Primary intraosseous low-grade myxofibrosarcomas radiologically mimic enchondromas and the MRI features that distinguish the former from the latter include low ADC values and slow progressive contrast enhancement.
Dr. Sanjay Desai, Consultant Musculoskeletal Radiologist, Deenanath Mangeshkar Hospital, Eradhwane, Pune - 411 004, Maharashtra, India. E-mail: drsanjaydesai@gmail.com
Introduction: Low-grade myxofibrosarcoma (LGMFS) is a neoplasm of soft tissues. According to the World Health Organization, LGMFS is a malignant myofibroblastic tumor arising from deep soft tissues with potential for recurrence and late metastatic spread. The incidence estimates are 0.18/million, accounting for 0.6% of all soft-tissue sarcomas. It can directly invade the bone and metastasize to bone; however, primary osseous low-grade myxofibrosarcoma is a rare entity. Thus, recognizing atypical presentations of uncommon neoplasms are a pertinent skill for the radiologist due to significant implications for management.
Case Report: A 40-year-old male with complaints of midfoot pain was referred to radiology department for imaging. Radiographs of the foot showed a lytic mildly expansile lesion in the first metacarpal with wide zone of transition and no sclerotic margin or matrix calcification. Magnetic resource imaging (MRI) and computed tomography (CT) examination demonstrated well defined lobulated lesion which appeared heterogeneously hyperintense on T2W images with cortical breach, extraosseous soft-tissue component, and early rapid progressive enhancement. The radiological diagnosis of enchondroma with pathological fracture was considered. Atypical findings of early progressive enhancement and extraosseous soft-tissue component were, however, incongruous with enchondroma and possibility of an aggressive/malignant etiology was also considered. Hence, the lesion was biopsied and diagnosis of LGMFS was made and subsequently confirmed on excised specimen. Follow-up CT scan post 6 months of surgical resection demonstrated no recurrence.
Conclusion: Primary osseous LGMFS is a rare entity and radiologically mimics enchondromas. Both LGMFS and enchondromas show T2W hyperintensity. MRI features that distinguish LGMFS from enchondroma include low apparent diffusion coefficient values and slow progressive enhancement in dynamic contrast-enhanced MRI.
Keywords: Apparent diffusion coefficient, computed tomography, enchondroma, magnetic resource imaging, myxofibrosarcoma, radiograph.
Low-grade myxofibrosarcoma (LGMFS) according to the World Health Organization is a malignant fibroblastic/myofibroblastic tumor arising from deep soft tissues with potential for recurrence and late metastatic spread [1, 2]. The incidence estimates are 0.18/million, accounting for 0.6% of all soft-tissue sarcomas [3]. Primary osseous myxofibrosarcoma is a rare pathology of bones especially in metatarsals which radiologically mimics enchondroma [4]. We have limited understanding of its presentation and course owing to sporadic reports in the literature. These are low-grade malignancies and show low risk of metastasis with high potential for local recurrence [5, 6]. With every recurrence, they are associated with increased risk of metastasis. Hence, they need to be differentiated from enchondromas by magnetic resource imaging (MRI) evaluation. Recognizing atypical presentations of uncommon neoplasms are a pertinent skill for the Musculoskeletal Radiologist, due to significant implications for management. We highlight the need to maintain an index of suspicion especially in the setting of discordant findings. Unclear diagnosis must be diligently followed up.
A 40-year-old male, otherwise well, presented with recent onset pain in midfoot region. Physical examination revealed non-palpable mass. No constitutional symptoms of fever or weight loss were present. Hemoglobin was 15 g %, red blood cells 5.15 × 1012/L, total blood count was 9000 × 109/L, and erythrocyte sedimentation rate 10 mm/h. Patient was referred to radiology department for imaging. Radiographs of the foot showed a lytic expansile lesion in first metacarpal with wide zone of transition, no sclerotic margin, and no matrix calcification (Fig. 1). Subsequently, the patient was referred for a MRI examination with computed tomography (CT) correlation to further characterize the lesion. The lesion was well defined, lobulated with endosteal scalloping. It was heterogeneously hyperintense on T2W images, hypointense on T1W images, with slow progressive peripheral nodular enhancement in dynamic contrast-enhanced MRI (DCEMRI) curves, and area of cortical breach with extraosseous soft-tissue component (Fig. 2a, b, 3, 4). Few areas of diffusion restriction were noted within the lesion (Fig. 5).
Subsequently, the patient was referred for a MRI examination with computed tomography (CT) correlation to further characterize the lesion. The lesion was well defined, lobulated with endosteal scalloping. It was heterogeneously hyperintense on T2W images, hypointense on T1W images, with slow progressive peripheral nodular enhancement in dynamic contrast-enhanced MRI (DCEMRI) curves, and area of cortical breach with extraosseous soft-tissue component (Fig. 2a, b, 3, 4). Few areas of diffusion restriction were noted within the lesion (Fig. 5).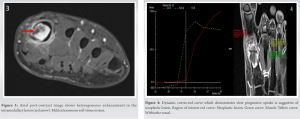
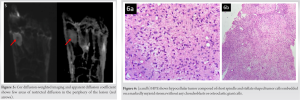
In view of above findings, the radiological diagnosis of enchondroma with a pathological fracture was made. However, due to atypical presentation of the lesion (heterogeneous hyperintensity on T2W images, early progressive peripheral nodular enhancement, extraosseous soft-tissue component, and areas of diffusion restriction), a possibility of aggressive/ malignant etiology was also considered and, hence, a biopsy was performed. The biopsy demonstrated a hypocellular tumor composed of short spindle and stellate shaped tumor cells embedded on a markedly myxoid stroma without any chondroblasts or osteoclastic giant cells on HPE (Fig. 6a and b). Diagnosis of LGMFS was made. Immunohistochemistry was positive for smooth muscle antigen, vimentin and negative for synaptophysin-100, cluster of differentiation 34, desmin (Fig. 7a and b). MiB-1 labeling index was focally high (10–25%).
Surgical excision was further carried out. The patient underwent surgical removal of first metatarsal proximal to tumor along with fibular grafting. The specimen was a greyish-white hard mass measuring 3.3 × 1.5 × 2 cm. There was no particular breach. Diagnosis of LGMFS was confirmed on the excised specimen.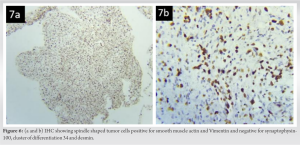
The patient was discharged and was advised to come for follow-up after 6 months. The patient was also advised to come to the hospital earlier in case of any increased pain or fever. Follow-up CT post 6 months of surgical resection demonstrated no recurrence or metastases.
Low-grade fibromyxoid sarcomas are malignant fibroblastic soft-tissue tumors with fibrous and myxoid elements. Another term for the same is Evans tumor. Their incidence is underestimated as they mimic other soft-tissue tumors; however, they are relatively rare.
LGMFS is seen in a wide age range but occur mostly in young adults and adolescents. Men are more commonly affected than female [7]. They typically manifest as a painless slow-growing mass. LGMFS commonly arise from the subfascial soft tissues of proximal extremities. In pediatric age group, superficial soft-tissues of the head-and-neck are commonly involved [7, 8]. Bone invasion by a primary tumor is rarely reported [9, 10, 11]. Surgery is the mainstay of treatment; however, local recurrence is common as seen in almost 50% of the cases [12, 13]. There is direct association with grade of tumor and rate of local recurrence, which implies higher the grade, more the risk of metastases [14, 15].
Although myxofibrosarcoma is known to metastasize to the bone [12], the incidence of primary osseous myxofibrosarcoma is rare, with only a few cases reported in the literature. In 1988, Frassica et al. published the first case of primary osseous myxofibrosarcoma. The case was of a tumor arising in the left distal femur in a middle-aged male [15]. Later, in 1997 and 2002, two more cases of myxoid malignant fibrous histiocytoma of the skull were described [16, 17]. Romeo et al. in 2012 re-evaluated previously diagnosed “malignant fibrous histiocytoma” or “fibrosarcoma” of bone, and three of them were reclassified as myxofibrosarcoma of bone [18].
Enchondromas aka chondromas [19] are common intramedullary cartilage tumors with benign imaging features. They are commonly detected in pediatric age group and young adults. Enchondromas are the most common benign primary bone neoplasms of extremities (hands/feet) and are commonly seen as well-circumscribed lobulated masses with sharp borders [20]. On MR imaging, these shows T2 hyperintense signal with internal foci of low signal of “rings and arcs”, suggestive of chondroid matrix.
Both LGMFS and enchondromas show hyperintensity on T2 weighted fat saturated images and can be associated with pathological fractures. However, LGMFS is heterogeneous on T2W images with varying amounts of myxoid and fibrous components. (Myxoid component being hyperintense and fibrous component being hypointense on T2W images) [8, 21, 22]. Radiologically, LGMFS mimics a chondroid lesion; however, few pointers which would help to differentiate the two and are preferentially seen in LGMFS – (1) Heterogeneous signal on T2W images (few areas being hypointense due to fibrous element), (2) low apparent diffusion coefficient (ADC) values, and (3) slow progressive enhancement. Thus, every lesion which is lobulated having endosteal scalloping and is hyperintense on T2W images should not be thought of as only a chondral lesion [23].
LGMFS radiologically mimics enchondromas. Both show T2W hyperintensity and can be associated with pathological fractures. MRI features that distinguish LGMFS from enchondroma include low ADC values and slow progressive enhancement in DCEMRI. With every recurrence, LGMFS is associated with increased risk of metastasis; hence, the importance of differentiation between the them.
Every lesion which is lobulated having endosteal scalloping and is hyperintense on T2W images should not be thought of only as a chondral lesion. LGMFS radiologically mimic enchondromas; however, MRI features that distinguish LGMFS from enchondroma include low ADC values and slow progressive enhancement in DCEMRI. LGMFS is known to recur and every recurrence is associated with increased risk of metastasis, hence, the importance of this case report.
References
- 1.Kurisaki-Arakawa A, Suehara Y, Arakawa A, Takagi T, Takahashi M, Mitani K, et al. Deeply located low-grade fibromyxoid sarcoma with FUS-CREB3L2 gene fusion in a 5-year-old boy with review of literature. Diagn Pathol 2014;9:163. [Google Scholar]
- 2.Doyle LA, Möller E, Cin PD, Fletcher CD, Mertens F, Hornick JL. MUC4 is a highly sensitive and specific marker for low-grade fibromyxoid sarcoma. Am J Surg Pathol 2011;35:733-41. [Google Scholar]
- 3.Maretty-Nielsen K, Baerentzen S, Keller J, Dyrop HB, Safwat A. Low-grade fibromyxoid sarcoma: Incidence, treatment strategy of metastases, and clinical significance of the FUS gene. Sarcoma 2013;2013:256280. [Google Scholar]
- 4.Finos L, Righi A, Frisoni T, Gambarotti M, Ghinelli C, Benini S, et al. Primary extraskeletal myxoid chondrosarcoma of bone: Report of three cases and review of the literature. Pathol Res Pract 2017;213:461-6. [Google Scholar]
- 5.Goel K, Slipak A, Ercolano L, Silverman JF, Tang BT. Primary osseous low-grade myxofibrosarcoma of clavicle presenting with multiple skeletal metastases. Cureus 2020;12:e10170. [Google Scholar]
- 6.Tsuchie H, Kaya M, Nagasawa H, Emori M, Murahashi Y, Mizushima E, et al. Distant metastasis in patients with myxofibrosarcoma. Ups J Med Sci 2017;122:190-3. [Google Scholar]
- 7.Wang L, Li L, Chen DQ, Yang L, Li SK, Cheng C. Low-grade myofibroblastic sarcoma: Clinical and imaging findings. BMC Med Imaging 2019;19:36. [Google Scholar]
- 8.Sargar K, Kao SC, Spunt SL, Hawkins DS, Parham DM, Coffin C, et al. MRI and CT of low-grade fibromyxoid sarcoma in children: A report from children’s oncology group study ARST0332. AJR Am J Roentgenol 2015;205:414-20. [Google Scholar]
- 9.Li W, Li D, Zhu X, Lu S, He C, Yang Q. Low-grade myxofibrosarcoma following a metal implantation in femur: A case report. Diagn Pathol 2014;9:6. [Google Scholar]
- 10.Park SW, Kim HJ, Lee JH, Ko YH. Malignant fibrous histiocytoma of the head and neck: CT and MR imaging findings. AJNR Am J Neuroradiol 2009;30:71-6. [Google Scholar]
- 11.Murphey MD, Gross TM, Rosenthal HG. From the archives of the AFIP. musculoskeletal malignant fibrous histiocytoma: Radiologic-pathologic correlation. Radiographics 1994;14:807-26. quiz 827-8. [Google Scholar]
- 12.Jo VY, Fletcher CD. WHO classification of soft tissue tumours: An update based on the 2013 (4th) edition. Pathology 2014;46:95-104. [Google Scholar]
- 13.Mentzel T, Calonje E, Wadden C, Camplejohn RS, Beham A, Smith MA, et al. Myxofibrosarcoma. Clinicopathologic analysis of 75 cases with emphasis on the low-grade variant. Am J Surg Pathol 1996;20:391-405. [Google Scholar]
- 14.Kayser D, Walton Z, Bruner E, Chapin RW. Myxofibrosarcoma: First report of myxofibrosarcoma of bone arising at a bone infarct. Skeletal Radiol 2017;46:1143-7. [Google Scholar]
- 15.Frassica FJ, Sim FH, Wold LE. Case report 462: Grade 2 myxoid fibrosarcoma of femur. Skeletal Radiol 1988;17:77-80. [Google Scholar]
- 16.Nakayama K, Nemoto Y, Inoue Y, Mochizuki T, Soares SB Jr, Ohata K, et al. Malignant fibrous histiocytoma of the temporal bone with endocranial extension. AJNR Am J Neuroradiol 1997;18:331-4. [Google Scholar]
- 17.Woodhams R, Kan S, Iwabuchi K, Oka H, Sagiuchi T, Hayakawa K. A case of malignant fibrous histiocytoma (MFH) in the skull bone presenting extensive permeative osteolysis. Radiat Med 2002;20:141-5. [Google Scholar]
- 18.Romeo S, Bovee JV, Kroon HM, Tirabosco R, Zanatta L, Mertens F, et al. Malignant fibrous histiocytoma and fibrosarcoma of bone: A reassessment in the light of currently employed morphological, immunohistochemical and molecular approaches. Virchows Arch 2012;461:561-70. [Google Scholar]
- 19.Douis H, Saifuddin A. The imaging of cartilaginous bone tumours. I. Benign lesions. Skeletal Radiol 2012;41:1195-212. [Google Scholar]
- 20.Walden MJ, Murphey MD, Vidal JA. Incidental enchondromas of the knee. AJR Am J Roentgenol 2008;190:1611-5. [Google Scholar]
- 21.Yue Y, Liu Y, Song L, Chen X, Wang Y, Wang Z. MRI findings of low-grade fibromyxoid sarcoma: A case report and literature review. BMC Musculoskelet Disord 2018;19:65. [Google Scholar]
- 22.Petscavage-Thomas JM, Walker EA, Logie CI, Clarke LE, Duryea DM, Murphey MD. Soft-tissue myxomatous lesions: Review of salient imaging features with pathologic comparison. Radiographics 2014;34:964-80. [Google Scholar]
- 23.Antonescu CR, Argani P, Erlandson RA, Healey JH, Ladanyi M, Huvos AG. Skeletal and extraskeletal myxoid chondrosarcoma: A comparative clinicopathologic, ultrastructural, and molecular study. Cancer 1998;83:1504-21. [Google Scholar]









