Anatomical reduction, adequate fixation, and judicious selection of implants are of utmost importance for successful outcomes of femoral neck fractures in children, even if the child presented late.
Dr. Janki Sharan Bhadani, Department of Orthopaedics, Indira Gandhi Institute of Medical Science, Patna - 800 014, Bihar, India. Email: jsbhadani@gmail.com
IntroductionFracture neck of femur in pediatric age group occurs due to high energy trauma and is an uncommon entity with high complication rate. No uniform guidelines are present to manage these fractures, especially in delayed presentation of fracture neck of femur as a smaller number of such cases were reported.
Case ReportEight children (nine hips), five boys and three girls of age <15 years, were operated on. The mean delay in surgery time was 8.6 days (range: 5–22 days). The mean union time was 13.44 weeks. The mean follow-up was 20.88 months (range: 12–36 months). All the cases were managed with closed or open reduction followed by internal fixation with or without hip spica application and resulted in satisfactory outcomes in most of the cases.
ConclusionAnatomical reduction (open or closed) and fixation reduce the risk of complications even in delayed presentation if the orthopedic surgeon is familiar with the management.
KeywordsHigh energy trauma, neck of femur fracture, pediatric hip, delayed presentation.
The fracture of the neck of femur in the pediatric age accounts for <1% [1, 2, 3]. These fractures occur due to high-energy trauma such as RTAs, sports activities, fall from height, and are also at times associated with metabolic disorders [4, 5, 6, 7, 8]. This may present as a part of polytrauma or of multiple fractures with pelvic injury, acetabulum fracture, dislocated hip, or ipsilateral shaft fracture [9, 10, 11, 12]. These children are at a high risk of complications such as osteonecrosis of the femoral head, non-union, premature physeal fusion, and reduction of neck-shaft angle despite appropriate diagnosis and management [9, 13, 14, 15]. Due to the difference in vascular anatomy of the proximal femur in adults and pediatric age groups, sometimes complications are inevitable and result in unsatisfactory outcomes [6, 7, 15]. In the literature, multiple methods of fracture fixation, such as fixation with multiple cannulated cancellous screw (CCS), paediatric dynamic hip screw (DHS), have been suggested. Early stable fixation with anatomical reduction supplemented by hip spica immobilization in children is done to obtain good outcomes [9, 15, 16]. Fractures were classified using Delbet classification, which guides treatment and provides insight into prognosis [9, 16, 17]. Unintentional delay in surgery is not unusual in developing countries [18, 19]. There are no uniform guidelines to manage these fractures, especially in delayed presentation of fracture neck of femur due to relatively small number of reported cases. This research assesses surgical outcomes in pediatric neck of femur fracture when presented late.
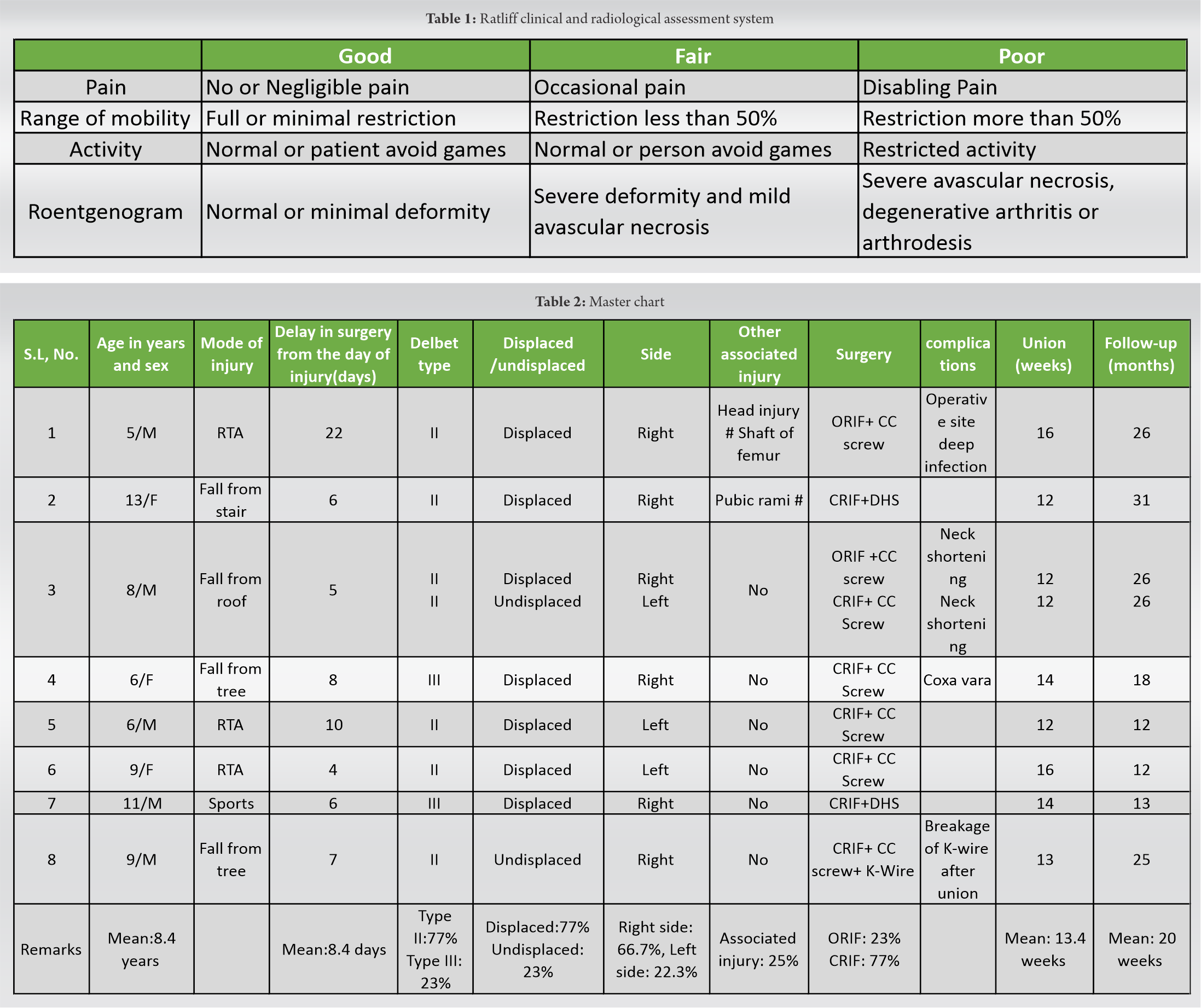
The aim of the study is to assess the outcome of the management of the femoral neck fractures in pediatric age operated after 24 h, the usual advocated period. Children with pathological fractures, metabolic diseases of bones, and neural disorders like cerebral palsy patients were excluded from the study. After prior informed and written consent for taking part in the study from guardians of children, we analyze all patients (age <15 years) with the neck of femur fracture operated from January 2016 to December 2020. Eight children (total of nine hips), in which five boys and three girls who completed a minimum follow-up of at least 1 year, were incorporated in the study. Fractures were categorized using Delbet and Colonna classification system [13] and further fractionated into undisplaced and displaced. Both closed reduction or open reduction and internal fixation (CRIF/ORIF) were included in the study. Multiple CCS or DHS or combinations of implants, for example, CCS+DHS or CCS+ Kirschner wire (K-wire) were used depending on the fracture pattern. Postoperative immobilization was done with or without the application of spica cast (for 6 weeks) depending on the age of patients, pattern of fracture, quality of fixation, and compliance. We have used Ratliff’s method to assess the outcome of the study [Table 1] [20].
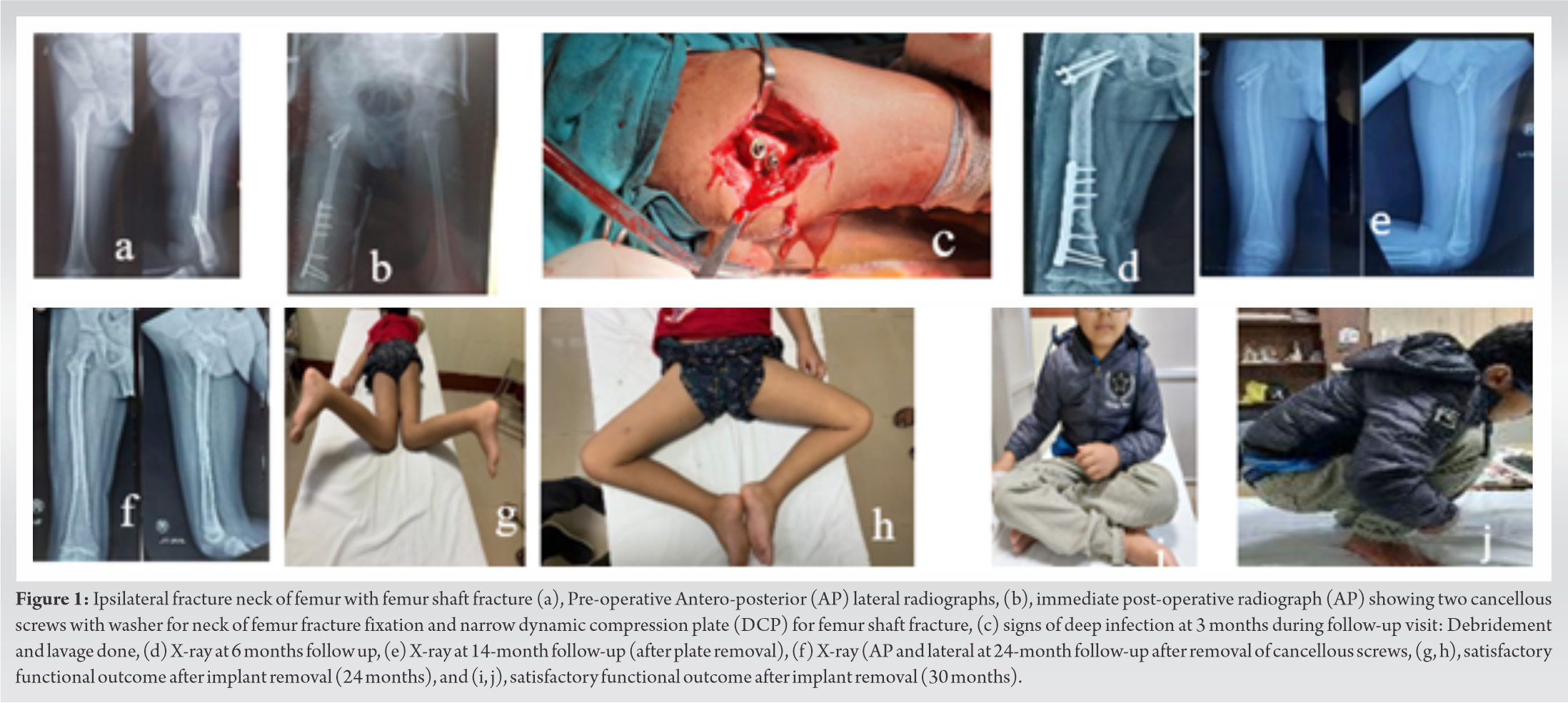
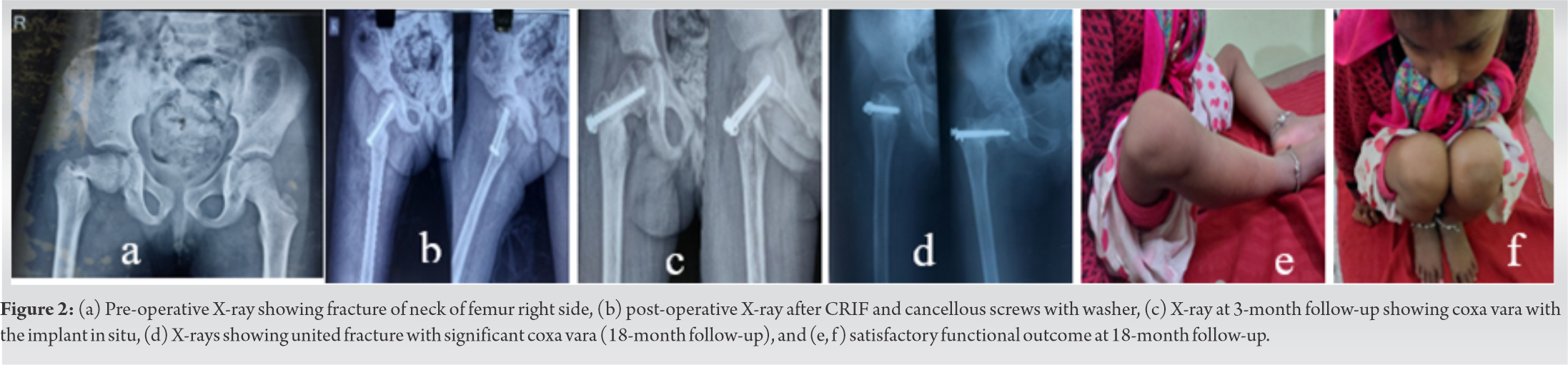
In our study, there were a total of eight patients (nine hips) of mean age of 8.4 years (range 5–13 years), five were male and three were female. The most common modes of injury were falls from height (50%), road traffic accidents (RTA) (37.5%), and accidents due to sporting activities (12.5%). The most commonly observed fracture was Type II Delbet (transcervical type; five were managed by CRIF and two by ORIF) and two were Type III Delbet (Cervicotrochanteric; both were managed by CRIF). No case of Delbet’s Type I and IV was found. Seven fractures were displaced and two undisplaced. Fixations were done in all fractures after reduction – either closed or open. Six fractures were fixed with CCS of which open reduction was done in two cases, [Fig. 1, 2] in two fractures closed reduction and internal fixation were done with DHS + one CC Screw [Fig. 3] and one fracture was fixed with CCS + K-wire. The preference of implants depends on the child age, fracture type, and surgeon familiarity with implants. In older children and Delbet Type III/IV, fracture DHS was preferred, where as in younger children, partially threaded cancellous screw (either 6.5 mm or 4.5 mm) was used. The average delay in surgery time was 8.6 days (range: 5–22 days). One child was also associated with head injury and ipsilateral shaft of femur fracture. In that case, surgery was delayed due to poor health condition, one child had a fracture of ipsilateral pubic rami, and one child had bilateral fracture of neck femur. The average union time was 13.44 weeks. The average follow-up was 20.88 months (range: 12–36 months). One patient presented with sinus with frank pus discharge through the operated site 2 months after the primary surgery, which was managed successfully with debridement, lavage, and local antibiotic instillation (vancomycin powder), keeping the implant in situ, and continued intravenous antibiotic for 6 weeks postoperatively based on culture and sensitivity. There were coxa vara in one case, neck shortening in two cases, and implant breakage in one case [Table 2].
Expertise to treat the fracture neck of femur in children is difficult for most orthopedic surgeons because it is rare, so we get less opportunity to treat these. Cases of these fractures have been growing in the recent past due to the rise in RTAs. In this study, 37.5% of fractures were due to RTAs which is comparable to studies done by Bali et al. (53%), and 50% were due to falls from height either from trees or stairs [12]. The mean age of children in our study has been 8.4 years (range 5–13 years). Age consideration is important not only for the selection of suitable implants for the fixation after reduction but also as a predictor of prognosis. Age ≥10 years is the solitary statistically notable independent predictor of avascular necrosis (AVN) (P = 0.04) of head of femur according to Pavone et al. (44 cases). In another study by Riley et al. (255 cases), there were no cases of AVN found in children <11 years old. Although overall 20% of cases developed AVN in both the studies [16, 21]. In our study, two out of ten children were more than 10 years old and none of them developed AVN. However, in developing countries, delay in definitive care is not so uncommon due to unavoidable circumstances such as delay in presentation due to poverty, illiteracy, quack treatment, late referral to specialized hospitals from remote areas, and lack of resources [16, 22]. Patient load, lack of expertise, or escalation of an ongoing pandemic may also contribute to delay in definitive care. In our study, we have found that late referral to hospitals by local clinics is the most common cause of delay in treatment. In this study, 78% of cases were Delbet Type II, succeeded by 22% Delbet Type III, which is similar to the available literature (II>III>IV>I) [12, 20, 23, 24]. In this study, no cases of Delbet Type I and IV fractures were found. Anatomical reduction and stable fixation without delay are important factors to avoid complications that are usually associated with fractures [5, 6, 7, 8, 9, 17, 18, 23]. We have done open reduction in two of nine hips as the anatomical reduction was not possible by closed means in these two cases. In spite of the common belief that injury of vascular supply by ORIF may increase the risk of AVN, none of them developed AVN in our study, which supports the fact described by Song et al., who reported a low incidence of AVN in patients in which ORIF was done [25]. It might be because of the release of tamponade effect by capsulotomy in the ORIF group which reduces intracapsular pressure [26]. As the major blood supply of the head of femur is through lateral epiphyseal artery that traverses along the posterior part of femoral neck and not anteriorly, hence, capsulotomy anteriorly does not hamper those [12]. Age, delay in surgery, fracture type, reduction of fracture either open or closed, and method of fixation all have bearing on functional outcome [23, 27, 28, 29]. We have found 78% of satisfactory outcome according to the modified Ratliff criteria in our study which is comparable with Bombaci et al. [24] (24 h delay, 22 patients, 73 months mean follow-up, fair to good outcomes in 20 (91.0%), and with poor outcomes in two (9.1%)) using modified Ratliff criteria, and Toguri et al. [30] (96 months of mean follow-up in 61 out of 102 children). We found one or more complications in five of the nine fractures, (55.5%) which at times affect the outcome. Dendane et al. reported 33% complications in their study [6]. There was bilateral neck shortening in one case due to premature physeal closure. One child developed limping due to coxa vara deformity, probably because we have not achieved satisfactory reduction of the fracture. Revision surgery was done in one case of infection, which was managed with prompt debridement and instillation of local antibiotics. There were no complications such as non-union, overgrowth of the femoral neck, or post-traumatic slipped capital femoral epiphysis. There was no case of AVN noticed in any of the children in our study even if there was delay in treatment, which supports the fact that development of AVN can occur independently and not depend on the fracture fragment displacement [16]. There is a risk of osteonecrosis in 17% to 47% of the cases, because blood vessels of pediatric hip are critical as they do not cross the growth plate and also get injured easily in hip fractures [12, 13, 16, 18, 21, 25]. Coxa vara is defined as a decrease in femoral neck-shaft angle of 120° or less. One child (11%) managed by CRIF with CCS developed coxa vara which is comparable to 18% found in Lark et al. study [13]. One case developed coxa vara after CRIF. ORIF helps to achieve near anatomical reduction and lessen chances of non-union and reduced neck-shaft angle and neck shortening in addition to avoiding AVN [31]. There was no development of non-union in any of the cases in our study. Non-union has been reported in 10% of these fractures in children and is commonest in Delbet Type II [12, 14]. Implant (K-wire) breakage detected after 12 months in one patient but asymptomatic, non-compliant, and did not undergo further surgery for implant removal as advised. This was late loss of reduction in one case resulting in coxa vara managed by in situ application of hip spica for 4 weeks. Deep infection occurred in one case (11%), managed by debridement, lavage, and local antibiotic instillation, though reported incidence of infection is up to 1% in such fractures [9, 14, 17]. Our study has some limitations including the sample size – merely eight patients – and use of several types of implants.
We need to leave no stone unturned to reduce the risk of potentially devastating complications for neck of femur fractures in children. Anatomical reduction and adequate fixation are of utmost importance for successful outcomes even if patients presented late.
Management of late presenting pediatric neck of femur fracture is a challenging problem and there is no universal single acceptable method or approach for addressing such cases. Anatomical reduction and adequate stability with appropriate implants are key factors to achieve a successful outcome in these cases.
References
- 1.Papalia R, Torre G, Maffulli N, Denaro V. Hip fractures in children and adolescents. Br Med Bull 2019;129:117-28. [Google Scholar]
- 2.Boardman MJ, Herman MJ, Buck B, Pizzutillo PD. Hip fractures in children. J Am Acad Orthop Surg 2009;17:162-73. [Google Scholar]
- 3.Mazurek T, Lorczyński A, Ceynowa M. Bilateral femoral neck fracture in a child: A 17-year follow-up. J Pediatr Orthop B 2011;20:295-8. [Google Scholar]
- 4.Dhar D. Bilateral traumatic fracture of neck of femur in a child: A case report. Malays Orthop J 2013;7:34-6. [Google Scholar]
- 5.Palocaren T. Femoral neck fractures in children: A review. Indian J Orthop 2018;52:501-6. [Google Scholar]
- 6.Dendane MA, Amrani A, El Alami ZF, El Medhi T, Gourinda H. Displaced femoral neck fractures in children: Are complications predictable? Orthop Traumatol Surg Res 2010;96:161-5. [Google Scholar]
- 7.Matejka J, Pavelka T, Kostál J, Cervenková H. Long-term results following fracture of the femoral neck in children. Acta Chir Orthop Traumatol Cech 2005;72:98-104. [Google Scholar]
- 8.Rocha DF, Horwitz DS, Sintenie JB. Femoral neck fractures in children: Issues, Challenges, and Solutions. J Orthop Trauma 2019;33:S27-32. [Google Scholar]
- 9.Patterson JT, Tangtiphaiboontana J, Pandya NK. Management of pediatric femoral neck fracture. J Am Acad Orthop Surg 2018;26:411-9. [Google Scholar]
- 10.Flynn JM, Wong KL, Yeh GL, Meyer JS, Davidson RS. Displaced fractures of the hip in children. Management by early operation and immobilisation in a hip spica cast. J Bone Joint Surg Br 2002;84:108-12. [Google Scholar]
- 11.Hajdu S, Oberleitner G, Schwendenwein E, Ringl H, Vécsei V. Fractures of the head and neck of the femur in children: An outcome study. Int Orthop 2011;35:883-8. [Google Scholar]
- 12.Bali K, Sudesh P, Patel S, Kumar V, Saini U, Dhillon MS. Pediatric femoral neck fractures: Our 10 years of experience. Clin Orthop Surg 2011;3:302-8. [Google Scholar]
- 13.Lark RK, Dial BL, Alman BA. Complications after pediatric hip fractures: Evaluation and management. J Am Acad Orthop Surg 2020;28:10-9. [Google Scholar]
- 14.Dial BL, Lark RK. Pediatric proximal femur fractures. J Orthop 2018;15:529-35. [Google Scholar]
- 15.Dai ZZ, Zhang ZQ, Ding J, Wu ZK, Yang X, Zhang ZM, et al. Analysis of risk factors for complications after femoral neck fracture in pediatric patients. J Orthop Surg Res 2020;15:58. [Google Scholar]
- 16.Pavone V, Testa G, Riccioli M, Di Stefano A, Condorelli G, Sessa G. Surgical treatment with cannulated screws for pediatric femoral neck fractures: A case series. Injury 2019;50:S40-4. [Google Scholar]
- 17.Pinto DA, Aroojis A. Fractures of the proximal femur in childhood: A review. Indian J Orthop 2020;55:23-34. [Google Scholar]
- 18.Varshney MK, Kumar A, Khan SA, Rastogi S. Functional and radiological outcome after delayed fixation of femoral neck fractures in pediatric patients. J Orthop Traumatol 2009;10:211-6. [Google Scholar]
- 19.Kumar I, Ahmed W, Roshan R, Kumar S, Bhadani JS. Traumatic bilateral neck of femur fracture in paediatric age: A case report and review of literature. Med J Armed Forces India 2022 (in press) [Google Scholar]
- 20.Ratliff AH. Fractures of the neck of the femur in children. J Bone Joint Surg Br 1962;44:528-42. [Google Scholar]
- 21.Riley PM, Morscher MA, Gothard MD, Riley PM. Earlier time to reduction did not reduce rates of femoral head osteonecrosis in pediatric hip fractures. J Orthop Trauma 2015;29:231-8. [Google Scholar]
- 22.Azam MQ, Iraqi A, Sherwani M, Abbas M, Alam A, Sabir AB, et al. Delayed fixation of displaced Type II and III pediatric femoral neck fractures. Indian J Orthop 2009;43:253-8. [Google Scholar]
- 23.Canale ST, Bourland WL. Fracture of the neck and intertrochanteric region of the femur in children. J Bone Joint Surg Am 1977;59:431-43. [Google Scholar]
- 24.Bombaci H, Centel T, Babay A, Türkmen IM. Evaluation of complications of femoral neck fractures in children operated on at least 24 hours after initial trauma. Acta Orthop Traumatol Turc 2006;40:6-14. [Google Scholar]
- 25.Song KS. Displaced fracture of the femoral neck in children: Open versus closed reduction. J Bone Joint Surg Br 2010;92:1148-51. [Google Scholar]
- 26.Pauyo T, Drager J, Albers A, Harvey EJ. Management of femoral neck fractures in the young patient: A critical analysis review. World J Orthop 2014;5:204-17. [Google Scholar]
- 27.Heiser JM, Oppenheim WL. Fractures of the hip in children: A review of forty cases. Clin Orthop Relat Res 1980;149:177-84. [Google Scholar]
- 28.Lam SF. Fractures of the neck of the femur in children. J Bone Joint Surg Am 1971;53:1165-79. [Google Scholar]
- 29.Moon ES, Mehlman CT. Risk factors for avascular necrosis after femoral neck fractures in children: 25 Cincinnati cases and meta-analysis of 360 cases. J Orthop Trauma 2006;20:323-9. [Google Scholar]
- 30.Togrul E, Bayram H, Gulsen M, Kalaci A, Ozbarlas S. Fractures of the femoral neck in children: Long-term follow-up in 62 hip fractures. Injury 2005;36:123-30. [Google Scholar]
- 31.Chen Y, Zhang X, Guo H, Liu N, Ren J, Lu C. Poor outcomes of children and adolescents with femoral neck fractures: A meta-analysis based on clinical studies. Orthop Surg 2020;12:639-44. [Google Scholar]