SSN neuropathy is a rare condition. It is a frequently overlooked diagnosis in the setting of pain and dysfunction of the shoulder. Surgeons should be suspicious of the diagnosis in all patients with shoulder pathology of unclear etiology, especially in patients who participate in repetitive overhead activity.
Dr. Sagie Haziza, Department of Orthopaedic Surgery, 1611 NW 12th Street, University of Miami Hospital, Miami 33136, Florida. E-mail: sagiehaziza@gmail.com
Introduction: Supra-scapular nerve (SSN) neuropathy is a rare condition that can cause shoulder dysfunction. Prior literature has identified mass effect, space occupying lesions, trauma, and repetitive overhead activities as possible etiologies.
Cases Presentations: We report two cases of SSN neuropathy; a 21-year-old competitive female volleyball player with traction associated neuropathy and a 45-year-old male with a large paralabral ganglion cyst causing compressive neuropathy.
Conclusion: The following report highlights two different etiologies of SSN neuropathy and reviews the treatment of these conditions. Clinicians should consider SSN neuropathy in patients with unexplained shoulder pain and dysfunction.
Keywords: Suprascapular nerve neuropathy, suprascapular nerve entrapment, dynamic nerve compression, paralabral ganglion cyst.
Suprascapular nerve (SSN) neuropathy is a rare condition that is often forgotten in the setting of shoulder dysfunction [1, 2, 3]. Prior literature has identified mass effect, space occupying lesions, trauma including rotator cuff tears, repetitive overhead activities, and anatomical variants as possible primary or secondary etiologies [4, 5, 6, 7]. The prevalence of SSN neuropathy accounts for 1–2% of shoulder pain cases, with elite competitive athletes engaging in repetitive overhead activities at a higher risk [7, 8]. In this report, we examine two different etiologies of SSN neuropathy in patients who presented to an outpatient clinic and review the treatment of these conditions.
Patient 1
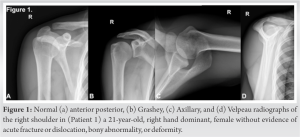
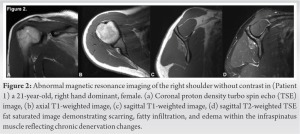
A 21-year-old, right hand dominant, female (85.7 kg) without medical history presented to outpatient sports medicine clinic with chronic right shoulder pain and weakness. The patient is a highly active student athlete competing on a Division I collegiate volleyball team as the outside hitter. In her final season, athletic trainers identified visible atrophy of the infraspinatus muscle and subjective dominant shoulder external rotation weakness without pain or discomfort. A full musculoskeletal exam was performed significant for reduced 4/5 right shoulder external rotation strength with considerable atrophy of the right infraspinatus muscle. Plain radiographs demonstrated no acute fractures or dislocations, without degenerative changes or obvious bony abnormality or deformity (Fig. 1). Magnetic resonance imaging (MRI) without contrast of the right shoulder demonstrated nonspecific scarring, fatty infiltration, atrophy, and edema of the infraspinatus muscle belly reflecting chronic denervation changes (Fig. 2). The fat planes surrounding the SSN at the level of the spinoglenoid and suprascapular notches were preserved without evidence of a paralabral cyst, compressive or hypertrophic ligamentous pathology, labral tear, or bony abnormality. There was mild insertional infraspinatus tendinosis with low grade 0.5 × 0.5 cm articular surface partial-thickness tear.
The patient was diagnosed with dynamic SSN injury due to traction at the spinoglenoid notch. She was advised to refrain from overhead activity for 6 weeks and a prescription for rotator cuff and periscapular strength rehabilitation was provided. Nonsteroidal anti-inflammatory drugs (NSAIDs) were prescribed to help reduce inflammation associated with potential neuritis. At 6-week follow-up, the patient was compliant with rehabilitation 5 times per week and was progressing well without pain or discomfort when performing overhead activities. Despite subjective improvement in external rotation strength, the atrophy and objective weakness persisted. A strict rehabilitation and strength conditioning program were recommended to enhance external rotation strength and limit overhead hitting as much as possible. She is currently 8-months from her initial presentation and has completed her senior year season; her function and performance have not declined; however, she has not regained full strength or muscle mass.
Patient 2
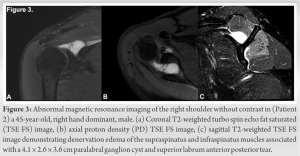
A 45-year-old, right hand dominant, male (83.9 kg) presented to clinic for acute right shoulder pain without identifiable traumatic event. The patient reported an intermittent achy sensation over his right long head of the bicep tendon and posterior shoulder with radiation to the ipsilateral elbow worse with shoulder abduction and internal rotation. He had previously trialed conservative management with NSAIDs and a physical therapy program without improvement. On physical examination, he reported tenderness to palpation over the bicep tendon and posterior shoulder. He demonstrated reduced 4/5 right shoulder external rotation strength without evidence of muscular atrophy. Plain radiographs demonstrated no acute fractures or dislocations, no degenerative changes, or obvious bony deformities. MRI without contrast of the right shoulder demonstrated denervation edema of the supraspinatus and infraspinatus muscles with an associated paralabral ganglion cyst extending from the supraspinatus fossa displacing the muscle belly of the supraspinatus superiorly and tracking inferiorly around the spinoglenoid notch. It measured 4.1 × 2.6 × 3.6 cm and corresponded with an anterior-based superior labrum anterior posterior (SLAP) tear. The rotator cuff tendons were intact (Fig. 3).
Surgical decompression of the cyst and labral repair was recommended and performed without complications. The SLAP tear was anteriorly based from the 12 to 2 O’clock position. The posterior labrum and bicep tendon was intact without abnormality. The cyst was identified protruding from the posterior capsular space posterosuperior to the glenoid, which was somewhat unusual as the clear SLAP pathology was anterior. We attempted to decompress the cyst from the anterior labral pathology by reflecting it off the anterior glenoid neck. There was a small release of cystic appearing fluid with this maneuver, but it did not achieve release of the obvious bulging cyst in the posterosuperior capsular space. We then made a small rent in the capsular tissue directly over the bulging cyst and just off the posterosuperior labrum, which achieved a large egress of cystic fluid and decompression of the bulging cyst. The area was milked with an arthroscopic probe releasing more fluid intra-articularly. The SLAP tear was repaired with suture anchors at the 12:30 and 1:30 positions paying attention not to strangulate the biceps anchor. The capsular incision was repaired in side-to-side fashion with a knotless, all-suture anchor placed into the posterior glenoid neck at the site of the rent. Physical therapy was initiated at the 1-week follow-up visit. At his 6-weeks follow-up visit, he reported improvement in pain and range of motion, but was not compliant with his physical therapy protocol. At 3-month follow-up, he reported continued improvement with only mild intermittent discomfort in the posterior shoulder, no tenderness to palpation, improved external rotation strength 5/5, and full range of motion. He was recommended to continue a home exercise program and all activity restrictions were removed. He is now 7-months post-operation and has had no complications or residual symptoms.
SSN neuropathy is a rare pathology resulting from compression or traction injury anywhere along the SSN course from the upper trunk of the brachial plexus to its motor insertions at the supraspinatus and infraspinatus muscles [2, 9]. Injury can result in nerve ischemia, conduction impairment, and if left untreated, may result in irreversible damage [2]. Injury typically occurs as the nerve passes through the suprascapular and spinoglenoid notches. Suprascapular notch compression leads to impairment of supraspinatus and infraspinatus muscles [1, 2, 9], In contrast, distal compression of SSN as it courses around the scapular spine at the spinoglenoid notch causes impairment of the infraspinatus muscle, exclusively [9]. Patients classically present with a gradual dull, achy pain in the posterior and lateral shoulder with weakness in abduction and external rotation, depending on location, and severity of injury [1, 9, 10]. On physical exam, supraspinatus and/or infraspinatus muscles atrophy along with shoulder abduction and external rotation deficits may be observed [11]. MRI is the preferred modality to assess for the pathologic cause of neuropathy [11]. Electromyography (EMG) and nerve conduction studies may be used as confirmatory studies [1, 11]. Identifying the causative etiology is necessary to determine the proper treatment approach [9].
Patient 1 was an elite competitive athlete performing repetitive overhead sport-specific activity resulting in traction associated SSN dysfunction. Conservative management is recommended for most patients with traction and dynamic overuse injuries with no focus of nerve compression [6, 9]. Treatment includes anti-inflammatory medications, activity modification, and physical therapy [1, 6, 9]. Many reports describe traction injury to SSN neuropathy in various overhead athletics including volleyball, golf, basketball, tennis, weight-lifting, and swimming [1, 12, 13, 14, 15, 16, 17, 18, 19, 20]. SSN neuropathy is more common in athletes playing volleyball with a prevalence of infraspinatus, supraspinatus muscle atrophy, and weakness in up to 20–45% of volleyball players compared to 12–33% across all athletes [12, 17, 21], The exact mechanism of injury is contentious. Some authors describe compression of the SSN during terminal shoulder external rotation and abduction, or cocking phase and subsequent follow through [16]. Using EMG and nerve conduction study of 35 professional beach volleyball players, Lajtai et al. described infraspinatus atrophy in 34% of participants and significant external rotation and elevation strength deficits in 90% and 93% of their cohort’s hitting shoulder, respectively [13]. EMG identified a greater latency in the hitting shoulder compared to the contralateral shoulder suggesting a demyelination mechanism [13]. The majority of prior literature evaluating SSN dysfunction in overhead athletes identifies isolated infraspinatus impairment from traction at the spinoglenoid notch as the most common cause. Patient 1 continues to respond well to non-surgical treatment. As she has now completed her volleyball career, we plan to monitor return of motor function and muscle mass.
Compression of the SSN from a paralabral cyst is the most common extrinsic or secondary cause of neuropathy. Compression neuropathy has been reported in patients with SLAP tears, ganglion cysts, Bennett lesion, ossified or hypertrophied superior transverse scapular and spinoglenoid ligaments [22, 23, 24], In a 2018 systematic review, Memon et al. report the most common cause of compressive SSN neuropathy was a cyst at the spinoglenoid notch identified in 42% of patients [23]. Paralabral cysts are often associated with labral tears and can cause compression of the SSN at the spinoglenoid notch or suprascapular notches [22, 25]. Authors have described arthroscopic and open decompressions of the suprascapular and/or spinoglenoid notch, including possible transverse scapular ligament release [11, 14]. Prior literature supports surgical decompression with improvement in pain, strength, and function; however, some authors report variable return of muscle strength and mass [9]. In our second patient, an arthroscopic approach was used to decompress the paralabral cyst and repair the labral tear resulting in pain reduction, and improved strength and function.
While SSN neuropathy is an infrequent pathology in the setting of shoulder dysfunction, it is important to be aware of the possible etiologies. SSN neuropathy can be difficult to diagnose and may mimics more common shoulder pathologies [7]. SSN neuropathy should be considered in all patients with unexplained shoulder pain and dysfunction, especially in patients performing repetitive overheard activities.
SSN neuropathy is a rare and overlooked condition in the setting of shoulder pain and dysfunction. This report describes two unique presentation of SSN neuropathy including the presenting signs, symptoms, and treatments, and discusses the clinical importance of suspecting the pathology.
References
- 1.Boykin RE, Friedman DJ, Higgins LD, Warner JJ. Suprascapular neuropathy. J Bone Joint Surg Am 2010;92:2348-64. [Google Scholar]
- 2.Cummins CA, Messer TM, Nuber GW. Suprascapular nerve entrapment. J Bone Joint Surg Am 2000;82:415-24. [Google Scholar]
- 3.Gosk J, Urban M, Rutowski R. Entrapment of the suprascapular nerve: Anatomy, etiology, diagnosis, treatment. Ortop Traumatol Rehabil 2007;9:68-74. [Google Scholar]
- 4.shah AA, Butler RB, Sung SY, Wells JH, Higgins LD, Warner JJ. Clinical outcomes of suprascapular nerve decompression. J Shoulder Elbow Surg 2011;20:975-82. [Google Scholar]
- 5.Reece CL, Varacallo M, Susmarski A. Suprascapular Nerve Injury. Treasure Island, FL: StatPearls Publishing LLC.; 2021. [Google Scholar]
- 6.Kostretzis L, Theodoroudis I, Boutsiadis A, Papadakis N, Papadopoulos P. Suprascapular nerve pathology: A review of the literature. Open Orthop J 2017;11:140-53. [Google Scholar]
- 7.Bozzi F, Alabau-Rodriguez S, Barrera-Ochoa S, Ateschrang A, Schreiner AJ, Monllau JC, et al. Suprascapular neuropathy around the shoulder: A current concept review. J Clin Med 2020;9:2331. [Google Scholar]
- 8.Memon AB, Dymm B, Ahmad BK, Sripathi N, Schultz L, Chandok A. Suprascapular neuropathy: A review of 87 cases. Muscle Nerve 2019;60:250-3. [Google Scholar]
- 9.Strauss EJ, Kingery MT, Klein D, Manjunath AK. The evaluation and management of suprascapular neuropathy. J Am Acad Orthop Surg 2020;28:617-27. [Google Scholar]
- 10.Martin SD, Warren RF, Martin TL, Kennedy K, O’Brien SJ, Wickiewicz TL. Suprascapular neuropathy. Results of non-operative treatment. J Bone Joint Surg Am 1997;79:1159-65. [Google Scholar]
- 11.Freehill MT, Shi LL, Tompson JD, Warner JJ. Suprascapular neuropathy: Diagnosis and management. Phys Sportsmed 2012;40:72-83. [Google Scholar]
- 12.Mazza D, Iorio R, Drogo P, Gaj E, Viglietta E, Rossi G, et al. Did the prevalence of suprascapular neuropathy in professional volleyball players decrease with the changes occurred in serving technique? Phys Sportsmed 2021;49:57-63. [Google Scholar]
- 13.Lajtai G, Wieser K, Ofner M, Raimann G, Aitzetmüller G, Jost B. Electromyography and nerve conduction velocity for the evaluation of the infraspinatus muscle and the suprascapular nerve in professional beach volleyball players. Am J Sports Med 2012;40:2303-8. [Google Scholar]
- 14.Plancher KD, Luke TA, Peterson RK, Yacoubian SV. Posterior shoulder pain: A dynamic study of the spinoglenoid ligament and treatment with arthroscopic release of the scapular tunnel. Arthroscopy 2007;23:991-8. [Google Scholar]
- 15.Sandow MJ, Ilic J. Suprascapular nerve rotator cuff compression syndrome in volleyball players. J Shoulder Elbow Surg 1998;7:516-21. [Google Scholar]
- 16.Miura K, Tsuda E, Ishibashi Y. Glenohumeral rotational deficit and suprascapular neuropathy in the hitting shoulder in male collegiate volleyball players. Prog Rehabil Med 2019;4:20190002. [Google Scholar]
- 17.Ferretti A, De Carli A, Fontana M. Injury of the suprascapular nerve at the spinoglenoid notch. The natural history of infraspinatus atrophy in volleyball players. Am J Sports Med 1998;26:759-63. [Google Scholar]
- 18.Young SW, Dakic J, Stroia K, Nguyen ML, Harris AH, Safran MR. High incidence of infraspinatus muscle atrophy in elite professional female tennis players. Am J Sports Med 2015;43:1989-93. [Google Scholar]
- 19.Witvrouw E, Cools A, Lysens R, Cambier D, Vanderstraeten G, Victor J, et al. Suprascapular neuropathy in volleyball players. Br J Sports Med 2000;34:174-80. [Google Scholar]
- 20.Holzgraefe M, Kukowski B, Eggert S. Prevalence of latent and manifest suprascapular neuropathy in high-performance volleyball players. Br J Sports Med 1994;28:177-9. [Google Scholar]
- 21.Challoumas D, Dimitrakakis G. Insights into the epidemiology, aetiology and associations of infraspinatus atrophy in overhead athletes: A systematic review. Sports Biomech 2017;16:325-41. [Google Scholar]
- 22.Moen TC, Babatunde OM, Hsu SH, Ahmad CS, Levine WN. Suprascapular neuropathy: What does the literature show? J Shoulder Elbow Surg 2012;21:835-46. [Google Scholar]
- 23.Memon M, Kay J, Ginsberg L, Simunovic N, Bak K, Lapner P, et al. Arthroscopic management of suprascapular neuropathy of the shoulder improves pain and functional outcomes with minimal complication rates. Knee Surg Sports Traumatol Arthrosc 2018;26:240-66. [Google Scholar]
- 24.Bautista JM, Fernandez-Jara J, Bautista SM, Fernandez-Miranda PM, Mora MV, San Jose BG, et al. Infraspinatus atrophy due to Bennett lesion causing suprascapular nerve palsy. J Ultrason 2021;21:e177-81. [Google Scholar]
- 25.Wee TC, Wu CH. Ultrasound-guided aspiration of a paralabral cyst at the spinoglenoid notch with suprascapular nerve compressive neuropathy. J Med Ultrasound 2018;26:166-7. [Google Scholar]