Liquid-nitrogen-frozen autograft is a feasible option in reconstruction of the bone defect arising from limb salvage surgery for osteosarcoma in low income countries.
Dr. Elijah N Muteti, Department of Orthopaedics and Rehabilitation, Moi University, Eldoret, Kenya/P. O. Box 1998-30100, Eldoret, Kenya. E-mail: enmuteti@gmail.com
Introduction: Limb salvage is a technically demanding and capital intensive procedure. In low-income countries, amputation followed by prosthesis use is widely used for the treatment of limb malignancies. This is associated with considerable morbidity and frequent non-adherence to prosthetic use. Therefore, we are reporting a case of osteosarcoma of the femur treated by the use of pre-operative chemotherapy, followed by frozen free femur autograft and intramedullary nailing, with excellent radiologic and functional results at 1 year of follow-up, in a developing country.
Case Report: A 16-year-old female presented with the left thigh swelling and pain for 3 months. X-ray of the left femur showed an osteosclerotic tumor in the medial aspect of the middle third of the left femur, diagnosed as osteogenic sarcoma on biopsy. Pre-operative chemotherapy was given. En bloc resection of the tumor was done. The cleaned femur shaft was frozen in liquid nitrogen, reimplanted, and stabilized with an intramedullary nail. One year after surgery, the femur osteotomy sites are fully united and the patient is fully ambulant, without evidence of metastasis or recurrence.
Conclusion: This case describes the successful use of a free frozen autograft of the femur in a 16-year-old girl with osteosarcoma of the left femur, done in a developing country, Kenya. It demonstrates the feasibility of limb salvage using this technique in low-income countries.
Keywords: Limb salvage, Liquid-nitrogen-frozen graft, Osteogenic sarcoma, Osteosarcoma
Limb salvage is considered a technically demanding and capital intensive procedure, though cost-effective in the long term [1]. In the low-income countries, amputation followed by prosthesis use is considered the more feasible option in the treatment of limb malignancies and is widely practiced [2, 3, 4]. Most patients do not prefer this option, which is associated with considerable morbidity and frequent non-adherence to prosthetic use [5]. Therefore, we are reporting this case of a 16-year-old girl with osteosarcoma of the left femur treated by the use of pre-operative chemotherapy, followed by liquid-nitrogen-frozen free femur autografting and intramedullary nailing, with excellent radiologic and functional results at 1 year follow-up.
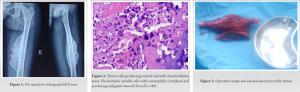
A 16-year-old female presented with the left thigh swelling and pain for 3 months. There was a palpable mass deep to the quadriceps muscle on the medial side of the thigh, but no evidence of metastasis. Complete blood cell count, erythrocyte sedimentation rate, C-reactive protein, and renal function tests were normal. X-ray of the left femur showed an osteosclerotic tumor in the medial aspect of the middle third of the left femur (Fig. 1). Open biopsy was done and histomorphologic evaluation of the sample revealed a tumor composed of pleomorphic spindle cells having a dense eosinophilic cytoplasm, marked nuclear atypia, and brisk mitotic activity. Areas of necrosis, deposition of thin, lace-like malignant osteoid, and chondroblastic differentiation were noted, features consistent with osteogenic sarcoma (Fig. 2).
CT scan of the chest and abdomen was normal. The left femur showed a mass measuring 10x5x5 cm in the medial aspect of the mid-femur. The cortex of the femur was thickened, sclerotic and the adjacent periosteum was involved. This sclerosis and ossification extended medially into the adjacent soft tissues, including the vastus medialis muscle, giving a sunburst appearance. The femoral neurovascular bundle was not involved by the tumor. No skip lesions were evident in the femur on magnetic resource imaging scan. Six cycles of pre-operative chemotherapy were given. The agents used were: cisplatin, doxorubicin, fosaprepitant, palonosetron, dexamethasone, mannitol, magnesium sulfate, and intravenous normal saline. Ensuing neutropenia was corrected with filgrastim. Neutropenic sepsis was treated using intravenous fluconazole, metronidazole, and augmentin. There was delay in initiating surgery and an additional two cycles of the same agents, keeping the cumulative doxorubicin dose to below 450 mg/m2. Limb salvage surgery was elected as treatment of choice for this patient; using a free, frozen femur shaft autograft technique and stabilization with an intramedullary nail. Two separate operating rooms that were adjacent to each other were prepared for this procedure, one for the patient and the other for the preparation of the autograft. With the assistance of a vascular surgeon, an anteromedial incision was made on the left thigh extending from the groin to the distal third of the femur, along the course of the left femoral artery. The previous biopsy incision scar was included in this incision in an ellipsoid fashion approximately 4 cm wide. The femoral neurovascular bundle was isolated and the tumor was dissected circumferentially leaving a 1 cm cuff of normal muscle tissue attached to it. A chevron osteotomy was made four fingerbreadths from the proximal and distal soft-tissue margin of the tumor, thus freeing the femoral diaphysis plus the encompassing tumor, from the rest of the left thigh tissues (Fig. 3). The specimen was stripped of all soft tissues. The tumor was bony hard, measuring 16 cm by 8 cm by 8 cm. It was shaved off the diaphysis using an orthopedic power saw, allowing visualization of the original femur cortex. This autograft femur diaphysis was reamed, washed and the intramedullary canal irrigated with saline. It was dipped intermittently in liquid nitrogen over the first 5 min and then left in the liquid nitrogen for 15 min. The now frozen graft was placed in a sterile open container for 10 min at room temperature allowing it to thaw, followed by placing it in distilled water. The femur autograft measured approximately 32 cm long (Fig. 4).
The femur autograft was replaced in the thigh, ensuring the chevron osteotomies fit well, and a locked intramedullary SIGN nail was placed (Fig. 5). A vacuum drain was left in situ. The incision was closed in layers. Thigh compression using crepe bandage was applied on the left thigh for 6 weeks. Radiographs done at 12 months post-operation demonstrated healing of the osteotomy sites with maintained implant position and the patient has normal lower limb function
(Fig. 7a, b).
Limb salvage requires resection of the tumor. This creates a bone defect that frequently requires reconstruction. The options of reconstruction include bone transport, vascularized fibula transplant, free frozen autograft, allograft, or endoprosthesis [6]. Bone transport is tedious requiring multiple procedures and is associated with frequent pin traction infections. Vascularized fibular transplant requires microvascular expertise which is not commonly available in low-income countries. Femur shaft replacement with an endoprosthesis was too expensive and, due to its non-biological nature in a young person, may fail with time. Therefore, frozen autograft was chosen as the method of choice. A pedicle frozen autograft would have been ideal, but being a first case and the accompanying unfamiliarity with the handling of liquid nitrogen made the authors choose free freezing that could be done in a separate room, away from the patient and the rest of the theater team. This is the first case, to the best of our knowledge treated by free frozen autograft in our country and possibly in the Sub-Saharan Africa region.
The first records of cryotherapy were by Cooper in 1962. His techniques have been modified and recorded extensively in Japan. Tsuchiya et al. described the pedicle frozen autograft technique [7]. The advantages of autograft are that it is a one-time operation, the fit of the autograft is perfect since it is biological and likely to incorporate fully [8, 9]. Liquid nitrogen is readily available in Kenya, because it is used by veterinarians for artificial insemination of cows. The cost is affordable. However, there are risks inherent with this technique. The operator needs to be aware of the risks of handling liquid nitrogen including hypoxia, contact burns, and bone graft explosion [10]. Infection may occur and this was prevented by meticulous surgical technique, compression of the thigh to prevent seroma formation and prolonged post-operative antibiotics. Failure of fixation is higher with the use of an intramedullary nail, compared with use of a plate as recommended by Tsuchiya. An appropriate locking plate was not available, coupled with the surgeon familiarity with the sign nailing technique in femur shaft fracture, and made the surgeons choose this technique over plating. Graft fracture can occur and this plus late infections warrant prolonged follow-up in these patients. Certainly, the fusion evident at 1 year and the full range of active motion at the knee is very encouraging to the authors. This is in spite of significant excision of portions of the vastus intermedius and vastus medialis. We believe the young age of the patient, availability of chemotherapy/ oncology treatment, and coupled with the relatively less aggressive nature of this supposedly parosteal type of osteosarcoma contributed to a favorable outcome in this particular patient. Long-term follow-up is clearly mandatory. The authors would encourage utilization of liquid nitrogen frozen autograft as a viable alternative in our set up for limb salvage in well-selected patients.
This case describes the successful use of liquid-nitrogen-frozen free femur autograft in osteosarcoma of the femur, done in a developing country, Kenya, with preservation of lower limb function for 1 year.
We advocate for the use of liquid-nitrogen-frozen autograft in the treatment of limb malignancies in low-income countries, in an effort to avoid amputations and save limb function.
References
- 1.Grimer RJ, Carter SR, Pynsent PB. The cost-effectiveness of limb salvage for bone tumours. J Bone Joint Surg 1997;79:558-61. [Google Scholar]
- 2.Morris SC, Nelson S, Zuckerman LM. Limb salvage for musculoskeletal tumors in the austere environment: Review of the literature with illustrative cases regarding considerations and pitfalls. J Am Acad Orthop Surg Glob Res Rev 2020;4:1-11. [Google Scholar]
- 3.Lisenda L, Linda ZA, Snyman FP, Kyte RD, Lukhele M. Osteosarcoma patient outcomes at a South African tertiary hospital. S Afr Med J 2017;107:754-7. [Google Scholar]
- 4.Muteti EN, Busakhala N, Vadgama H, Lagat D. Forequarter amputations at the Moi teaching and referral hospital. East Afr Orthop J 2018;12:16-9. [Google Scholar]
- 5.Baars EC, Schrier E, Dijkstra PU, Geertzen J. Prosthesis satisfaction in lower limb amputees: A systematic review of associated factors and questionnaires. Medicine (Baltimore) 2018;97:e12296. [Google Scholar]
- 6.Fritz J, Fishman EK, Corl F, Carrino JA, Weber KL, Fayad LM. Imaging of limb salvage surgery. AJR Am J Roentgenol 2012;198:647-60. [Google Scholar]
- 7.Tsuchiya H, Nishida H, Srisawat P, Shirai T, Hayashi K, Takeuchi A, et al. Pedicle frozen autograft reconstruction in malignant bone tumors. J Orthop Sci 2010;15:340-9. [Google Scholar]
- 8.Yazawa Y, Imanishi J, Torigoe T. Limb salvage using liquid nitrogen-treated autologous bone graft in sarcoma surgery. Jpn J Med 2018;1:239-42. [Google Scholar]
- 9.Zekry KM, Yamamoto N, Hayashi K, Karem M, Takeuchi A, Higuchi T, et al. Intercalary frozen autograft for reconstruction of malignant bone and soft tissue tumours. Int Orthop 2017;41:1481-7. [Google Scholar]
- 10.Office of the Vice President for Research. Liquid nitrogen handling. In: Environmental Health and Safety. Iowa: University of Iowa; 1847. [Google Scholar]