The diagnosis and treatment of bilateral anterior hip dislocation as an emergency to avoid complications.
Dr. Yogesh Ahuja, Senior Resident, Shri Guru Ram Rai Institute of Medical and Health Sciences, Dehradun - 248 001, Uttarakhand, India. E-mail: dryogeshahuja@gmail.com
Introduction: Traumatic anterior hip dislocation is less common than posterior dislocation and bilateral anterior hip dislocation is a very rare presentation. Early diagnosis and treatment are of paramount importance to prevent complications. Here, we report a case of traumatic bilateral anterior hip dislocation following a high-velocity motor vehicle accident.
Case Report: A 26-year-old man was brought to the emergency department following high-energy trauma due to a motor vehicular accident. He was in considerable pain with both hips in flexion, abduction, and external rotation. There was a restriction to the range of movement at bilateral hip joints. Clinical and radiological examination revealed bilateral anterior hip dislocation.
Conclusion: Isolated anterior, obturator type of dislocation involving both hip joints with no other associated bony injury is quite unusual. The diagnosis and treatment have to be prompt. The chances of complications are high.
Keywords: Traumatic anterior hip dislocation, bilateral anterior hip dislocation, obturator type anterior hip dislocation.
Traumatic dislocation of the hip joint represents about 5% of all dislocations [1]. Posterior dislocation of the hip is more common and accounts for around 85–90% of all hip dislocations [2]. Anterior hip dislocations account for 11% of all hip dislocations and are caused by abduction and external rotation force [3]. Hip dislocations are becoming increasingly common due to the increased number of motor vehicle accidents. The position of the femoral head in relation to the acetabular socket, the force vector at the time of impact, and anatomy determine the type of dislocation and associated fractures. The hip joint is inherently very stable and a massive bony column of the pelvis surrounds the femoral head, and high energy is usually required to produce these injuries. Hip dislocation can be classified into two major groups: anterior and posterior. Anterior dislocations are further classified by their anatomic location. Epstein and Harvey used a classification according to which it can be divided into low dislocation or obturator type and high dislocation or pubic type [4]. Obturator or inferior type is more common and contributes to 70% of all cases of anterior hip dislocation [3]. Bilateral hip dislocations are rare and account for around 1.25% of all hip dislocations [5]. Most of these cases are related to acetabular or proximal femoral fractures, consisting of complex lesions. Rarely, a pure dislocation with no associated fracture is seen. Early diagnosis of a dislocated hip and prompt reduction must be done in all hip dislocations to prevent complications like avascular necrosis [AVN] [1, 6].
A 26-year-old male patient had a road traffic accident and fell off a bridge, while he was driving his motorcycle with his hips in abduction, flexion, and external rotation and was brought to the emergency room nearly 20 h after injury with complaints of severe pain, inability to bear weight, and restriction of movements at bilateral hip joints. In the emergency room, ATLS protocol was followed. The patient was clinically and hemodynamically stable and there were no other systemic injuries on the primary survey. On detailed physical examination, both hips were in abduction, flexion, and external rotation (Fig. 1). The range of motion at both the hip joints was extremely painful and restricted. There was no neurovascular deficit and no associated injuries. Radiographic evaluation of the patient was done outside before he arrived in our hospital and a roentgenogram of the pelvis with both hips revealed a bilateral anterior hip dislocation into the obturator foramen with no associated fracture (Fig. 2).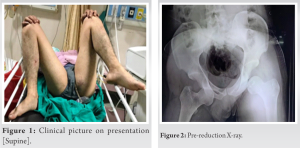
The patient was planned for immediate closed reduction and was shifted to the emergency operation theater. Under general anesthesia, dislocation of the right hip joint was reduced first in supine position using Allis’ maneuver. After stabilizing the pelvis, traction along with counter-traction was continuously applied in line with the femur, and an internal rotation and adduction force were applied to reduce the hip joint. After achieving reduction on the right side, left hip dislocation was reduced using a similar maneuver (Fig. 3). The reduction of both the hip joints was confirmed by C-arm images. Post-reduction, both hip joints were stable and neurovascular status was intact. Post-reduction, X-ray film for both the hip joints and computed tomography for the hip joints was done which revealed a concentric reduction of both the hip joints with no associated fracture or osteochondral fragments (Fig. 4, 5).
Below knee skin traction was applied bilaterally for 3 weeks. The patient was encouraged to perform static quadriceps strengthening exercises and was made to sit non-weight bearing from 4 weeks and was encouraged to do active knee range of motion exercises, quadriceps strengthening, and isometric gluteal muscle strengthening exercises. He was started on partial weight-bearing walking with a walker from 6 weeks and was gradually increased to full weight-bearing walking by 8 weeks. He returned to normal activity at 3 months. The patient was pain-free with full range of movement and no radiological signs of AVN or post-traumatic arthritis on follow-up at 21 months post-procedure (Fig. 6a, b).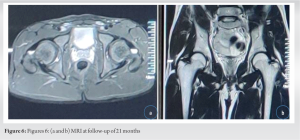
Hip dislocations occur as a result of high-energy trauma. It is seen in high-velocity motor vehicular accidents when a sudden deceleration occurs to a flexed knee and is commonly associated with fractures of the acetabulum or femoral head or neck [3]. Anterior hip dislocations are less common than posterior hip dislocations and bilateral hip dislocations are rarer. This is due to a strong anterior capsule and the Y ligament of Bigelow that prevent anterior hip dislocation [3]. A simultaneous traumatic anterior hip dislocation of the obturator type is an extremely rare injury. The greater trochanter impinges on the acetabular rim which acts as a lever and pushes the femoral head out anteriorly [7]. Epstein classified anterior hip dislocations into pelvic or superior and obturator or inferior types. This was further characterized as 2A, as there was no associated fracture [8]. A superior dislocation occurs from an abduction, external rotation, and extension moment acting on the hip. Obturator dislocation is due to flexion, abduction, and external rotation force on the hip [3].
The patient was driving his motorcycle with his hips in abduction, flexion, and external rotation and an exaggeration of the same position during trauma could cause bilateral obturator dislocation [3]. Pelvic radiographs should be performed in polytrauma patients with suspected hip dislocation. Judet views will be helpful in the identification of associated acetabular fractures [9]. Although a CT scan would better reveal associated fractures of the acetabulum and femoral head, it is not recommended as a routine pre-reduction investigation. However, a post-reduction CT scan would help in planning further course of management by visualizing intra-articular osteochondral fragments and associated acetabular fractures and also assess the quality of reduction [10]. Dudkiewicz et al. recommend a post-reduction CT to look for intra-articular fragments [11]. Prompt diagnosis and management are of paramount importance as the chance of complications significantly increases with time elapsed before the reduction of the dislocated hip. The current recommendation is to reduce the hip within 6 h from injury [2]. Hougaard and Thomsen reported that the incidence of AVN was 4.8% if the hip was reduced within 6 h and 58.8% if it was reduced after 6 h [12]. AVN was seen most commonly with posterior dislocation of the hip [7.5%] and less commonly with central dislocation [1.6%] and anterior dislocation of the hip [1.5%] [13]. The risk of AVN was 40% after surgical reduction of the hip [14]. Stewart et al. reported that it takes 17 months for osteonecrosis to be clinically detected [14]. Agarwal et al. recommend an MRI at 3 months post-reduction to look for the early changes of AVN following traumatic hip dislocations [15]. Post-traumatic arthritis, heterotopic ossification, and neurovascular injury are also reported in the literature as possible complications of hip dislocations. Post-traumatic arthritis can occur due to non-concentric reduction, osteonecrosis, associated fractures, and delay in the reduction of the hip. Sciatic nerve injury is most commonly seen with posterior hip dislocations [16]. Although rare, femoral nerve injury can occur with anterior hip dislocation [3]. Although these complications have been reported in the literature, our patient despite presenting 20 h after trauma had no complications at 21 months of follow-up and achieved a complete and painless range of movements at bilateral hip joints. However, close follow-up is essential to pick up complications and address them early.
Obturator dislocation is a rare clinical condition and bilateral obturator hip dislocation is much rarer with very few cases reported in the literature. It is commonly a result of high-velocity motor vehicular trauma and is an orthopedic emergency. Prompt diagnosis and emergent reduction are essential to prevent complications and improve the functional outcomes of patients. A close follow-up of patients is essential to identify and address complications as and when they occur.
Bilateral anterior hip dislocation is a rare clinical entity and is an orthopedic emergency. The diagnosis and treatment of bilateral anterior hip dislocation have to be quick and efficient to avoid complications.
References
- 1.Brav EA. Traumatic dislocation of the hip: Army experience and results over a twelve-year period. J Bone Joint Surg 1962;44:1115-34. [Google Scholar]
- 2.Sanders S, Tejwani N, Egol KA. Traumatic hip dislocation--a review. Bull NYU Hosp Jt Dis 2010;68:91-6. [Google Scholar]
- 3.Phillips AM, Konchwalla A. The pathologic features and mechanism of traumatic dislocation of the hip. Clin Orthop Relat Res 2000;377:7-10. [Google Scholar]
- 4.Epstein HC, Harvey JP Jr. Traumatic anterior dislocation of the hip, management and results-an analysis of fifty-five cases. J Bone Joint Surg 1972;54A:1561-2. [Google Scholar]
- 5.Shannak AO. Bilateral traumatic dislocation of the hips with ipsilateral femoral fracture. Clin Orthop Relat Res 1987;215:126-9. [Google Scholar]
- 6.Sahin V, Karakas ES, Aksu S, Atlihan D, Turk CY, Halici M. Traumatic dislocation and fracture-dislocation of the hip: A long-term follow-up study. J Trauma 2003;54:520-9. [Google Scholar]
- 7.Karaarslan AA, Acar N, Karci T, Sesli E. A bilateral traumatic hip obturator dislocation. Case Rep Orthop 2016;2016:3145343. [Google Scholar]
- 8.Epstein HC. Traumatic dislocations of the hip. Clin Orthop Relat Res 1973;92:116-42. [Google Scholar]
- 9.Kool DR, Blickman JG. Advanced trauma life support®. ABCDE from a radiological point of view. Emerg Radiol 2007;14:135-41. [Google Scholar]
- 10.Brooks RA, Ribbans WJ. Diagnosis and imaging studies of traumatic hip dislocations in the adult. Clin Orthop Relat Res 2000;377:15-23. [Google Scholar]
- 11.Dudkiewicz I, Salai M, Horowitz S, Chechik A. Bilateral asymmetric traumatic dislocation of the hip joints. J Trauma 2000;49:336-8. [Google Scholar]
- 12.Hougaard K, Thomsen PB. Coxarthrosis following traumatic posterior dislocation of the hip. J Bone Joint Surg Am 1987;69:679-83. [Google Scholar]
- 13.Letournel E, Judet R. Surgical anatomy. In: Letournel E, Judet R, Elson RA, editors. Fractures of the Acetabulum. Berlin, Heidelberg: Springer; 1981. p. 1-6. [Google Scholar]
- 14.Stewart MJ, Milford LW. Fracture-dislocation of the hip: An end-result study. J Bone Joint Surg Am 1954;36:315-42. [Google Scholar]
- 15.Agarwal S, Singh GK, Jain UK, Jyoti G. Simultaneous anterior and posterior traumatic dislocation of the hip. A case report with review of the literature. Arch Orthop Trauma Surg 2000;120:236-8. [Google Scholar]
- 16.Alshammari A, Alanazi B, Almogbil I, Alfayez SM. Asymmetric bilateral traumatic hip dislocation: A case report. Ann Med Surg (Lond) 2018;32:18-21. [Google Scholar]









