This case represents a unique presentation and operative technique for the treatment of an incarcerated greater tuberosity fracture.
Dr. Imran Gruhonjic, SSM Health St. Anthony Hospital, Oklahoma City, Oklahoma, United States. E-mail: imran.gruhonjic@ssmhealth.com
Introduction: Proximal humerus fractures are common injuries of the upper extremity. These fractures are frequent in the elderly population due to low-energy trauma and in the younger patient secondary to high-energy trauma that is associated with shoulder dislocations. Proximal humerus fractures are frequently classified according to the Neer classification which is defined by the number of segments and the amount displacement required to define the fracture as displaced. Segments include the greater tuberosity (GT), the lesser tuberosity, the humeral head, and the humeral shaft. Fractures are considered displaced if there is at least 45° of angulation or 1 cm of displacement.
Case Report: We present a case of a 42-year-old Caucasian patient with a displaced and incarcerated GT avulsion fracture following a motorcycle accident. In this report, we describe the patient positioning, technique using open reduction internal fixation utilizing multiple anchors and suture to treat this injury and the successful outcome of our patient 1 year from the injury.
Conclusion:While standard open reduction internal fixation techniques using plates and screws are appropriate for treating these injuries, we chose to pursue a method that involved only bio-absorbable suture anchors. Using these anchors, we were able to achieve an anatomic reduction of the GT fragment that ultimately went on to achieve full healing.
Keywords:Proximal humerus fracture, motorcycle, greater tuberosity avulsion, suture anchors, trauma evidence: Level V.
Proximal humerus fractures are common injuries of the upper extremity. These injuries are the seventh most frequent fracture in adults, and the third in patients over 65 years of age [1]. Their prevalence ranges from 4% to 10% of all fractures [2]. They are generally considered osteoporotic fractures occurring in the elderly population as a result of low-energy trauma and are reported to be more common in females than males with a 4:1 ratio over the age of 50 [3]. In contrast to the elderly, low energy, proximal humerus fracture, and isolated greater tuberosity (GT) fractures occur more commonly in the younger patient secondary to high-energy trauma. Two mechanisms of injury which can result in isolated GT fractures include direct impaction and shearing forces. Impaction injury could occur from direct impact to the area or fall on a hyperabducted shoulder causing the GT to impact the acromion or superior glenoid [4]. Shearing type injury with resulting GT fracture occurs secondary to anterior glenohumeral dislocation. GT fractures have been found in 15%–30% of anterior glenohumeral dislocations [5].
Proximal humerus fractures generally are classified by the Neer classification which is defined by the number of segments and the amount displacement required to define the fracture as displaced. Segments include the GT, the lesser tuberosity, the humeral head, and the humeral shaft. Fractures are considered displaced if there is at least 45° of angulation or 1 cm of displacement [6]. The GT, however, tolerates less displacement. More recent literature suggests that fractures with >3 mm of displacement in the athlete and overhead worker and with displacement of more than 5 mm in the active patient be treated surgically [7, 8]. The primary goal of operative fixation is to restore mechanical function of the attached rotator cuff and decrease risk of impingement with range of motion.
This is a case report of a 42-year-old male who presented to our ED after being involved in a motorcycle accident. He sustained a left GT avulsion fracture. The fracture fragment was retracted to the level of the glenohumeral joint which indicated that the rotator cuff muscles were still attached and functional (Fig. 1).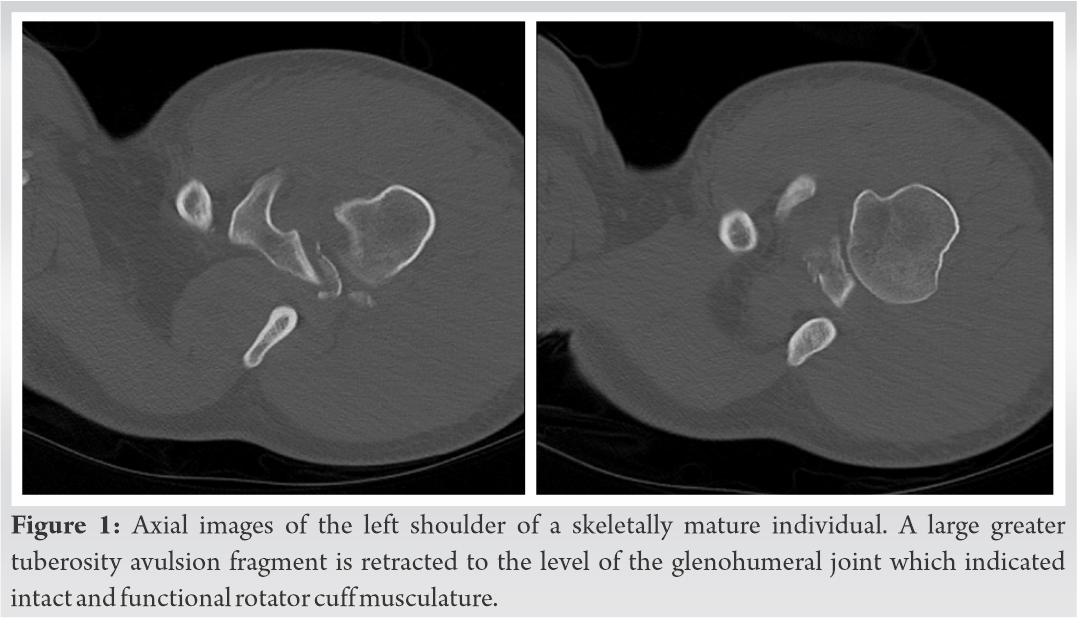 After non-operative versus operative treatment options were discussed with the patient, it was decided to proceed with open reduction internal fixation to give the patient the greatest chance of range of motion recovery. A standard deltopectoral approach was utilized. The avulsed GT fracture with attached rotator cuff was identified. Two 4.75 mm Arthrex anchors with associated FiberWire (Arthrex) were placed in the footprint of the GT (Fig. 2).
After non-operative versus operative treatment options were discussed with the patient, it was decided to proceed with open reduction internal fixation to give the patient the greatest chance of range of motion recovery. A standard deltopectoral approach was utilized. The avulsed GT fracture with attached rotator cuff was identified. Two 4.75 mm Arthrex anchors with associated FiberWire (Arthrex) were placed in the footprint of the GT (Fig. 2). 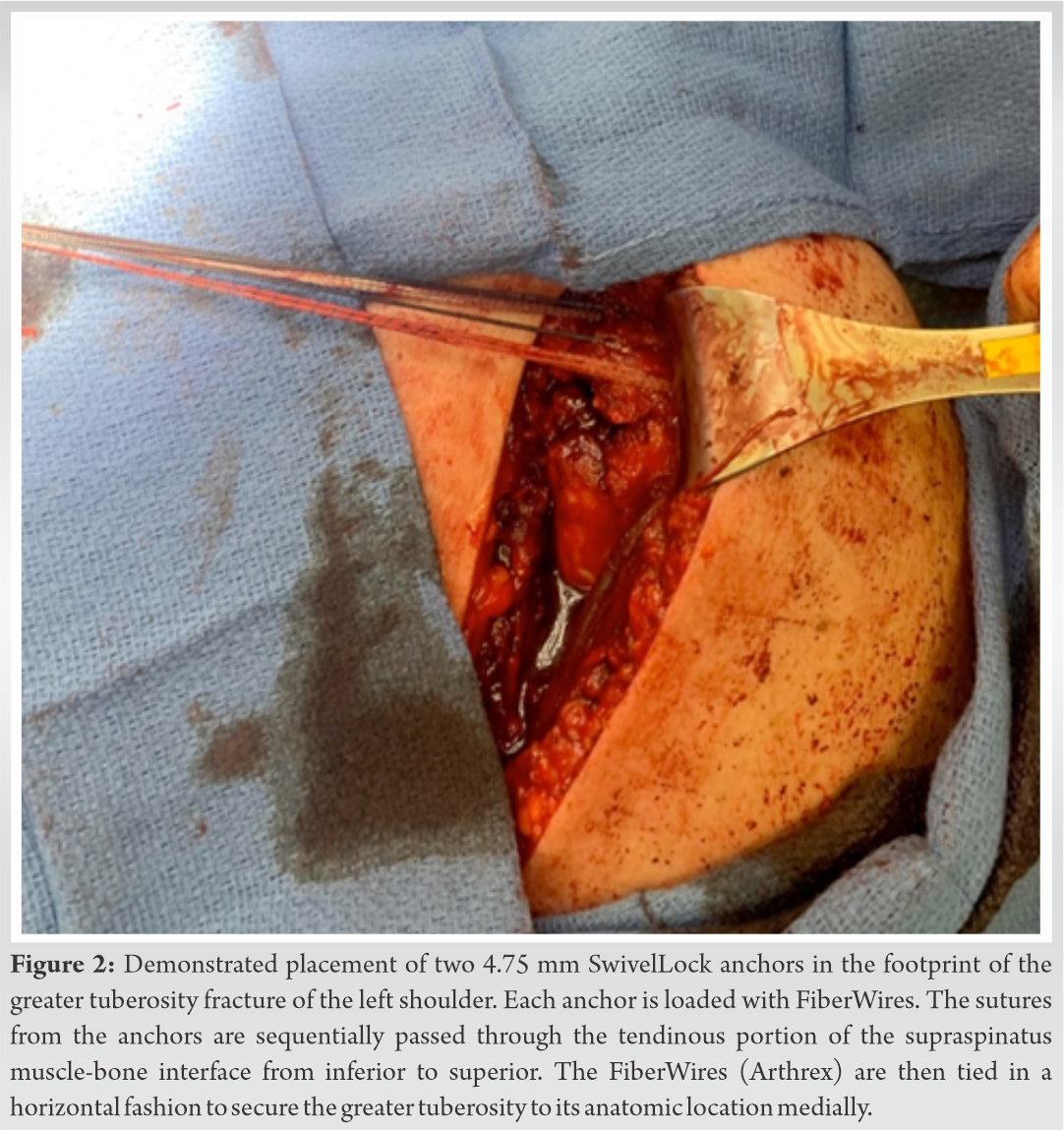 The sutures were then sequentially passed through the tendinous portion of the supraspinatus muscle-bone interface from inferior to superior. The FiberWires (Arthrex) were then tied in a horizontal fashion to secure the lesser tuberosity to its anatomic location medially. Next, the FiberWires were placed laterally into two separate anchors for further compression (Fig. 3).
The sutures were then sequentially passed through the tendinous portion of the supraspinatus muscle-bone interface from inferior to superior. The FiberWires (Arthrex) were then tied in a horizontal fashion to secure the lesser tuberosity to its anatomic location medially. Next, the FiberWires were placed laterally into two separate anchors for further compression (Fig. 3).  Postoperatively, the patient was placed in a shoulder immobilizer. He underwent early pendulum exercises followed by rotator cuff repair protocol. At the last follow-up, 8 months postoperatively, he had 140° of active forward flexion and 20° of external rotation and radiographs showed fully healed fracture fragments (Fig. 4).
Postoperatively, the patient was placed in a shoulder immobilizer. He underwent early pendulum exercises followed by rotator cuff repair protocol. At the last follow-up, 8 months postoperatively, he had 140° of active forward flexion and 20° of external rotation and radiographs showed fully healed fracture fragments (Fig. 4).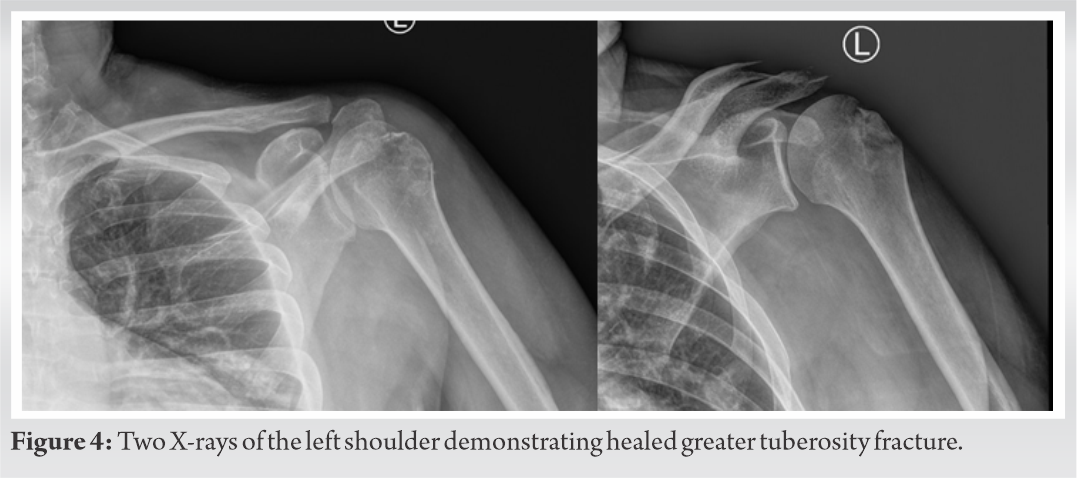
Our report presents a case of an isolated GT fracture with an intact rotator cuff, incarcerated in the glenohumeral joint following a motor vehicle accident. Proximal humerus fractures are common orthopedic injuries. Within this, GT fractures make up a small portion [4]. Roughly, 19% of all proximal humerus fractures are isolated GT fractures [9]. Typically, fractures in this region occur through the physeal lines and 5% to 57% can be associated with dislocation [10]. As there are many muscles that can act as deforming forces on the proximal humerus, displacement of these fractures is common. Most notably for the GT, the rotator cuff, namely, the supraspinatus and infraspinatus, act as the primary deformers. These muscles will typically pull the fragment superior and posterior. It is believed that a forceful contraction of the rotator cuff against a distracted humeral head from the glenoid is what leads to these avulsion type fractures [10].
As these GT fractures occur, their degree of displacement can lead to impingement. Most authors cite that 5 mm of displacement is enough to provide unsatisfactory results if left alone. For example, superior displacement can lead to impingement of the subacromial space [4]. The treatment of these injuries is sought to achieve anatomical reduction, prevent impingement, and restore rotator cuff function [9]. Incarcerated GT fragments in the glenohumeral joint can be detrimental to the cartilage and lead to early onset arthritis if not treated in a timely manner.
Many treatment options exist for GT fractures. Depending on the injury pattern and degree of displacement, arthroscopic versus open techniques can be utilized. Most commonly, heavy suture fixation, isolated screws, or a combination of plates and screws are utilized to secure the displaced fragment [4, 10].
In addition, factors such as degree of comminution, inadequate reduction, size of fragments, and lower bone quality can lead to bone loss at presentation and an increased risk of GT resorption after fixation [11]. To mitigate these risks, bone grafting may be used at times to aid in achieving appropriate reduction and allowing the bone the greatest potential to fully heal.
While standard open reduction internal fixation techniques using plates and screws are appropriate for treating these injuries, we chose to pursue a method that involved only bioabsorbable suture anchors. Using these anchors, we were able to achieve an anatomic reduction of the GT fragment that ultimately went on to achieve full healing. While many options exist for surgically treating these injury patterns, successful outcomes have been noted in 80–100% of cases when these fractures are treated operatively [10]. It is important to treat all displaced fractures with surgical intervention to allow these patients to optimize their chances of regaining full use of their shoulder.
Proximal humerus fractures are common injuries of the upper extremity. There are several described treatment techniques. This article is a case report of a patient with a displaced GT avulsion fracture treated with open reduction internal fixation utilizing multiple anchors and suture.
Isolated GT fractures can be detrimental to a patients function and range of motion. With the attachments of the rotator cuff, notably the supraspinatus and infraspinatus, at the GT, these fragments may become incarcerated in the glenohumeral joint. Operative treatment of these injuries is imperative to prevent accelerated osteoarthritis of the glenoid and humeral head and to restore optimal function of the joint.
References
- 1.Roux A, Decroocq L, El Batti S, Bonnevialle N, Moineau G, Trojani C, et al. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res 2012;98:715-9. [Google Scholar]
- 2.Passaretti D, Candela V, Sessa P, Gumina S. Epidemiology of proximal humeral fractures: A detailed survey of 711 patients in a metropolitan area. J Shoulder Elb Surg 2017;26:2117-24. [Google Scholar]
- 3.Iglesias-Rodríguez S, Domínguez-Prado DM, García-Reza A, Fernández-Fernández D, Pérez-Alfonso E, García-Piñeiro J, et al. Epidemiology of proximal humerus fractures. J Orthop Surg Res 2021;16:402. [Google Scholar]
- 4.Green A, Izzi J Jr. Isolated fractures of the greater tuberosity of the proximal humerus. J Shoulder Elbow Surg 2003;12:641-9. [Google Scholar]
- 5.Robinson CM, Shur N, Sharpe T, Ray A, Murray IR. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg Am 2012;94:18-26. [Google Scholar]
- 6.Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 1970;52:1077-89. [Google Scholar]
- 7.Kim SH, Ha KI. Arthroscopic treatment of symptomatic shoulders with minimally displaced greater tuberosity fracture. Arthroscopy 2000;16:695-700. [Google Scholar]
- 8.Park TS, Choi IY, Kim YH, Park MR, Shon JH, Kim SI. A new suggestion for the treatment of minimally displaced fractures of the greater tuberosity of the proximal humerus. Bull Hosp Joint Dis 1997;56:171-6. [Google Scholar]
- 9.Godin JA, Katthagen JC, Fritz EM, Pogorzelski J, Millett PJ. Arthroscopic treatment of greater tuberosity avulsion fractures. Arthroscopy Tech 2017;6:e777-83. [Google Scholar]
- 10.Rouleau DM, Mutch J, Laflamme GY. Surgical treatment of displaced greater tuberosity fractures of the humerus. J Am Acad Orthop Surg 2016;24:46-56. [Google Scholar]
- 11.Miyamura S, Lans J, Min KS, Waryasz GR, Murase T, Chen NC. Bone resorption of the greater tuberosity after open reduction and internal fixation of complex proximal humeral fractures: Fragment characteristics and intraoperative risk factors. J Shoulder Elbow Surg 2021;30:1626-35. [Google Scholar]





