It's a very rare injury and easily missed; leading to unnecessary deadly complications.
Dr. Harsh Kotecha, Department of Orthopaedics, MGM Medical College, Kamothe, Navi-Mumbai - 410209, Maharashtra, India. E-mail: kotecha611@gmail.com
Introduction: This article reports a case of surgical repair of traumatic rupture of tibialis posterior (TP) tendon in a young healthy male after alleged history of grinder (heavy machine) injury over the foot, with the help of a suture anchor and running whip stitch followed by immobilization in a below knee slab postoperatively. The acute rupture of the TP tendon (TPT), compared to an acute rupture of the Achilles tendon, is a quite uncommon disease to be diagnosed in the emergency department setting. In most cases symptoms related to a TP dysfunction, like weakness, pain along the course of the tendon, swelling in the region of the medial malleolus, and the partial or complete loss of the medial arch with a flatfoot deformity precede the complete rupture of the tendon.
Case Report: A 32-year-old healthy male presented to the outpatient clinic with a history of pain and swelling in the right foot for 10 months after alleged history of sustaining a grinder (heavy machine) injury to the medial aspect of the right foot 10 months ago. Anteroposterior and oblique radiographs of the right foot suggestive of no skeletal pathology and patient was managed conservatively with analgesic, anti-inflammatory, and compression bandaging. A magnetic resource imaging of the right foot was advised after no relief of symptoms and was suggestive of high-grade tear of the distal tibialis posterior tendon from the level of medial malleolus to its insertion. Surgical repair of the TPT was planned with a suture anchor placed in the navicular bone. The procedure was carried out under spinal anesthesia and there were no complications in the intraoperative or post-operative period. Patient was given a below knee slab with the foot in inversion postoperatively which was revised into a below knee cast with foot in inversion. Six-week post-operative follow-up, cast was removed and physiotherapy was started for the patient that included Active Ankle ROM and Gait Training, patient had a Modified Olerud and Molander Score of 45/100. Six-month post-operative follow-up, patient was relieved of chronic pain and was able walk and stand on his toes without pain and showed significant improvement in gait with Modified Olerud and Molander Score 90/100.
Conclusion: The TPT is the main dynamic stabilizer of the medial longitudinal arch of the foot. With appropriate surgical technique, adequate post-operative immobilization followed by physiotherapy surgical repair of the TPT helped alleviate the chronic pain experienced by the patient during weight bearing activities.
Keywords: traumatic, tibialis, posterior, surgical, repair.
The tibialis posterior (TP) tendon elevates the medial arch and inverts, adducts, and plantar flexes the foot. During the stance phase of gait, the TP is the main dynamic stabilizer of the foot. As a strong contributor to the midtarsal joint locking mechanism, the TP tendon (TPT) inverts the hindfoot, creating a rigid midfoot allowing the gastrocnemius-soleus complex to transmit plantar flexion forces to the metatarsal heads. The TP muscle arises from the interosseous membrane and adjacent surfaces of the proximal tibia and fibula. The myotendinous junction appears in the distal third of the leg. The TPT courses behind the medial malleolus at a relatively acute angle and further passes posterior to the axis of the tibiotalar joint and medial to the axis of the subtalar joint. From an anatomical point of view, the main insertion of the TPT is at the navicular bone [1].
The acute rupture of the TPT, compared to an acute rupture of the Achilles tendon, is a quite uncommon disease to be diagnosed in the emergency department setting. Complete traumatic rupture of the TPT is a rare condition, which can be easily missed in the emergency department setting with only six cases reported since 1995. The pathogenic mechanism leading to the rupture of an apparently healthy tendon is generally a trauma in pronation and external rotation and, less frequently, a direct trauma to the ankle. Signs and symptoms of a TP insufficiency, like swelling and pain along the course of the tendon with or without a progressive loss of the medial arch, swelling in the region of the medial malleolus indicate in some cases a TP rupture [2]. In this case report, we describe a traumatic rupture of TPT following alleged history grinder (heavy machine) Injury to the medial aspect of the right foot with no associated fractures.
A 32-year-old healthy male presented to the outpatient clinic with a history of pain and swelling in the Right foot for 10 months after alleged history of sustaining a grinder (heavy machine) injury to the medial aspect of the right foot 10 months ago. At the time of injury, the patient sustained a contused lacerated wound approximately 3 × 0.5 × 0.5 cm in size over the medial aspect of the right foot and visited the emergency department at a local hospital. Anteroposterior and oblique radiographs of the right foot and anteroposterior, lateral, and mortise radiographs of the right ankle suggested no fractures or skeletal abnormalities. The CLW was sutured, and dressing was done, and the patient was managed conservatively with analgesic, anti-inflammatory, and compression bandaging. One month following the injury, the patient started experiencing a dull aching persistent, non-radiating pain in the right foot which was insidious in onset; aggravated on weight bearing, and relieved on taking rest. A magnetic resource imaging (MRI) of the right foot was advised after no relief of symptoms with conservative management. The MRI showed a high-grade tear of the distal TPT from the level of medial malleolus to its insertion and was planned for operative management of TPT tear.
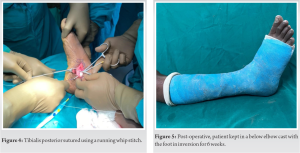
After anesthetic workup, patient was posted for surgery and operated with open repair of TPT using suture anchor. After administration of spinal anesthesia, a 5 cm incision (Fig. 1) was taken over the right foot beginning from the tip of the medial malleolus extending distally and curved anteriorly till the navicular bone. Superficial dissection was carried out and the fibers of TP were identified (Fig. 2), alternate sliding tenotomy, and lengthening carried out for the proximal end of the TPT. A 2.5 mm suture anchor (Fig. 3) was fixed in the navicular bone and fibers of TPT were sutured using a running whip stitch (Fig. 4). There were no complications in the intraoperative or post-operative period. Patient was given a below knee slab with the foot in inversion postoperatively.
After removal of sutures, the slab was revised into a below knee cast with the foot in inversion (Fig. 5) for 6 weeks.
The patient’s assessment was carried out based on Modified Olerud and Molander Score. Six-week post-operative follow-up, cast was removed, and physiotherapy was started for the patient that included active ankle ROM and gait training, patient had a Modified Olerud and Molander Score of 45/100 (Table 1) at 6 weeks. At 6-month post-operative follow-up, patient was relieved of chronic pain and was able walk and stand on his toes without pain and showed significant improvement in gait with Modified Olerud and Molander Score 90/100 (Table 2).
The isolated rupture of the tendon, with no clinical and radiological signs of a flatfoot deformity, is uncommon but should nevertheless be considered in the emergency department. The clinical evaluation in this setting should include an appropriate medical history taking (signs of TPT dysfunction) with plain radiographic examination. Clinical evaluation alone may not be sufficient in diagnosing acute TPT rupture and magnetic resonance imaging might be helpful in the immediate management of TPT rupture for early surgical repair [2]. Surgical repair of TPT, in whom conservative treatment has failed, replacement or augmentation of the deficient posterior tibial tendon has been recommended by itself or in conjunction with other procedures, including medial displacement calcaneal osteotomy, lateral column lengthening through the calcaneus, or calcaneocuboid joint, subtalar arthrodesis, and triceps surae lengthening. While the use of other tendons including the flexor hallucis longus and peroneus brevis has been described, the flexor digitorum longus (FDL) is most frequently used because of its proximity and less essential primary function and involves transfer of the FDL tendon through a tunnel in the navicular. Fixation often is obtained by sewing the tendon back onto itself. An alternative technique for fixing the posterior tibial tendon into a navicular tunnel with a suture anchor requires less FDL tendon length and dissection than the standard tendon-to-tendon technique [3].
In our review of literature, although uncommon, operative management in cases of isolated TPT without associated medial malleolus fracture or deformity is advocated to relieve chronic pain in the foot.
The TPT is the main dynamic stabilizer of the medial longitudinal arch of the foot [2] With appropriate surgical planning and technique, adequate post-operative immobilization followed by physiotherapy, surgical repair of the TPT helped alleviate the chronic persistent pain experienced by the patient during his day-to-day activities and return to his pre-injury status.
Diagnosing a case of acute traumatic rupture of TPT can be challenging. Complete traumatic rupture of the TPT is a rare condition, routine radiographs are often misleading. A detailed evaluation is essential.
References
- 1.Willegger M, Seyidova N, Schuh R, Wihndhager R, Hirtler L. The tibialis posterior tendon footprint: An anatomical dissection study. J Foot Ankle Res 2020;13:25. [Google Scholar]
- 2.Martinelli N, Bonifacini C, Bianchi A, Moneghini L, Scotto G, Sartorelli E. Acute rupture of the tibialis posterior tendon without fracture. J Am Podiatric Med Assoc 2014;104:298-301. [Google Scholar]
- 3.Sullivan RJ, Gladwell HA, Aronow MS, Nowak MD. An in vitro study comparing the use of suture anchors and drill hole fixation for flexor digitorum longus transfer to the navicular. Foot Ankle Int 2006;27:363-6. [Google Scholar]