Management of Osteosarcoma in a child less than 8 years is a challenge due to the resulting limb length discrepancy, hence an attempt can be made to preserve physeal growth by this novel technique.
Dr. Satvik N Pai, Department of Orthopaedic Surgery, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. E-mail: satvik.pai@gmail.com
Introduction: Osteosarcoma is a malignant tumor, the treatment of which is controversial between amputation and limb salvage surgery. Osteosarcoma occurring in a child is a challenge to manage due to the arrest of limb and the resultant limb length discrepancy. The management options for a child less than eight years of age are very limited.
Case report: We present a case of a six year old child who was diagnosed to have osteosarcoma of proximal tibia. She was started on neoadjuvant chemotherapy, after which, she underwent wide resection and reconstruction with free vascularised fibular graft. The joint was fused using a locking compression plate and screws. The locking screws were inserted avoiding the distal femoral physis, enabling growth of the physis in future. Adjuvant chemotherapy was then given. Follow up radiographs showed Harris growth lines indicating growth to be occurring at the distal femoral physis. She was not found to have recurrence on last follow up four years after surgery.
Conclusion:We found reconstruction using free fibular graft and arthrodesis using plate and screws, provided satisfactory results. An attempt can be made to preserve the distal femur physis.
Keywords:Osteosarcoma, proximal tibia, limb salvage surgery, vascularised fibula graft.
Osteosarcoma is the most common malignancy of bone in the paediatric population. It is derived from primitive osteoid forming mesenchymal cells [1] Amputation was previously considered the standard surgical procedure for osteosarcoma [2]. Advances in imaging and development of effective chemotherapy have led to limb salvage surgery being increasingly practised [3]. Osteosarcoma occurring in a child is a challenge to manage due to the arrest of limb and the resultant limb length discrepancy. The management options for a child less than eight years of age are very limited. We present a case of proximal tibia osteosarcoma in a six year old female child, managed with chemotherapy and limb salvage surgery with reconstruction done using a free vascularised fibula graft.
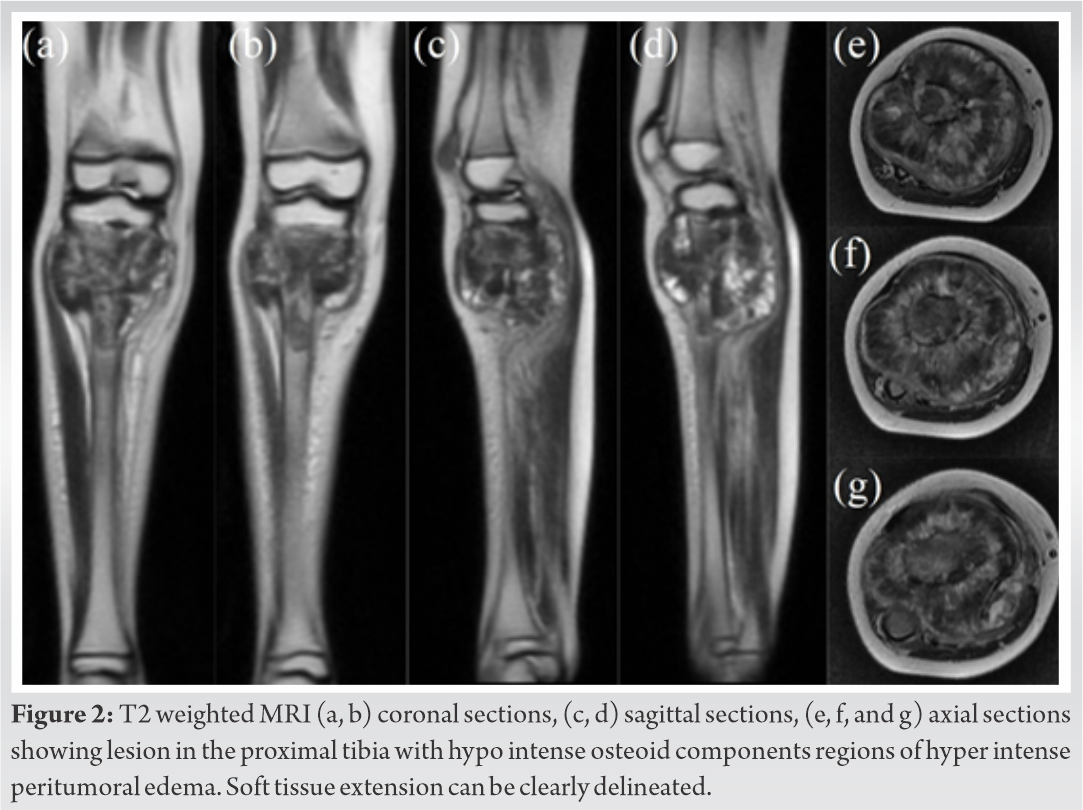
A six year old female child was brought to us with complaints of pain in her right leg since 15 days. She also had a swelling over the proximal part of her leg, which had increased in size rapidly since they first noticed it 15 days earlier. On examination, we found a bony hard, tender swelling extending over the anterior, medial and lateral aspect of the proximal leg. Range of movement of the knee joint was restricted with flexion up to 80 degrees, which was associated with pain. Radiographs (Fig. 1) showed an osteoblastic lesion over the metaphyseal region of proximal tibia. Sun burst pattern of matrix mineralisation was pronounced. A wide zone of transition was present. Codman’s triangle type of periosteal reaction was also visible. Magnetic Resonance Imaging (MRI) (Fig. 2) showed an expansile mass lesion in the metaphyseal region of proximal tibia. Positron Emission Tomography (PET) scan showed no evidence of increased uptake elsewhere in the body. Blood investigations showed alkaline phosphatase to be elevated. A core needle biopsy of the lesion was performed under fluoroscopic guidance, in line with the planned surgical approach for wide excision- medial approach. 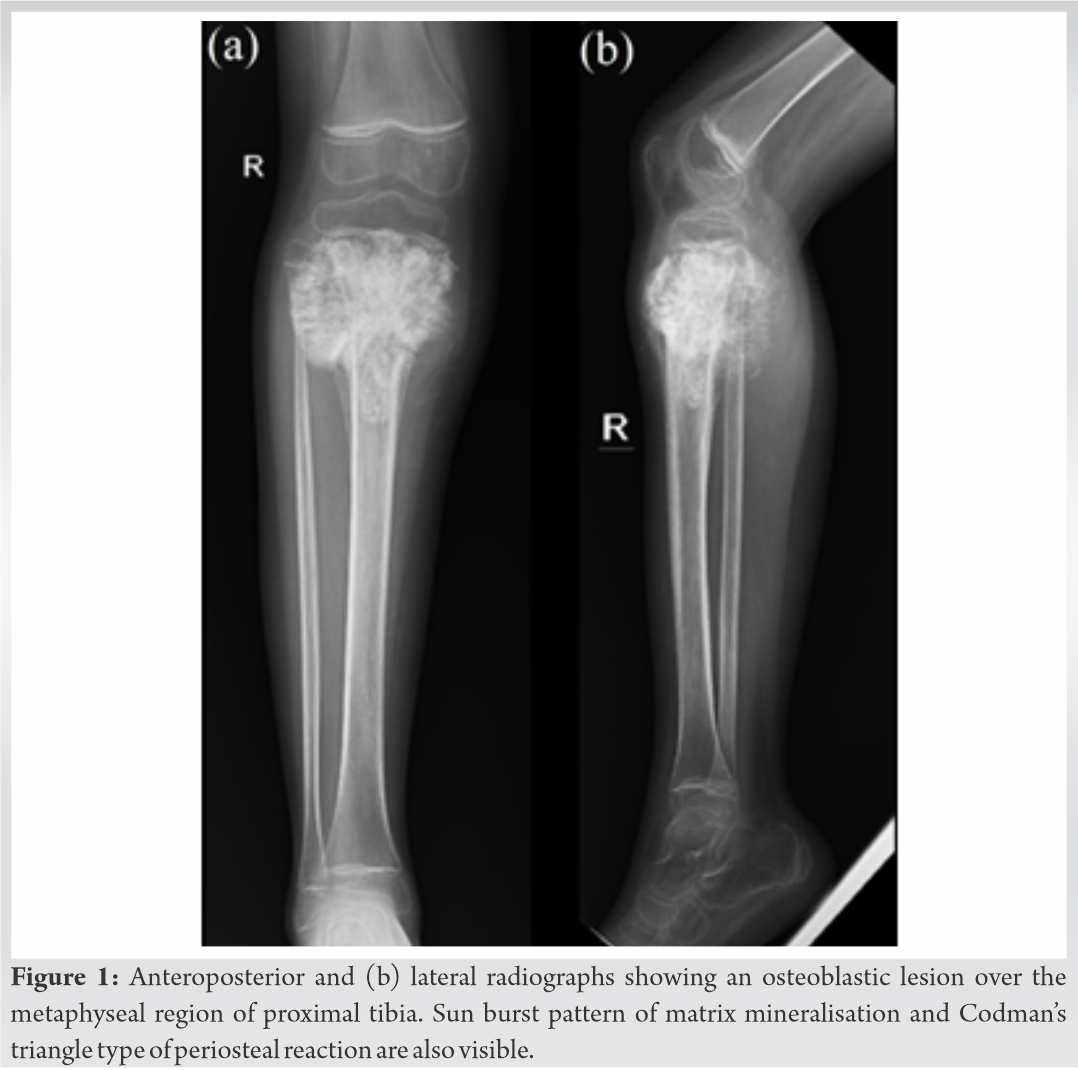
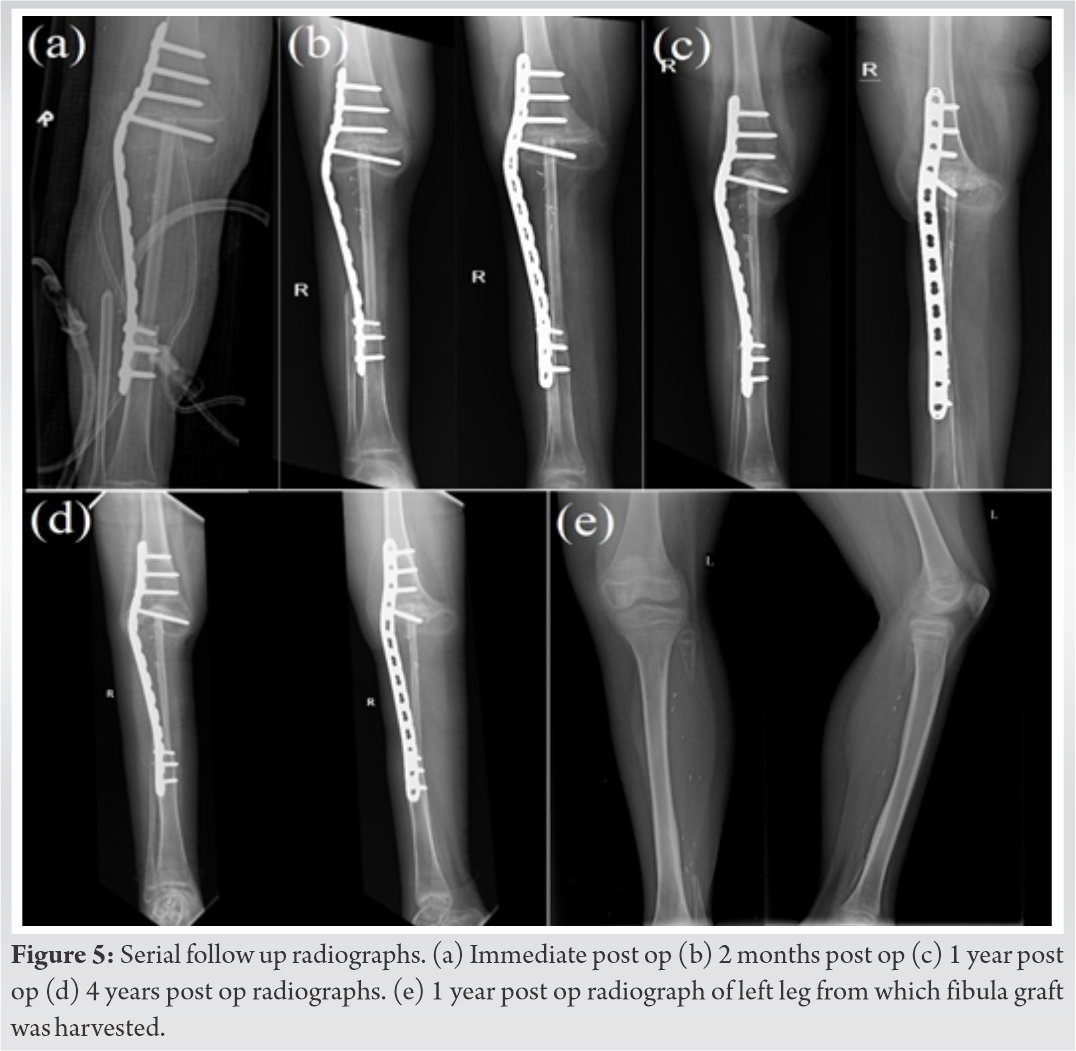
She was started on chemotherapy as per European and American Osteosarcoma Study (EURAMOS) protocol. Pre-operative chemotherapy consisted of five week cycles of methotrexate, doxorubicin (adriamycin) and cisplatin. Two such cycles was given for 10 weeks. Two weeks after which, she underwent wide resection of right proximal tibia and reconstruction with free vascularised fibular graft. Fibula was harvested from the contralateral side, peroneal artery of the fibula graft was anastomosed to right anterior tibial artery. The joint was fused using a 16 hole locking compression plate and screws. The locking screws were inserted avoiding the distal femoral physis (Fig. 4), enabling growth of the physis in future. The resected specimen on histopathological examination showed classical features of grade three conventional osteosarcoma, 15% tumor necrosis and margins to be free of malignancy.
Nine cycles of adjuvant chemotherapy were then given over 40 weeks. She was not permitted to bear weight over her right lower limb until two months after surgery, following which partial weight bearing was permitted for one month, and full weight bearing mobilisation was started three months after the surgery. Serial radiographs were taken on follow up (Fig. 5). Harris growth lines were visible in follow up radiographs indicating growth to be occurring at the distal femoral physis. She was not found to have recurrence on last follow up four years after surgery. She was able to walk unaided and was rehabilitated to her normal routine and activities, with Musculoskeletal Tumor Society Score (MSTS) of 19. Once fusion of the fibula graft on both sides has occurred completely, plate removal has been planned. The growth of the distal femur physis needs to be followed up.
Osteosarcoma around the knee joint was traditionally treated with amputation. In the last two decades, limb salvage therapy consisting neo-adjuvant chemotherapy, Limb salvage surgery (LSS) and adjuvant chemotherapy has gained favour [4]. LSS involves resection of the tumor and reconstruction procedure. The four main reconstructive procedures used currently are endoprosthesis, autograft, bulk allograft, and allograft prosthetic composite [5]. Each procedure has its own unique advantages and drawbacks. Use of an endoprosthesis is the most commonly used method of reconstruction, however is associated with a revision rate of 40% [6]. Allograft use has the risk of rejection reaction, allograft bone fracture, infection, and non‐union, with 54% of patients will requiring revision surgery [7]. Use of fibula autograft is especially useful for lower limb long bone defects, even when the defect is in excess of 15cm.Free vascularised fibular bone grafts (FVFGs) have shown success rates of 93.5% [8]. Due to the fact that they have their own blood supply, FVFGs are effective even in cases where there is poor vascularity at the recipient site. While FVFGs are versatile grafts used in a multitude of locations, there is scare literature available in their use for arthrodesis. Early complications of FVFGs is bleeding at the site of a technically poorly performed micro vascular anastomosis. Late complications include non-union, graft fracture and donor site morbidity. The other aspect of limb salvage therapy that is vital is the chemotherapy. Neoadjuvant chemotherapy has proven to significantly improve survival and success of LSS [9]. We employed chemotherapy as per the EURAMOS protocol [10], which has proven to be superior to other regimens and safe for use. In our case, following wide excision of the tumor, there would be a bone defect of about 12cm (cranio-caudal size of tumor was 9cm) and the knee joint would be lost whether the resection is intra-articular or extra-articular. The age of the child and residual growth of the child poses a unique challenge. Xu et al [11] note that custom mega prosthesis for child of this age is not advocated in view of high failure rates (especially in proximal tibia tumours) and potential growth for growth of the other limb leading to severe limb length discrepancy. Extendable tumor prosthesis while an interesting option, cannot match the residual growth of the contralateral limb in children less than 8 years of age. Arthrodesis of the knee joint has poor fusion rates in children as the epiphysis is cartilaginous and physeal growth would be arrested. Hence, limb salvage and reconstruction in a child less than 8 years of age is extremely challenging. Hence, amputation is usually favoured up to the age of eight years. However, the parents of the child were not willing for an amputation. This left led us to attempt a modification of knee arthrodesis using a vascularised fibula graft but preserving the distal femur physis.
Osteosarcoma can be treated with chemotherapy and limb salvage surgery. A viable option for the management of proximal tibia osteosarcoma is reconstructing the resected segment using free fibular graft and arthrodesis using plate and screws. An attempt can be made to preserve the distal femur physis by a modification of technique described in the case report.
Reconstructing the resected segment using free fibular graft and arthrodesis using plate and screws is viable option for the management of proximal tibia osteosarcoma, especially in children. An attempt can be made to preserve the distal femur physis by avoiding screws in the physis. This would enable further growth of physis in the future, thereby decreasing the limb length discrepancy. Multidisciplinary approach.
References
- 1.Prater S, McKeon B. Osteosarcoma. [Updated 2021 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549868/ [Google Scholar]
- 2.Anderson ME. Update on Survival in Osteosarcoma. Orthop Clin North Am. 2016;47(1):283-292. doi:10.1016/j.ocl.2015.08.022 [Google Scholar]
- 3.Gil S, Fernandez-Pineda I, Rao B, et al. Role of Amputation in Improving Mobility, Pain Outcomes, and Emotional and Psychological Well-Being in Children With Metastatic Osteosarcoma. Am J Hosp Palliat Care. 2019;36(2):105-110. doi:10.1177/1049909118791119 [Google Scholar]
- 4.Brookes MJ, Chan CD, Baljer B, et al. Surgical Advances in Osteosarcoma. Cancers (Basel). 2021;13(3):388. Published 2021 Jan 21. doi:10.3390/cancers13030388 [Google Scholar]
- 5.Perez JR, Jose J, Mohile NV, et al. Limb salvage reconstruction: Radiologic features of common reconstructive techniques and their complications. J Orthop. 2020;21:183-191. Published 2020 Mar 27. doi:10.1016/j.jor.2020.03.043 [Google Scholar]
- 6.Jeys LM, Kulkarni A, Grimer RJ, Carter SR, Tillman RM, Abudu A. Endoprosthetic reconstruction for the treatment of musculoskeletal tumors of the appendicular skeleton and pelvis. J Bone Joint Surg Am. 2008;90(6):1265-1271. doi:10.2106/JBJS.F.01324 [Google Scholar]
- 7.Fox EJ, Hau MA, Gebhardt MC, Hornicek FJ, Tomford WW, Mankin HJ. Long-term followup of proximal femoral allografts. Clin Orthop Relat Res. 2002;(397):106-113. doi:10.1097/00003086-200204000-00015 [Google Scholar]
- 8.Xu M, Wang Z, Yu XC, Lin JH, Hu YC. Guideline for Limb-Salvage Treatment of Osteosarcoma. Orthop Surg. 2020;12(4):1021-1029. doi:10.1111/os.12702 [Google Scholar]
- 9.Zhang SP, Li X, Li H, Sun XH, Yan XF. Significance of neoadjuvant chemotherapy (NACT) in limb salvage treatment of osteosarcoma and its effect on GLS1 expression. Eur Rev Med Pharmacol Sci. 2018;22(19):6538-6544. doi:10.26355/eurrev_201810_16068 [Google Scholar]
- 10.Whelan JS, Bielack SS, Marina N, et al. EURAMOS-1, an international randomised study for osteosarcoma: results from pre-randomisation treatment. Ann Oncol. 2015;26(2):407-414. doi:10.1093/annonc/mdu526 [Google Scholar]
- 11.Xu M, Wang Z, Yu XC, Lin JH, Hu YC. Guideline for Limb-Salvage Treatment of Osteosarcoma. Orthop Surg. 2020;12(4):1021-1029. doi:10.1111/os.12702. [Google Scholar]