Platelet-rich plasma injection is a safe and efficacious treatment modality in recurrent cases of flexor tenosynovitis of the wrist, especially when associated with uncontrolled type 2 diabetes mellitus.
Dr. Debasish Jena, Department of Physical Medicine and Rehabilitation, All India Institute of Medical Sciences, Bhubaneswar - 751019, Odisha, India. E-mail: debasish.mbbs@gmail.com
IntroductionHand disorders are common manifestations in persons with diabetes mellitus. Flexor tenosynovitis (FTS) of the wrist is a relatively less common occurrence when compared with FTS of the finger. In the presence of uncontrolled diabetes, recurrence is not uncommon, and management may become difficult. There is no mention in the literature about the management of FTS in the wrist, especially in recurrent cases.
Case PresentationA 38-year-old lady presented with pain and swelling over the volar aspect of the wrist associated with weakness of the grasp. In addition, she reported tingling and a current-like sensation in the radial three and a half digits. Routine laboratory investigations and plain radiographs of the wrist and hand revealed no abnormalities. An ultrasound (USG) scan of the carpal tunnel showed thickening of the flexor tendons, surrounding hypo- to anechoic areas with enhanced color Doppler signal. In addition, there was associated thickening of the median nerve compared to the healthy side. She reported recurrence of the symptoms despite several trials of conservative management and one injection of local corticosteroid. We planned a single injection of platelet-rich plasma (PRP) under direct USG visualization in an in-plane and short-axis view. There was a significant improvement in both pain and function scores up to a 3-month follow-up.
ConclusionFTS of the wrist is a less commonly reported entity that can be missed with clinical examination only. A USG scan can help in the detection of this condition whenever the diagnosis is uncertain. In patients with uncontrolled diabetes, PRP injection appears to be a safe and appropriate treatment option that can improve pain and function scores in the moderate term.
KeywordsTenosynovitis, carpal tunnel syndrome, platelet-rich plasma, diabetes mellitus, rehabilitation, pain medicine, ultrasonography, pain management.
Diabetes mellitus (DM) predisposes to a wide array of musculoskeletal manifestations with longer duration of diabetes and inadequate sugar control being the two major risk factors. Hand complications are very common in DM, including but not limited to, carpal tunnel syndrome (CTS), de Quervain’s tenosynovitis, limited joint mobility, flexor tenosynovitis (FTS), and Dupuytren’s contracture [1]. FTS or stenosing tenosynovitis of finger (commonly known as trigger finger) is an established complication of diabetes but FTS of wrist is a less commonly reported complication. Furthermore, FTS of the wrist can cause increased tension in the carpal tunnel and compression of the median nerve resulting in CTS.
Platelet-rich plasma (PRP) injection is a relatively recent and efficacious treatment modality for a variety of musculoskeletal conditions because of its safety and regenerative properties [2]. In the past, PRP has been tried with encouraging results in the management of CTS and de Quervain’s tenosynovitis, with ongoing trial on FTS of finger but its effect on FTS of wrist remains unknown [3, 4, 5]! Therefore, we intend to report a case of uncontrolled type 2 DM associated with recurrent FTS of wrist and CTS who was managed with a single injection of PRP.
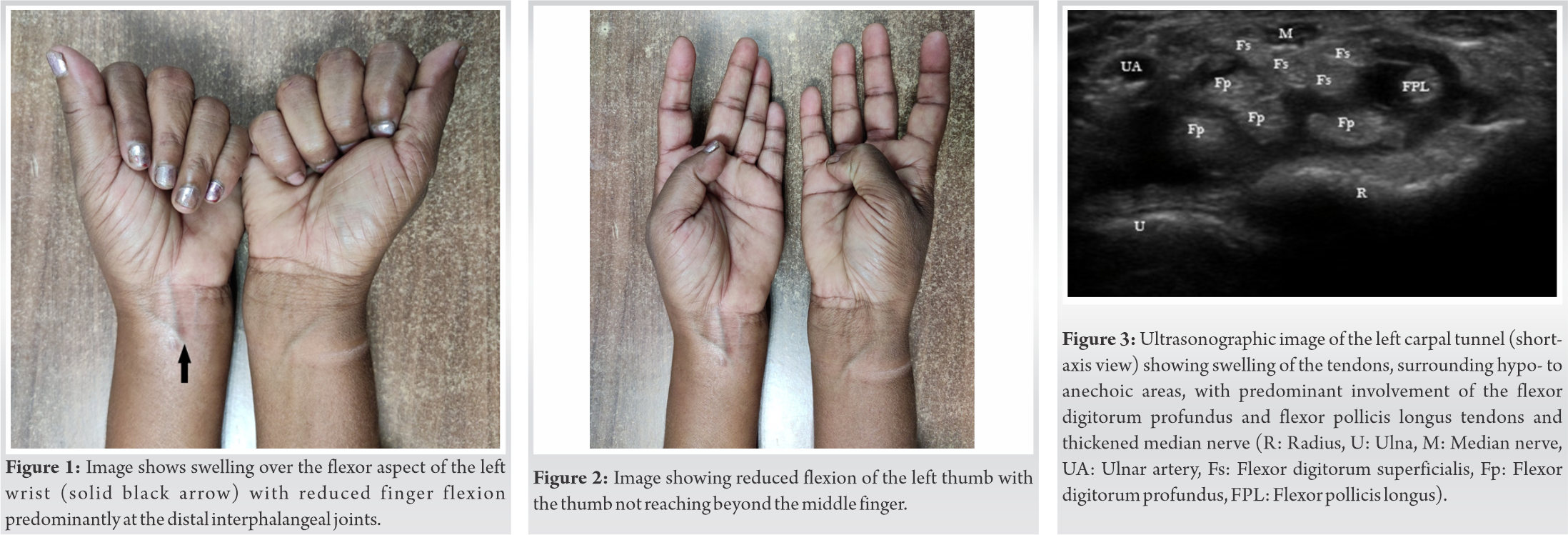
A 38-year-old lady presented to the outpatient facility of the department of physical medicine and rehabilitation of our hospital with the chief complaints of pain and associated swelling over the volar aspect of the left wrist. The swelling appeared 12 months back, gradually progressing in size associated with increasing pain intensity. Since the past 2 months, the pain started radiating to the hand involving the thumb, index, and middle finger. In addition, she developed stiffness of wrist and hand with reduced grip strength leading to difficulty in carrying out activities of daily living (ADLs). She had been diagnosed with DM since the past 3 years and was on oral hypoglycemic drugs. There was no history of thyroid disorder, rheumatoid arthritis, gout, tuberculosis, use of immunosuppressants, or any local trauma. On inspection, there was a clear swelling over the volar aspect of the left wrist. The overlying skin was shiny and edematous. There was no apparent wasting of the thenar eminence or any other associated features (Fig. 1). On palpation, the local temperature was normal and a Grade 2 tenderness over the swelling could be elicited. On functional evaluation, the grip strength was reduced compared to the healthy side with gross reduction in the fine functions of hand (Fig. 2). On further examination, the Phalen’s test, Tinel sign, and carpal tunnel compression test were positive. We made a provisional diagnosis of FTS of wrist resulting in CTS.
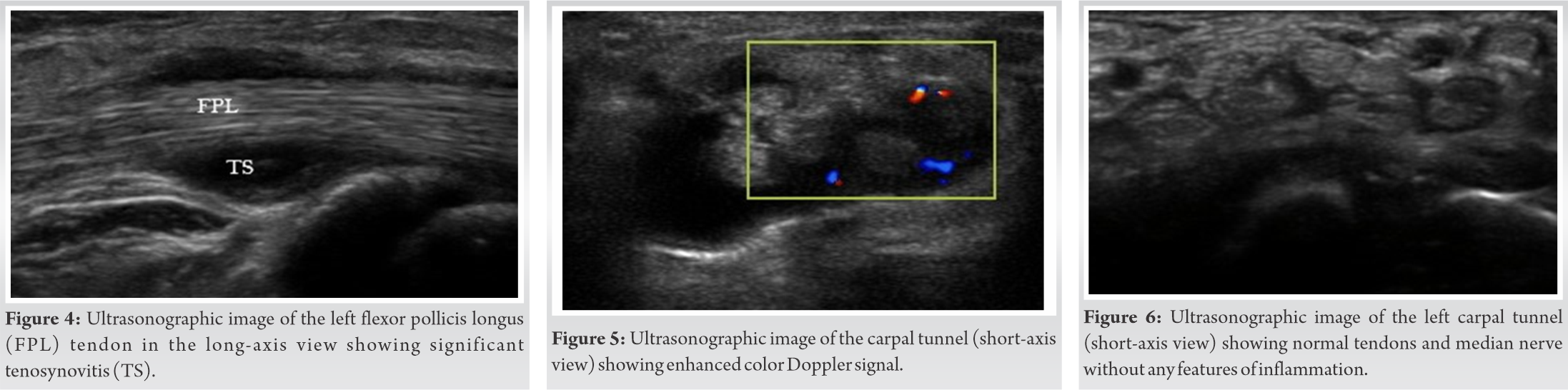
Laboratory investigations revealed uncontrolled DM with hemoglobin A1c level of 10.7% and a slightly raised ESR. A plain radiograph of the wrist including anteroposterior and lateral view was unremarkable. We further proceeded with an ultrasound (USG) scan of the wrist to confirm our diagnosis. USG scan was performed with a linear multi-frequency probe (13–8 MHz; Sonosite Inc.) in two perpendicular planes at the level of carpal tunnel. Compared to normal side, the affected side showed gross synovial thickening in the carpal tunnel, swelling of the flexor tendons with increased echogenicity, and color Doppler signal. In addition, the median nerve was thickened with a cross-sectional area of 15 mm2 (Fig. 3-5). A nerve conduction study of both upper limbs confirmed the compression of the median nerve at the level of wrist.
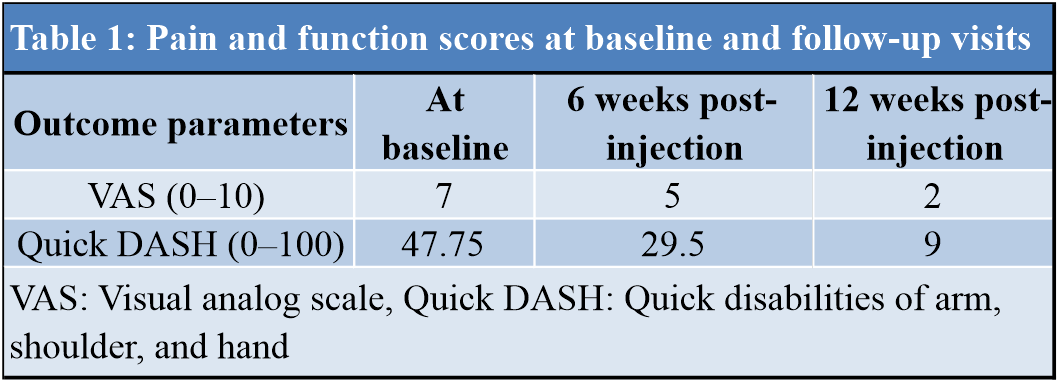
She has undergone treatment multiple times for this condition but the symptoms reappeared each time on stopping the medications. She has also been injected with local corticosteroids elsewhere with resolution of the symptoms for a period of 1 month only. At our institute, initially, she was advised with a short course of NSAIDs, local ice application, bracing for CTS, and activity modifications. Furthermore, she was counseled regarding the importance of strict glycemic control with diet modification, regular aerobic exercises, and oral hypoglycemic medications. As a next step, we planned for USG-guided injection PRP as corticosteroids were not indicated this case because of the uncontrolled diabetes. Before injection, the severity of her clinical symptoms was assessed using the visual analog scale (VAS; 0 – no pain and 10 – worst pain) and shortened disabilities of the arm, shoulder, and hand (DASH) questionnaire (Quick DASH/Q-DASH; 0 – no disability and 100 – maximum disability). The average score of pain on VAS was 7 and the function score on Q-DASH was 48.5. In the laboratory of our hospital, PRP was prepared using the Eppendorf AG Centrifuge 5702 (Eppendorf Hamburg, Germany; Platelet Separation System). First, 30 ml of venous blood was collected from patient’s asymptomatic hand and centrifugation was done at two consecutive density gradients (total 3100 runs for duration of 10 min). During the first centrifugation, RBCs were isolated, and in the second centrifugation, PRP was separated from the platelet-poor plasma and transferred in to a sterile tube. Next under continuous USG guidance, 3 ml PRP was injected into the carpal tunnel and another 2 ml was infiltrated around the median nerve with an in-plane approach in the short-axis view. The whole procedure of preparing PRP and its injection was performed under sterile condition.
Post-injection, the patient was advised to rest the affected part for 1 week and ice the injection site, thrice daily, 15 min each session for a period of 3 days. Tablet paracetamol (650 mg) was prescribed for managing her pain up to a maximum of three tablets per day. Further, she was demonstrated with median nerve mobilization exercises and flexor tendon gliding exercises and advised to start the exercise regimen after the 1-week rest period. She was followed up at 6 weeks and 12 weeks of injection and the VAS and Q-DASH scores were assessed at each follow-up (Table 1). At 3 months, she had a significant improvement in symptoms and was able to carry out her ADLs with minimal restrictions. USG scan at the end of 3 months showed normal appearing tendons and median nerve with no signs of inflammation (Fig. 6).
FTS of hand and wrist can occur in isolation or in association with certain medical conditions including DM, rheumatoid arthritis, tuberculosis, and other mycobacterial infections, histoplasmosis, etc. [6, 7, 8]. In a report of unusual causes of CTS, six patients out of 23 patients were having non-specific tenosynovitis in the carpal tunnel [9]. Tenosynovitis of flexor tendons at the wrist may produce one or more of the following signs/symptoms: (1) Pain and/or swelling at the volar surface of wrist, (2) compression of the median nerve leading to symptoms of CTS, and (3) weakness of the hand grip. In patients with chronic and/or progressive tenosynovitis, the synovium may infiltrate and result in adhesions, thereby producing weakness of the grasp [6]. Initial conservative management should include NSAIDs, ice application, rest to the affected part, and a night-time splinting for CTS. Moreover, treatment of the underlying condition should be given prior importance. If conservative management fails, local corticosteroid injection is the preferred treatment, if not contraindicated. In patients having persistent disabling symptoms despite an adequate conservative management and trial of injections, are best managed with flexor tenosynovectomy. However, in this case due to the presence of uncontrolled diabetes, steroids are not indicated due to a potential risk of acute rise in blood sugar levels [10]. Therefore, PRP appears to be a safer alternative in this case because of its safety and encouraging results reported in several musculoskeletal conditions. PRP is blood component that contains plasma-derived fibrinogen and platelet-related growth factors above the normal levels. Because of its autologous origin, PRP has minimal risk of allergy, transmission of bloodborne microorganisms, incompatibility, and medical contraindications. Because of the presence of higher concentrations of cytokines and growth factors, PRP aids in the healing of the injured tissue through enhanced tissue remodeling [11]. The effect of PRP in the management of CTS and synovitis of the flexor tendon sheath of fingers has already been established. As much as the authors are conscious, this is the first report on the use of PRP injection in the treatment of FTS of the wrist. Furthermore, in uncontrolled diabetes where corticosteroids are contraindicated, PRP can be a safe as well as effective option in those resistant to usual conservative management. In this report, a single-injection PRP provided moderate term improvement in both pain and function. The major limitation of this study is the inclusion of only a single case which prevents generalization of our results. Furthermore, a longer follow-up could have provided better understanding of the outcome. Therefore, further well-designed study with larger sample size and longer follow-up is warranted to support our results.
FTS of wrist itself or in association with CTS can produce significant pain and disability due to impaired hand function. USG can be a quick and effective diagnostic tool showing extensive thickening of the tendon sheaths, tenosynovium, and hypervascularity as the major findings. In patients with uncontrolled diabetes, PRP is a safe intervention and can provide moderate-term improvement in pain and function. To support our findings, the authors recommend further well-designed studies with longer follow-up.
FTS of the wrist is a less common complication of DM that can present as pain and swelling of the volar wrist. It can further lead to features of CTS by compression of the median nerve in the carpal tunnel. In severe cases, there can be gross impairment of the hand function. In resistant cases with poor glycemic control, a single injection of PRP under USG guidance is safe and effective treatment modality that can significantly improve pain and function up to moderate term.
References
- 1.Kaka B, Maharaj SS, Fatoye F. Prevalence of musculoskeletal disorders in patients with diabetes mellitus: A systematic review and meta-analysis. J Back Musculoskelet Rehabil 2019;32:223-35. [Google Scholar]
- 2.Ahmad Z, Howard D, Brooks RA, Wardale J, Henson F, Getgood A, et al. The role of platelet rich plasma in musculoskeletal science. JRSM Short Rep 2012;3:1-9. [Google Scholar]
- 3.Malahias MA, Johnson EO, Babis GC, Nikolaou VS. Single injection of platelet-rich plasma as a novel treatment of carpal tunnel syndrome. Neural Regen Res 2015;10:1856-9. [Google Scholar]
- 4.Giroti C, Mittal A, Gotecha D. Comparison of steroid injection and platelet-rich plasma injection in the treatment of De-Quervain tenosynovitis. Int J Orthop Sci 2021;7:463-6. [Google Scholar]
- 5.Aspinen S, Nordback P, Anttila T, Stjernberg-Salmela S, Ryhänen J, Kosola J, et al. Platelet-rich plasma versus corticosteroid injection for treatment of trigger finger: Study protocol for a prospective randomized triple-blind placebo-controlled trial. Trials 2020;21:984. [Google Scholar]
- 6.Ranawat C, Straub LR. Volar tenosynovitis of wrist in rheumatoid arthritis. Arthritis Rheum 1970;13:112-7. [Google Scholar]
- 7.Wada A, Nomura S, Ihara F. Mycobacterium kansaii flexor tenosynovitis presenting as carpal tunnel syndrome. J Hand Surg Br 2000;25:308-10. [Google Scholar]
- 8.Vitale MA, Roden AC, Rizzo M. Tenosynovitis of the wrist and thumb and carpal tunnel syndrome caused by Histoplasma capsulatum: Case report and review of the literature. Hand (N Y) 2015;10:54-9. [Google Scholar]
- 9.Chen CH, Wu T, Sun JS, Lin WH, Chen CY. Unusual causes of carpal tunnel syndrome: Space occupying lesions. J Hand Surg (European Volume) 2012;37:14-9. [Google Scholar]
- 10.Shin WY, An MJ, Im NG, Oh KR, Choe Y, Yoon SR, et al. Changes in blood glucose level after steroid injection for musculoskeletal pain in patients with diabetes. Ann Rehabil Med 2020;44:117-24. [Google Scholar]
- 11.Hoberman AR, Cirino C, McCarthy MB, Cote MP, Pauzenberger L, Beitzel K, et al. Bone marrow-derived mesenchymal stromal cells enhanced by platelet-rich plasma maintain adhesion to scaffolds in arthroscopic simulation. Arthroscopy 2018;34:872-881. [Google Scholar]