LPVNS of the ankle is a rare but important clinical entity and hindfoot endoscopy, when performed by an experienced ankle surgeon, is a safe and effective procedure for removal of LPVNS situated in posterior ankle recess.
Dr. Ivan Levaj, Department of Orthopaedic Surgery, University Hospital Centre Zagreb, Šalata 6-7, 10 000 Zagreb, Croatia. E-mail: ivanlevaj@gmail.com
Introduction: Pigmented villonodular synovitis (PVNS) is a rare and benign proliferative lesion affecting synovial lining of joints, bursae, and tendon sheaths. Depending on the extent of synovial involvement, two forms are distinguished, diffuse, and localized. Intra-articular localized form of PVNS (LPVNS) presents as a nodular, well circumscribed, pedunculated, or sessile soft-tissue mass.
Case Presentation: We report a case of an unusual localization of LPVNS in posterior ankle recess in a 42-year-old male with concomitant anterior ankle impingement syndrome. To address both the posterior and the anterior ankle disorders the patient was treated with combined two-portal endoscopic hindfoot approach and anterior ankle arthroscopy within the same operative session. The hindfoot endoscopy encompassed complete removal of the localized mass, partial synovectomy of the area at the base of the lesion, removal of os trigonum, and a loose body impinged in the interval between tibia and fibula. The anterior ankle arthroscopy included removal of the osteophytes from the anterior distal tibia and dorsal talus. Patient continued his normal daily and sporting activities without any restrictions and no recurrence of LPVNS 2 years after the surgery.
Conclusion: PVNS is an important clinical entity that should always be thought of as a differential diagnosis when treating patients with ankle disorders. Hindfoot endoscopy, when performed by an experienced ankle surgeon, is a safe and effective procedure for LPVNS of the posterior ankle recess, when deemed amenable to complete resection.
Keywords: Synovitis, pigmented villonodular, ankle, arthroscopy, hindfoot endoscopy.
Pigmented villonodular synovitis (PVNS) is a benign proliferative condition arising from synovial lining of joints, bursae, and tendon sheaths. It is a rare disease that can affect any age group but predominantly occurs in middle-age patients, with equal sex prevalence. In 1976, Granowitz et al. distinguished two forms of the disease, localized, and diffuse [1]. Their classification was based on macroscopic appearance and the extent of synovial involvement. Intra-articular localized PVNS (LPVNS) is described as nodular, well circumscribed, pedunculated, or sessile mass with focal synovial involvement, while diffuse PVNS (DPVNS) affects the entire synovium of the joint and is villous in nature. Microscopically, the two types show no clear difference. LPVNS is considerably less frequent compared to the DPVNS and represents only 6–11% of all PVNS cases. PVNS usually presents as a monoarticular disease of large joints. Knee is by far the most commonly affected joint, followed by hip, ankle, wrist, shoulder, and elbow [2]. The aim of this case report was to present a rare case of LPVNS localized in the posterior ankle recess that was excised using two-portal endoscopic hindfoot approach. The patient agreed to the publication of the data concerning the case.
A 42-year-old male presented to our outpatient clinic with a 2-year history of the right ankle stiffness, swelling, and intermittent catching and locking sensation. The patient’s medical history and family history were unremarkable. There was no history of trauma. Before the onset of symptoms, he played football regularly. On physical examination, there was a marked swelling of the right ankle. Passive and active dorsal and plantar flexion were reduced compared to the left ankle. Pain was elicited at extreme passive dorsiflexion and with direct palpation over the anterior ankle. The hyperplantarflexion test produced pain over the posterior aspect of the ankle and feeling of locking. The laxity observed with the anterior drawer maneuver was similar to that of the left ankle. Subtalar motion and midfoot motion were unrestricted and non-tender. Neurological and vascular examinations were normal.
Typical clinical findings on physical examination suggested anterior and posterior ankle impingement syndromes as most likely causes of patient’s symptoms, indicating further radiological investigations. Standard anteroposterior (AP) and lateral (LL) radiographs (Fig. 1) showed diffuse swelling of the ankle and osteophytes of the anterior distal tibia and dorsal talar neck. Os trigonum and unexpected soft-tissue mass were detected in the posterior ankle recess, behind the posterior process of the talus. Magnetic resonance imaging (MRI) of the ankle was performed to evaluate the soft-tissue mass (Fig. 2). MRI demonstrated a nodular lobulated soft-tissue mass in the posterior ankle recess measuring 29 × 18 × 19 mm. T1- and T2-weighted images showed heterogeneous mass, with predominantly low-to-intermediate signal intensity. PD-weighted images revealed a high signal intensity halo surrounding the low intensity signal mass. Furthermore, an additional bone fragment, which was not visible on standard AP and LL radiographs was detected on MRI. It was impinged between distal portion of tibia and fibula. Multislice computed tomography of the ankle was also performed to define the morphology of the bony lesions and help more accurate planning of surgical procedure. The patient’s history, clinical, and radiological findings helped to confirm the diagnosis of anterior and posterior ankle impingement syndromes with the presence of a loose body, impinged between tibia and fibula. Because of typical MRI findings for LPVNS, an excisional biopsy of the soft-tissue mass in the posterior ankle recess was indicated to confirm the diagnosis. Due to concurrent presence of anterior and posterior ankle pathology, we decided to use combined two-portal endoscopic hindfoot approach and anterior ankle arthroscopy within the same operative session. The procedure was executed with the patient under spinal anesthesia and in the prone position. A tourniquet was placed around his upper leg but was not inflated. This was done due to good experience of senior authors [3], who have previously described that not inflating the tourniquet, while using an arthroscopic pump, provides good visualization and good postoperative results in anterior ankle arthroscopy. The hindfoot endoscopy was performed through the posteromedial and posterolateral portals as described by van Dijk et al. [4], and by utilising a 4.0 mm 30° arthroscope. The portals were used interchangeably as viewing or working portals. At the level of subtalar joint, a well-encapsulated, pedunculated, and yellowish-brown nodule was observed. It was cut from the stalk with a radiofrequency wand and the mass was removed from the joint with a grasper (Fig. 3). The specimen was sent for histopathological analysis. Partial synovectomy was then performed at the base of the lesion with the help of a shaver and a radiofrequency wand to achieve complete macroscopic local clearance. Os trigonum and a loose body impinged in the interval between tibia and fibula were also extracted from the posterior ankle recess. After the completion of hindfoot endoscopy, the portals were sutured. The patient was then turned into a supine position, leaving all instruments on a sterile table. The foot and ankle were disinfected again, with new sterile draping applied. Once the patient was adjusted in the supine position, anterior ankle arthroscopy was performed using standard anteromedial and anterolateral portals utilizing a 2-portal dorsiflexion method. An arthroscopic shaver and a radiofrequency wand were used to debride hypertrophic synovium and fibrotic tissue in the anterior ankle recess, including the lateral and medial gutters. A combination of a shaver and a burr was then used to reshape the anterior distal tibia and dorsal talus to their native form. At the end of the procedure, a No. 12 closed suction drain was placed through the anterolateral portal into the joint and the portals were sutured.
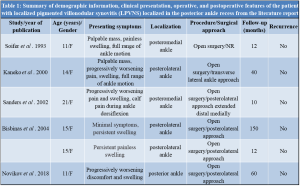
The drain was removed on the 1st postoperative day, when patient started with active and passive range of motion (ROM) exercises. A posterior splint with the ankle in the neutral position was used overnight for 3 weeks after the surgery. Weight-bearing as tolerated, with the support of crutches, was allowed for the first 3 weeks after surgery. It was followed by gradual progression to full weight-bearing over the next 3 weeks. During this period, patient underwent a course of physiotherapy, consisting of a ROM and strengthening exercises. Histopathological analysis confirmed that nodular mass found in the posterior recess of the ankle was indeed a LPVNS (Fig. 4). No recurrence was noted at the final follow-up, 2 years after the surgery. Patient was satisfied with the procedure. He continued playing football several times a week, without any restrictions.
We presented a case of LPVNS, found in posterior ankle recess that was successfully removed using two-portal endoscopic hindfoot approach. There is a consensus in the literature that LPVNS of the knee joint should be arthroscopically treated by removal of the localized mass and synovectomy of the area surrounding the base of the lesion [5, 6]. This has yet to be proven in the case of LPVNS of the ankle. However, there is a clear tendency in the literature toward arthroscopic treatment of LPVNS, when localized in anterior ankle recess [7, 8, 9, 10]. Our review of the recent literature on surgical management for LPVNS situated in the posterior ankle recess found only five case reports (six cases) (Table 1) [11, 12, 13, 14, 15]. In all six cases, LPVNS was managed using open surgical approaches and showed no recurrence, at the mean follow-up of 3.9 years. In 2000, van Dijk et al. [4] developed a two-portal technique for hindfoot endoscopy with the patient in the prone position, and although it is a relatively novel procedure, it has become an essential surgical method in the treatment of various posterior ankle and subtalar joint disorders. A great advancement introduced by this technique is the ability to reach several articular and periarticular structures in the posterior recess of the ankle and subtalar region through the two portals. However, hindfoot endoscopy is technically demanding surgical procedure which requires skills different from those usually required for arthroscopy when working inside a joint. The surgeon has to create a working space in the area external to the joint, normally occupied by fat and other soft tissues. The proximity of the tibial (medial) neurovascular bundle and sural nerve to the posteromedial and posterolateral portals raises the possibility of damage to these neurovascular structures, particularly when creating the working space needed in this type of approach. Nickisch et al. reported that out of 189 posterior ankle arthroscopies, injury to the tibial and sural nerve occurred in 7 cases (3.7%) in total, and from these only two (1.1%) failed to resolve [16]. Complication rates after hindfoot endoscopy reported by Zwiers et al. were similarly low with 1.8% of patients suffering a major complication and 5.4% of patients suffering a minor complication [17]. This is markedly better than the incidence of complications following open surgical treatment of posterior ankle impingement syndrome, which has been reported to be from 10% to 24% [18, 19]. Apart from the neurological problems, the most common complications of the hindfoot endoscopy are sinus tract formation, postoperative swelling, wound infection, and complex regional pain syndrome [20]. Adequate knowledge of regional anatomy, cadaver training, as well as careful pre-operative planning and standardized operative technique are of utmost importance to minimize the risk of these complications.
PVNS is an important clinical entity which every orthopedic surgeon should have heightened awareness of, particularly when treating patients with ankle disorders. Furthermore, LPVNS of the ankle, situated in posterior ankle recess, is amenable for arthroscopic treatment in the hands of experienced ankle surgeon. Complete removal of the localized mass and a partial synovectomy of the area at the base of the lesion should always be performed.
LPVNS is an important clinical entity. The diagnostic delay should be avoided by raising awareness of this entity among orthopedic surgeons, particularly those who treat patients with ankle disorders. Hindfoot endoscopy, when performed by an experienced ankle surgeon, is a safe and effective procedure for LPVNS of the posterior ankle recess.
References
- 1.Granowitz SP, D’Antonio J, Mankin HL. The pathogenesis and long-term end results of pigmented villonodular synovitis. Clin Orthop Relat Res 1976;114:335-51. [Google Scholar]
- 2.Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented villonodular synovitis: Radiologic-pathologic correlation. Radiographics 2008;28:1493-518. Available from: https://pubs.rsna.org /doi/10.1148/ rg.285085134 (Last accessed: 23 July 2022). [Google Scholar]
- 3.Dimnjaković D, Hrabač P, Bojanić I. Value of tourniquet use in anterior ankle arthroscopy: A randomized controlled trial. Foot Ankle Int 2017;38:716-22. Available from: https://journals.sagepub.com/ doi/ 10.1177/ 1071100717702461 (Last accessed: 23 July 2022). [Google Scholar]
- 4.van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for diagnosis and treatment of posterior ankle pathology. Arthroscopy 2000;16:871-6. Available from: https://www.arthroscopyjournal.org/article/S0749-8063(00)86731-6/fulltext (Last accessed: 23 July 2022). [Google Scholar]
- 5.Aurégan JC, Klouche S, Bohu Y, Lefèvre N, Herman S, Hardy P. Treatment of pigmented villonodular synovitis of the knee. Arthroscopy 2014;30:1327-41. Available from: https://www.arthroscopyjournal.org/article/S0749-8063(14)00404-6/fulltext (Last accessed: 23 July 2022). [Google Scholar]
- 6.Patel KH, Gikas PD, Pollock RC, Carrington RW, Cannon SR, Skinner JA, et al. Pigmented villonodular synovitis of the knee: A retrospective analysis of 214 cases at a UK tertiary referral centre. Knee 2017;24:808-15. Available from: https://www.thekneejournal.com/article/S0968-0160(17)30079-0/fulltext (Last accessed: 23 July 2022). 7 [Google Scholar]
- 7.Kubat O, Bojanić I, Smoljanović T. Localized pigmented villonodular synovitis of the ankle: Expect the unexpected. Foot Ankle Surg 2017;23:68-72. Available from: https://www.sciencedirect.com/science/article/abs/pii/S126877311630340X?via%3Dihub (Last accessed: 23 July 2022). [Google Scholar]
- 8.Kanatli U, Ataoglu MB, Özer M, Yildirim A, Cetinkaya M. Arthroscopic treatment of intra-articularly localised pigmented villonodular synovitis of the ankle: 4 cases with long-term follow-up. Foot Ankle Surg 2017;23:e14-9. Available from: https://www.sciencedirect.com/science/article/abs/pii/S1268773117300589?via%3Dihub (Last accessed: 23 July 2022). [Google Scholar]
- 9.Guo Q, Shi W, Jiao C, Xie X, Jiang D, Hu Y. Results and recurrence of pigmented villonodular synovitis of the ankle: Does diffuse PVNS with extra-articular extension tend to recur more often? Knee Surg Sports Traumatol Arthrosc 2018;26:3118-23. Available from: https://link.springer.com/article/10.1007/s00167-017-4488-8 (Last accessed: 23 July 2022). [Google Scholar]
- 10.Morelli F, Princi G, Rossato A, Iorio R, Ferretti A. Pigmented villonodular synovitis: A rare case of anterior ankle impingement. J Orthop Case Rep 2019;10:16-8. Available from: http://www.jocr.co.in/wp/2020/01/10/jocr-2020-v10-i01-1618 (Last accessed: 23 July 2022). [Google Scholar]
- 11.Soifer T, Guirguis S, Vigorita VJ, Bryk E. Pigmented villonodular synovitis in a child. J Pediatr Surg 1993;28:1597-600. Available from: https://www.sciencedirect.com/science/article/abs/pii/002234689390111W (Last accessed: 23 July 2022). [Google Scholar]
- 12.Kaneko K, Nakahara D, Tobe M, Iwase H, Inoue Y, Ohbayashi O, et al. Pigmented villonodular synovitis of the ankle in an adolescent. Int Orthop 2000;24:234-7. Available from: https://link.springer.com/article/10.1007/s002640000141 (Last accessed: 23 July 2022). [Google Scholar]
- 13.Sanders SM, Mandracchia VJ, Kimball DA, Rissman LJ. Pigmented villonodular synovitis. A literature review and unusual case report. Clin Podiatr Med Surg 2002; 19:527-40. Available from: https:// www.sciencedirect.com/ science/article/abs/ pii/ S0891842202000496?via%3 Dihub (Last accessed: 23 July 2022). [Google Scholar]
- 14.Bisbinas I, De Silva U, Grimer RJ. Pigmented villonodular synovitis of the foot and ankle: A 12-year experience from a tertiary orthopedic Oncology Unit. J Foot Ankle Surg 2004;43:407-11. Available from: https:// www.sciencedirect.com/science/article/abs/pii/S1067251604004491 (Last accessed: 23 July 2022). [Google Scholar]
- 15.Novikov D, Richardson MW, Ho C, Gould ES, Khan FA. A rare incidence of pigmented villonodular synovitis of the ankle in an adolescent. J Foot Ankle Surg 2018;57:1263-6. Available from: https://www.jfas.org/article/S1067-2516(18)30101-7/fulltext (Last accessed: 23 July 2022). [Google Scholar]
- 16.Nickisch F, Barg A, Saltzman CL, Beals TC, Bonasia DE, Phisitkul P, et al. Postoperative complications of posterior ankle and hindfoot arthroscopy. J Bone Joint Surg Am 2012;94:439-46. Available from: https:// journals.lww.com/jbjsjournal/ Abstract/2012/03070/Postoperative_Complications_of_Posterior_Ankle_and.8.aspx (Last accessed: 23 July 2022). [Google Scholar]
- 17.Zwiers R, Wiegerinck JI, Murawski CD, Smyth NA, Kennedy JG, van Dijk CN. Surgical treatment for posterior ankle impingement. Arthroscopy 2013;29:1263-70. Available from: https://www.arthroscopyjournal.org/article/S0749-8063(13)00065-0/fulltext (Last accessed: 23 July 2022). [Google Scholar]
- 18.Abramowitz Y, Wollstein R, Barzilay Y, London E, Matan Y, Shabat S, et al. Outcome of resection of a symptomatic os trigonum. J Bone Joint Surg Am 2003;85:1051-7. Available from: https://journals.lww.com/jbjsjournal/Abstract/2003/06000/Outcome_of_Resection_of_a_Symptomatic_Os_Trigonum.10.aspx (Last accessed: 23 July 2022). [Google Scholar]
- 19.Vilá J, Vega J, Mellado M, Ramazzini R, Golanó P. Hindfoot endoscopy for the treatment of posterior ankle impingement syndrome: A safe and reproducible technique. J Foot Ankle Surg 2014;20:174-9. Available from: https://www.sciencedirect.com/science/article/ abs/pii/S1268773114000393?via%3Dihub (Last accessed: 23 July 2022). [Google Scholar]
- 20.Zekry M, Shahban SA, El Gamal T, Platt S. A literature review of the complications following anterior and posterior ankle arthroscopy. J Foot Ankle Surg 2019;25:553-8. Available from: https://www.sciencedirect.com/science/article/abs/pii/S1268773118300791?via%3Dihu (Last accessed: 23 July 2022). [Google Scholar]