To appreciate the role of MCP arthroplasty in JRA and compare/contrast silastic arthroplasty and pyrocarbon arthroplasty.
Dr. Marco Rizzo, Department of Orthopedic Surgery, Mayo Clinic, Rochester, Minnesota, United States. E-mail: rizzo.marco@mayo.edu
Introduction: Juvenile idiopathic arthritis (JIA) is an inflammatory arthritis of childhood that can lead to pain and dysfunction of the hands. In severe progressive cases, in which medical treatment does not result in symptom improvement, limited options are available. Metacarpophalangeal (MCP) joint arthroplasty remains a standard surgical treatment for inflammatory arthritis of the MCPmetacarpophalangeal joints in adults; however, no reports exist about its use in children or for JIA.
Case Presentation:We present two cases of MCP joint arthroplasty in patients with severe progressive JIA. The first patient presented at 21 years old with increasing pain and limited use of her right hand and underwent MCP arthroplasty using a pyrocarbon implant. The second patient presented at 14 years old with severe pain, contractures, subluxations, and the inability to use her right hand, subsequently undergoing MCP replacement with a silicone-based implant. The joint replacements resulted in pain relief and improvement of hand function for both patients, though the pyrocarbon implants had poor radiographic outcomes at 7 years follow- up, while the silicone implants had limited functional improvement.
Conclusions:MCPMetacarpophalangeal joint replacement may be considered in patients with severe inflammatory arthritis to relieve pain and/or to extend functional use of the fingers and hands. In these cases, silicone arthroplasty radiographically fared better than pyrocarbon.
Keywords:Metacarpophalangeal, arthroplasty, arthritis, juvenile.
Juvenile idiopathic arthritis (JIA) is the most common chronic rheumatic disease of childhood [1]. JIA encompasses a group of arthritides that are distinct from adult arthritic disease, requiring onset before 16 years of age and greater than 6 weeks duration [1]. In Europe and North America, its incidence and prevalence have been reported between 2–20 and 16–150 per 100,000, respectively [1]. One study noted that the most frequent joints involved are the knees, ankles, and elbows, followed by wrist and metacarpophalangeal (MCP) joint at 24% and 21% involvement, respectively [2]. By 5 years, MCP joint involvement had increased to 38% [2].
Conservative management of JIA includes medications, splinting, and corticosteroid injections [3]. If patients are resistant to traditional therapy with methotrexate, biologic therapy is attempted [3]. Frequently JIA can be controlled with just these steps and can even result in remission early in life [1, 3]. However, in some patients, the destructive process can progress, greatly impacting quality of life and ability to function. In this population, surgical intervention with MCP joint arthroplasty may serve as an alternative treatment to relieve pain and improve hand function. While there have been a number of studies on MCP joint replacement in osteoarthritis and rheumatoid arthritis of adults, there are none that discuss outcomes of MCP joint replacement in this population. A literature review showed that total joint replacement in patients with JIA can have good survival at 10 years, but has high rates of revision, as would be expected in young patients. In this article, we present two cases of patients with JIA involving the MCP joint treated with arthroplasty with greater than 5 years follow-up.
Case Report 1
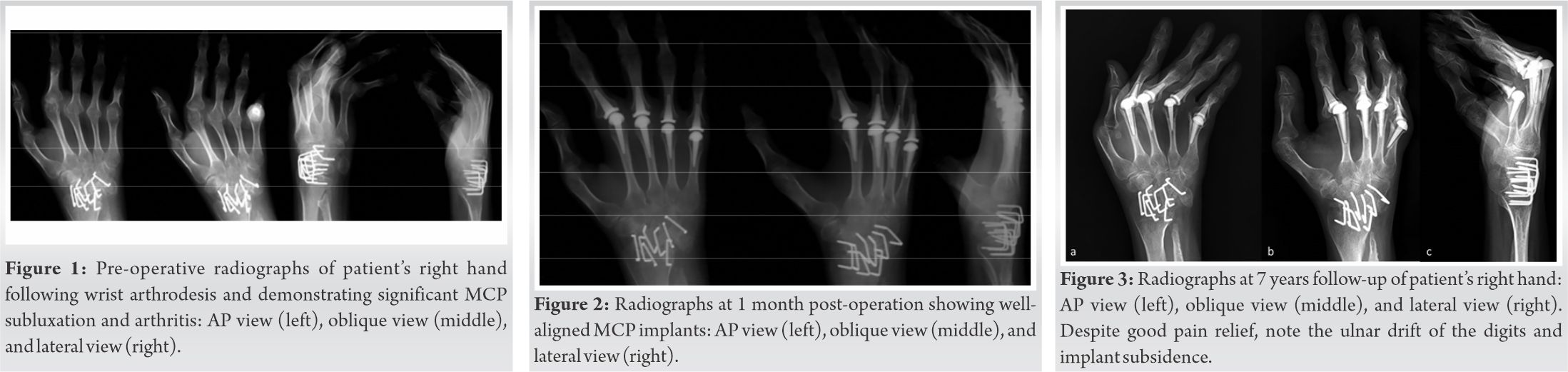
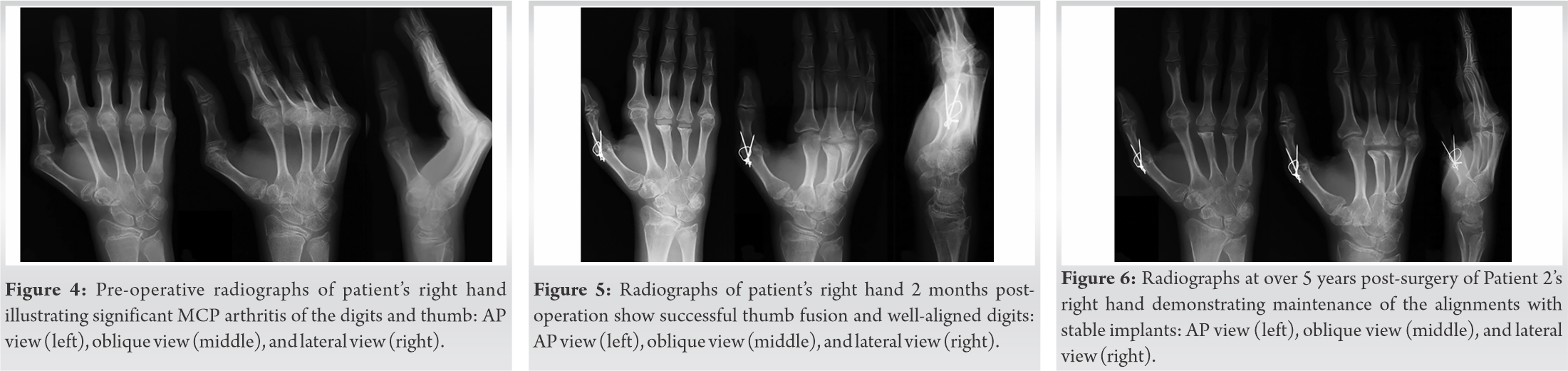
A 21-year-old right-handed female with history of JIA involving the knees, ankles, wrists, and hands presented with increasing pain and limited use of her right fingers. She began having symptoms at 6 years old affecting bilateral knees and ankles and was formally diagnosed at 9 years old. Initially, she was treated with methotrexate and hydroxychloroquine. She also had intra-articular corticosteroid injections performed to both knees. She, later, developed severe progressive disease in her wrists and hands requiring bilateral wrist fusions 11 years after diagnosis. Her disease progressed to affect her right hand MCP joints resulting in significant pain and deformity (Fig. 1). She failed splinting and conservative treatment and went on to have total arthroplasty of her index through small finger MCP joints. A dorsal surgical approach was used to centralize the extensor tendon and rebalance the soft tissues, followed by MCP arthroplasty of joints 2 through 5 (Fig. 2). After approximately 3 weeks of immobilization, the patient graduated to an MCP extension resting splint and started hand therapy. The ROM initially improved, as shown in Table 1, followed by a later decrease in the long and ring finger ROM.
The patient was followed for 7 years after the surgery requiring no reoperation or revision. At final follow-up, the patient had finished school and worked as a receptionist for 5 years before becoming a stay-at-home mom. Her post-operative course was free of clinical complications. However, radiographically her findings are worrisome with significant subsidence and recurrent deformity (Fig. 3). Overall, clinically she remains satisfied with her hands as they allowed her to retain most of her daily activities.
Case Report 2
The second patient was a 14-year-old right-handed female with a 9-year history of JIA manifested by pain and decreased ROM in her wrists, MCP joints of both hands, and elbows. The patient presented with increasing flexion contractures of the MCP joints of the right hand as well as volar subluxation of all five fingers of the right hand (Fig. 4). She had taken methotrexate and naproxen since age 7; however, at this time, she had been off her medication for 3 months. Besides contractures, she also lacked fingertip pinch, causing her to hold pens across the mid-portion of the palm while at school. While she maintained coronal plane alignment of her digits, she had notable subluxation and flexion contractures of the MCP joints. Due to the flexion contractures and increasing difficulty with activities of daily living (ADL), the decision was made to proceed with intrinsic muscle releases, capsular releases, and synovectomies of MCPs 2 through 5 on the right hand and possible arthroplasty (depending on intraoperative findings), with right thumb MCP synovectomy versus arthrodesis. A dorsal surgical approach was used for all fingers. Intraoperatively, there was complete loss of articular cartilage of the long and ring fingers, and silicone MCP arthroplasties were utilized for those joints. The index and little fingers had sufficient articular cartilage, so they received intrinsic muscle releases, capsular release, synovectomies, and temporary pinning of the MCP joints. The thumb also had complete loss of the articular cartilage and, therefore, proceeded with a fusion of the MCP joint of the thumb (Fig. 5). Postoperatively, a dorsal outrigger with extension slings to the thumb and fingers was used as well as a resting night splint to hold her fingers in neutral extension, though she did not use them consistently. Hand therapy was performed twice a day for 2 weeks beginning 2 weeks after surgery. At final follow-up, the patient reported that her pain was greatly reduced, though her function in prehensile pinch and grip only improved slightly, with thumb abduction interval increasing from 3.0 cm to 4.5 cm. The patient’s ROM improved over time, as shown in (Table 1). Extension was improved but not fully. She otherwise had revision-free survival of the implant for 5.2 years of follow-up after the surgery and did not develop any complications (Fig. 6).
Given the rare nature, no studies exist on the outcomes of MCP joint arthroplasty in this population. The previous literature has described the successful use of MCP joint arthroplasty in other inflammatory arthritides (e.g., rheumatoid arthritis); however, typically in older patients. Chung et al. found significant functional and ROM improvement in MCP joints after arthroplasty, with improvements in Michigan Hand Outcomes Questionnaire function and ADL scores of 23 and 16 points, respectively [4]. Studies have also reported a 20–34 degree improvement in ulnar deviation and 9 degree improvement in arc of motion at the MCP joint [4, 5] However, silicone-based implants have a rate of fracture around 9–10% in larger-sized studies, though higher rates have been reported [4, 5]. Kirschenbaum et al. followed patients for an average of 8.5 years and had a revision rate of 2–3% [5], while Chung et al. reported the same revision rate during a 3 year follow-up study [4]. Although direct comparison is not possible to these studies, the patients in our study also experienced improvement in range of motion and reasonable implant survival.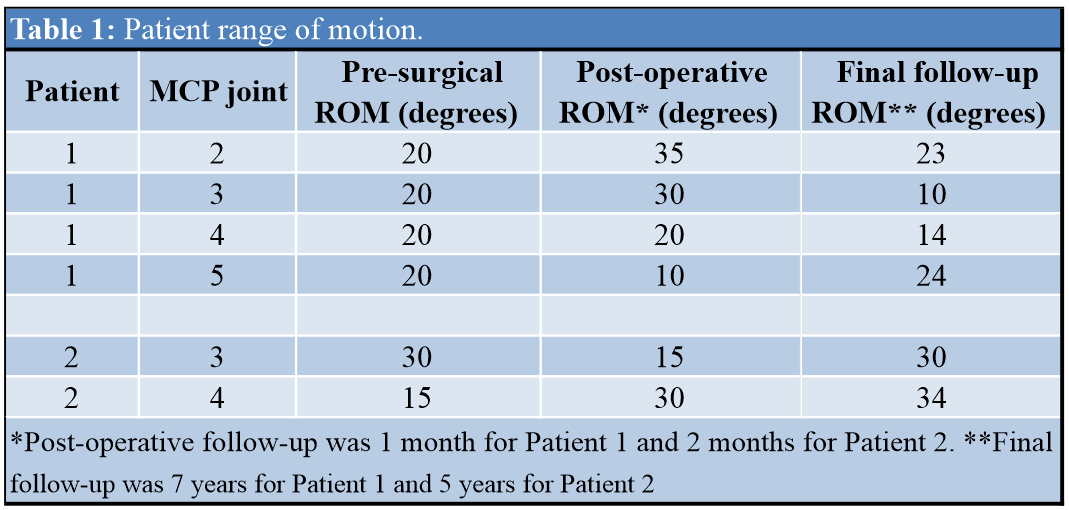
Medical treatment commonly results in improvement or remission of JIA; however, in rare cases, surgical treatment may be necessary. These two cases demonstrate successful treatment of JIA with MCP joint arthroplasty, improving pain, and function. Silicone implants fared better radiographically but had limited functional improvement compared to pyrocarbon, though more studies would be necessary to identify, in which implant provides better outcomes for this population. Recognizing the limitations and risks with arthroplasty in young patients, we do not recommend that MCP joint arthroplasty should be routinely performed; however, in cases that are recalcitrant to medical and conservative treatment, MCP arthroplasty may be considered a viable option to improve pain and function.
In patients with severe JIA, MCP joint arthroplasty can relieve pain and improve functional use of the hands. At minimum 5.2 years follow-up, silastic implants fared better radiographically than pyrocarbon implants.
References
- 1.Ravelli A, Martini A. Juvenile idiopathic arthritis. Lancet 2007;369:767-78. [Google Scholar]
- 2.Hemke R, Nusman CM, Van der Heijde DM, Doria AS, Kuijpers TW, Maas M, et al. Frequency of joint involvement in juvenile idiopathic arthritis during a 5-year follow-up of newly diagnosed patients: Implications for MR imaging as outcome measure. Rheumatol Int 2015;35:351-7. [Google Scholar]
- 3.Giancane G, Alongi A, Ravelli A. Update on the pathogenesis and treatment of juvenile idiopathic arthritis. Curr Opin Rheumatol 2017;29:523-9. [Google Scholar]
- 4.Chung KC, Burns PB, Kim HM, Burke FD, Wilgis EF, Fox DA. Long-term followup for rheumatoid arthritis patients in a multicenter outcomes study of silicone metacarpophalangeal joint arthroplasty. Arthritis Care Res (Hoboken) 2012;64:1292-300. [Google Scholar]
- 5.Kirschenbaum D, Schneider LH, Adams DC, Cody RP. Arthroplasty of the metacarpophalangeal joints with use of silicone-rubber implants in patients who have rheumatoid arthritis. Long-term results. J Bone Joint Surg Am 1993;75:3-12. [Google Scholar]
- 6.Baghdadi YM, Jacobson JA, Duquin TR, Larson DR, Morrey BF, Sanchez-Sotelo J. The outcome of total elbow arthroplasty in juvenile idiopathic arthritis (juvenile rheumatoid arthritis) patients. J Shoulder Elbow Surg 2014;23:1374-80. [Google Scholar]
- 7.Cross MB, Cicalese E, Nam D, McArthur BA, Lipman JD, Figgie MP. Results of custom-fit, noncemented, semiconstrained total elbow arthroplasty for inflammatory arthritis at an average of eighteen years of follow-up. J Shoulder Elbow Surg 2014;23:1368-73. [Google Scholar]
- 8.Ibrahim EF, Rashid A, Thomas M. Linked semiconstrained and unlinked total elbow replacement in juvenile idiopathic arthritis: A case comparison series with mean 11.7-year follow-up. J Shoulder Elbow Surg 2017;26:305-13. [Google Scholar]
- 9.Heyse TJ, Ries MD, Bellemans J, Wright TM, Lipman JD, Figgie MP, et al. Total knee arthroplasty in patients with juvenile idiopathic arthritis. Clin Orthop Relat Res 2014;472:147-54. [Google Scholar]
- 10.Buchheit J, Serre A, Bouilloux X, Puyraveau M, Jeunet L, Garbuio P. Cementless total knee arthroplasty in chronic inflammatory rheumatism. Europ J Orthop Surg Traumatol 2014;24:1489-98. [Google Scholar]
- 11.Swarup I, Lee YY, Christoph EI, Mandl LA, Goodman SM, Figgie MP. Implant survival and patient-reported outcomes after total hip arthroplasty in young patients with juvenile idiopathic arthritis. J Arthroplasty 2015;30:398-402. [Google Scholar]
- 12.Daurka JS, Malik AK, Robin DA, Witt JD. The results of uncemented total hip replacement in children with juvenile idiopathic arthritis at ten years. J Bone Joint Surg Br 2012;94:1618-24. [Google Scholar]
- 13.Cruz-Pardos A, Garcia-Rey E, Garcia-Cimbrelo E, Ortega-Chamarro J. Alumina-on-alumina THA in patients with juvenile idiopathic arthritis: A 5-year followup study. Clin Orthop Relat Res 2012;470:1421-30. [Google Scholar]
- 14.Jolles BM, Bogoch ER. Juvenile arthritis patients report favorable subjective outcomes of hip arthroplasty despite poor standard outcome scores. J Arthroplasty 2012;27:1622-28. [Google Scholar]