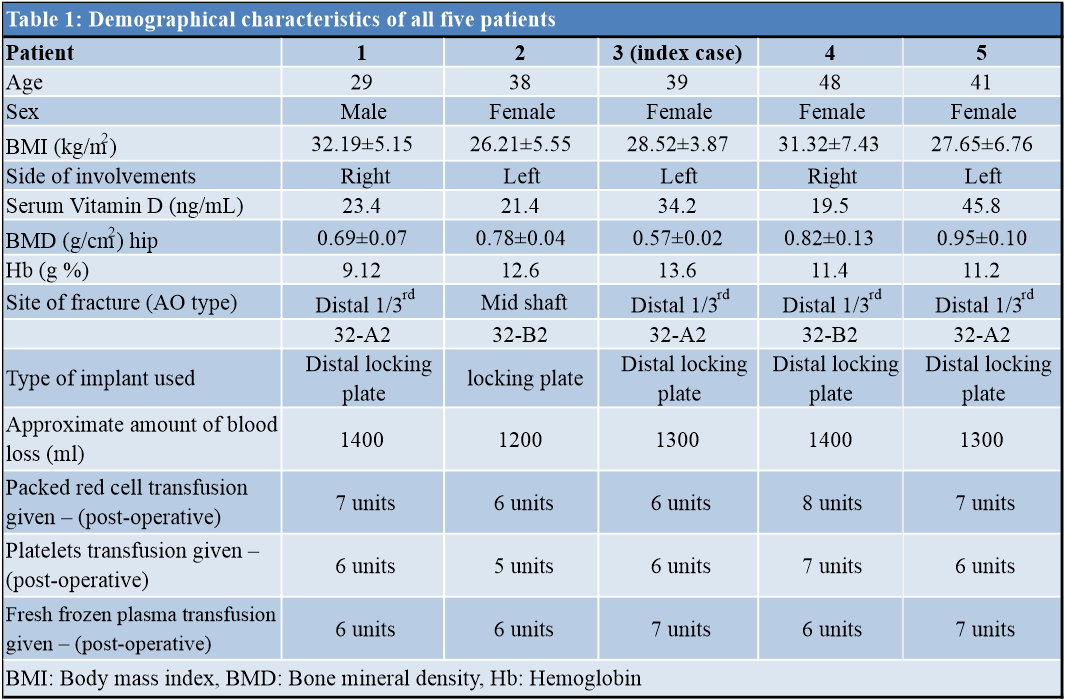
On arrival, in the emergence department, she had mild swelling and many light blue circular venous varicosities on the left thigh. The left thigh’s plain radiography revealed a fracture of distal 1/3rd of femoral shaft with the hypoplastic femur and numerous phleboliths (Fig. 1b and c). Computed tomography (CT) scan revealed extensive AVMs and phleboliths in the thigh muscles more in quadriceps femoris and vastus lateralis muscle along with hypoplastic and hypotrophied femur. The intramedullary canal of femur was also very narrow (Fig. 1b and c). CT angiography of thigh showed that the AVMs were fed by the multiple branches of the deep and superficial femoral artery. We planned open reduction and internal fixation by distal femoral locking plate by limited open reduction (Fig. 2a-d). Initially, feeding artery embolization was performed and on next day, she was taken for fracture fixation. Under spinal anesthesia, initially, closed reduction was tried but could not be achieved on the fracture table. Subsequently, we planned open reduction and internal fixation with titanium distal locking femoral plate; however, a considerable amount of bleeding (1300 mL) took place during the whole procedure. Total blood loss was 1300 mL, subsequently 6 units of packed RBC, 7 units of fresh-frozen plasma, and 6 units of platelet concentrate were administered. Patient was kept in the intensive care unit for close monitoring. All patients received IV antibiotics (Teicoplanin 400 mg 1 day before surgery and 4 days postoperatively thereafter).
Compressive stockinet was applied to all patients’ immediately after surgery and no suction drain was placed. Every patient was given IV Tranexamic acid 500 mg thrice a day for 5 days. Subcutaneous Teriparatide (20 μg daily) was given to each patient for 12-month postoperatively. Initially, non-weight-bearing walking was allowed using two axillary crutches for 3 months and then partial weight bearing walking for another 3 months and full weight-bearing walking thereafter. Follow-up X-ray was taken at 6, 9, and 12 months. In four patients, fracture union was achieved in 9 months, whereas it was 12 months in one patient (Table 2). We did not encounter any major complications in our series (Table 2).
Our case series demonstrates that hypoplastic and pathological fracture femur associated with extensive AVMs can be successfully treated by plate fixation using limited open reduction and administration of subcutaneous teriparatide. The problems in our series were presence of extensive AVMs in a wide area around thigh and the femur. For fracture fixation, a locking plate or IM nailing was required. We encountered two problems. First, intramedullary canal was significantly narrow to accommodate nail and second, risk of profound bleeding during open reduction and internal fixation. The ideal procedure would be a closed reduction and external fixation device, but this method is not always possible, especially in developing country and unavailability of desired hardware inventory. These AVMs are generally present at birth, progress silently and gradually, and manifest clinically later on with or without pain, ulceration, and swelling, a discrepancy in leg length, bleeding, and tortuous venous channels [13, 23]. Breugem et al. [13] reported that 18 (20%) had involvement of bone out of 90 patients with vascular malformations. They suggested that it should be treated with a multidisciplinary approach. They also noted that with intraosseous involvement, it affects bone growth and leads to local osteoporosis and possess risk of fracture. Surgical intervention is often associated with risk of profound bleeding, inadequate resection of lesion, and local recurrence. In the orthopedic literature, few authors reported on the management of these pathological fractures associated with AVM. Jończyk et al. [17] reported pathologic subtrochanteric fracture in a 19-year-old boy along with extensive AVM in same thigh and treated by embolization followed by closed reduction and intramedullary femoral nailing. Even with closed reduction patient had a risk of profound bleeding. Patient was given total 4 units of packed red blood cells transfusion. He noted fracture union in 9 months after surgery. Two authors have reported Klippel-Trenaunay syndrome (KTS) with fracture femur [24, 25]. Gupta et al. [25] reported that fracture shaft femur with KTS was treated by closed reduction and external fixator and fracture united in 4.5 months. Because of extensive AVM, there has been a constant risk of delayed union, refracture, and implant back out, due to very thin femoral cortex. If delayed union or non-union took place, it would be extremity challenging to perform the bone graft due to greater risk of excessive bleeding. To avoid such incidences, we initiated teriparatide therapy from 2nd weeks post-surgery. This is a recombinant PTH analog, widely used in management of osteoporosis [19, 20, 21, 22]. Borges et al. [26] reported accelerated fracture healing after teriparatide therapy in an 84-year-old woman with a trochanteric fracture. Kim et al. [20] in a systemic review evaluated the role of teriparatide in fracture union in osteoporotic patients. Huang et al. [22] reported rapid fracture healing after teriparatide therapy in trochanteric fracture. Since teriparatide has definite role in healing of fracture as noted by many authors, we believe that in pathologic fracture with a hypotrophic and thin femoral cortex, it also helps in fracture union in a stipulated time frame.
We managed five cases of pathologic fracture femur shaft coexisted with extensive AVMs. Fracture union was achieved by limited open reduction distal femoral locking plate fixation and teriparatide. Although treatment of hypoplastic bone with pathologic fracture due to AVM possess many challenges, a minimally invasive method of fracture fixation would be ideal, sometimes it may not be available. However, a limited open reduction and distal femoral locking plate fixation can be an alternative method for fracture fixation along with multidisciplinary support for the favorable outcome.
The management of extensive AVMs with fracture femur poses great challenges for young orthopedic surgeons, especially with limited hardware/implant availability. As far as possible closed reduction and minimally invasive fracture fixation method should be chosen. The multidisciplinary approach, which involves interventional radiologist and vascular surgeon with good blood component support, is essential for a favorable outcome.
References
- 1.Dasgupta R, Fishman SJ. ISSVA classification. In: Seminars in Pediatric Surgery. Vol. 23: WB Saunders; 2014. p. 158-61. [Google Scholar]
- 2.Merrow AC, Gupta A, Patel MN, Adams DM. 2014 revised classification of vascular lesions from the International Society for the Study of Vascular Anomalies: Radiologic-pathologic update. Radiographics 2016;36:1494-516. [Google Scholar]
- 3.Marler JJ, Mulliken JB. Current management of hemangiomas and vascular malformations. Clin Plast Surg 2005;32:99-116, ix. [Google Scholar]
- 4.López-Gutiérrez JC, García-Miguel P. Skeletal hemangiomas and vascular malformations. J Pediatr Hematol Oncol 2006;28:634. [Google Scholar]
- 5.Takeuchi A, Matsubara H, Yamamoto N, Hayashi K, Miwa S, Igarashi K, et al. Successful treatment of pathologic femoral shaft fracture associated with large arteriovenous malformations using a 3-dimensional external fixator and teriparatide: A case report. BMC Surg 2019;19:35. [Google Scholar]
- 6.Ayhan S, Palaoglu S, Geyik S, Saatci I, Onal MB. Concomitant intramedullary arteriovenous malformation and a vertebral hemangioma of cervical spine discovered by a pathologic fracture during bicycle accident. Eur Spine J 2015;24:187-92. [Google Scholar]
- 7.Richter GT, Friedman AB. Hemangiomas and vascular malformations: Current theory and management. Int J Pediatr 2012;2012:645678. [Google Scholar]
- 8.Hein KD, Mulliken JB, Kozakewich HP, Upton J, Burrows PE. Venous malformations of skeletal muscle. Plast Reconstr Surg 2002;110:1625-35. [Google Scholar]
- 9.Do YS, Park KB, Park HS, Cho SK, Shin SW, Moon JW, et al. Extremity arteriovenous malformations involving the bone: Therapeutic outcomes of ethanol embolotherapy. J Vasc Interv Radiol 2010;21:807-16. [Google Scholar]
- 10.Plowman PN. Radiation therapy and vascular malformations. In: Endovascular Neurosurgery. London: Springer; 2000. p. 139-55. [Google Scholar]
- 11.Brahmbhatt AN, Skalski KA, Bhatt AA. Vascular lesions of the head and neck: An update on classification and imaging review. Insights Imaging 2020;11:19. [Google Scholar]
- 12.Mishra M, Singh G, Gaur A, Tandon S, Singh A. Role of sclerotherapy in management of vascular malformation in the maxillofacial region: Our experience. Natl J Maxillofac Surg 2017;8:64-9. [Google Scholar]
- 13.Breugem CC, Maas M, Breugem SJ, Schaap GR, van der Horst CM. Vascular malformations of the lower limb with osseous involvement. J Bone Joint Surg Br 2003;85:399-405. [Google Scholar]
- 14.Igari K, Kudo T, Toyofuku T, Jibiki M, Inoue Y. Multidisciplinary approach to a peripheral arteriovenous malformation. EJVES Extra 2012;23:e11-3. [Google Scholar]
- 15.Yu X, Nie T, Zhang B, Dai M, Liu H, Zou F. Misdiagnosis of pathological femoral fracture in a patient with intramuscular hemangioma: A case report. Oncol Lett 2016;12:195-8. [Google Scholar]
- 16.Madani H, Farrant J, Chhaya N, Anwar I, Marmery H, Platts A, et al. Peripheral limb vascular malformations: An update of appropriate imaging and treatment options of a challenging condition. Br J Radiol 2015;88:20140406. [Google Scholar]
- 17.Jończyk J, Szubert W, Panasiuk M. Pathological subtrochanteric femoral fracture due to extensive arterio-venous malformation. A case study. Ortop Traumatol Rehabil 2015;17:297-303. [Google Scholar]
- 18.Mnaymneh W, Vargas A, Kaplan J. Pathologic fracture of the clavicle caused by arteriovenous malformation. Clin Orthop Relat Res 1980;???:256-8. [Google Scholar]
- 19.Body JJ, Gaich GA, Scheele WH, Kulkarni PM, Miller PD, Peretz A, et al. A randomized double-blind trial to compare the efficacy of teriparatide [recombinant human parathyroid hormone (1-34)] with alendronate in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 2002;87:4528-35. [Google Scholar]
- 20.Kim SM, Kang KC, Kim JW, Lim SJ, Hahn MH. Current role and application of teriparatide in fracture healing of osteoporotic patients: A systematic review. J Bone Metab 2017;24:65-73. [Google Scholar]
- 21.Babu S, Sandiford NA, Vrahas M. Use of Teriparatide to improve fracture healing: What is the evidence? World J Orthop 2015;6:457-61. [Google Scholar]
- 22.Huang TW, Chuang PY, Lin SJ, Lee CY, Huang KC, Shih HN, et al. Teriparatide improves fracture healing and early functional recovery in treatment of osteoporotic intertrochanteric fractures. Medicine (Baltimore) 2016;95:e3626. [Google Scholar]
- 23.Lam K, Pillai A, Reddick M. Peripheral arteriovenous malformations: Classification and endovascular treatment. Appl Radiol 2017;46:15-22. [Google Scholar]
- 24.Tsaridis E, Papasoulis E, Manidakis N, Koutroumpas I, Lykoudis S, Banos A, et al. Management of a femoral diaphyseal fracture in a patient with Klippel-Trenaunay-Weber syndrome: A case report. Cases J 2009;2:8852. [Google Scholar]
- 25.Gupta Y, Jha RK, Karn NK, Sah SK, Mishra BN, Bhattarai MK. Management of femoral shaft fracture in klippel-trenaunay syndrome with external fixator. Case Rep Orthop 2016;2016:8505038. [Google Scholar]
- 26.Borges JL, Freitas A, Bilezikian JP. Accelerated fracture healing with teriparatide. Arq Bras Endocrinol Metabol 2013;57:153-6. [Google Scholar]