Avoid pestering the ulnar nerve.
Dr. Sandeep Boddeda, Department of Orthopaedic Surgery, Sunshine Bone and Joint Institute, Secunderabad, Telangana, India. E-mail: sandeep.boddeda@gmail.com
Introduction: Distal humerus fractures constitute around 0.2 to 7% of all fractures, 30% of all umerus fractures, most common in young adults, are due to high energy trauma and in old age due to osteoporosis. A common step in all currently available approaches is to identify the ulnar nerve, expose, mobilise, and retract this from its surrounding bed or in situ release. Ulnar neuropathy is either observed immediately after surgery or delayed up to one year after surgery. We are describing a new posterior approach for intra-articular distal humerus fractures, where identification and retraction of the ulnar nerve are not required to fix the intra-articular fractures of the distal humerus, thereby avoiding injury to the ulnar nerve.
Material and Methods: Seven patients with AO type B and C were treated using our new ulnar nerve-sparing approach between January 2017 and December 2019. Postoperatively, all the patients have been examined for ulnar neuropathy symptoms.
Results: We have no ulnar nerve neuropathy either in the post-operative period or at 2 years follow-up (five cases were followed up for 2 years and two patients lost to follow-up after 6 months). At the end of 2 years, the mean range of motion achieved at elbow was 134°. The mean oxford elbow score was 45.2 (42–47). Heterotopic ossification and infection were not found in our cases.
Conclusion: Our ulnar nerve-sparing approach for intra-articular fractures of distal third humerus by posterior approach helps in fixing articular fractures of distal humerus without exposing ulnar nerve during surgery without compromising on the exposure of fracture for fixation, thus reducing the chances of ulnar nerve injury and post-operative neuropathy.
Keywords: A new technique, distal humerus intra-articular fractures, avoid ulnar neuropathy, surgical approach to elbow, posterior surgical to elbow, elbow fractures, ORIF elbow fractures, latest posterior approaches to the elbow
Distal humerus fractures constitute around 0.2% to 7% of all fractures, 30% of all humerus fractures, most common in young adults is due to high-energy trauma and in old age due to osteoporosis [1]. Commonly used surgical approaches are Campbells [2], Alonso-Lhames [3] Paratricipetal, and Olecranon osteotomy [4]. Triceps flexor carpi ulnaris approach (TRIFCU) [5] and the Triceps peel approach, a modification of TRIFCU [6], are other approaches used to fix these fractures. A common step in all the above approaches is to identify the ulnar nerve, expose, mobilise, and retract this from its surrounding bed. These approaches are associated with high incidence of ulnar nerve injury leading to post-operative ulnar nerve neuropathy [7, 8, 9, 10]. Ulnar neuropathy is either observed immediately after surgery or delayed up to 1 year after surgery. During surgical fixation of distal humerus, Shearin et al. [11] reported an overall ulnar neuropathy incidence of 19.3%. Of those patients undergoing in situ release, the incidence was 15.3% and of those who underwent transposition, there was a 23.5% incidence of ulnar neuropathy. We are describing a new posterior approach for intra-articular distal humerus fractures, where identification and retraction of the ulnar nerve are not required to fix the intra-articular fractures of the distal humerus, thereby avoiding injury to the ulnar nerve. Surgical Technique Position Lateral decubitus position operative side limb facing up, elbow flexed to 90° over the sandbag. Bony landmarks Medial epicondyle, Olecranon Tip, and Lateral epicondyle. Skin incision Midline incision starting 7 cm proximal to the olecranon and extending 6 cm distal to the olecranon with a medial curve over the tip of the olecranon, curving laterally over the ulna. Superficial dissection Superficial dissection is carried out medial to the medial epicondyle and lateral to the lateral epicondyle on the medial and lateral sides. Skin, subcutaneous tissue, and superficial fascia are cut in the same line of skin incision. Superficial dissection is continued between the superficial fascia and the deep fascia of the triceps muscle. Lateral superficial dissection Superficial dissection on the lateral side extends up the posterior surface of the lateral epicondyle for posterior plating and can be carried over the lateral and superior surface distal humerus for lateral anatomical plate positioning.
Medial superficial dissection
Medial superficial dissection is done up to the medial and anterior to the medial epicondyle. Care is taken not to cut or perforate the brachial fascia over the medial head of the triceps.
Deep surgical dissection on the lateral side
Deep dissection on the lateral side is the same as described in standard approaches and must be restricted proximally up to 10cm from the lateral epicondyle.
Deep dissection on the medial side
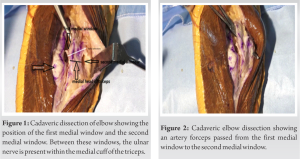
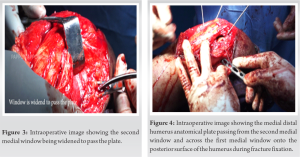
This consists of creating two windows for fracture exposure and fixation after identifying the medial epicondyle, olecranon tip, and medial epicondyle. The Medial First window is in the midline (Fig. 1) along the medial border of the triceps tendon, olecranon, and medial border of the proximal ulna. The triceps tendon is divided, leaving a 2–3 mm wide tendon sheath attached to the medial head of the triceps, along the medial border of the olecranon continued 4 cm distally along the medial border of the proximal ulna, medial head of the triceps is separated subperiosteally dissecting the medial head of flexor carpi ulnaris and flexor digitorum superficialis attachments. The medial head of the triceps is retracted medially to do a medial arthrotomy on the medial side. Then, the medial expansion of the first window is done subperiosteally along the medial surface of the cubital tunnel (extra-articular portion of the medial surface of trochlea), posterior surface of medial humeral condyle up to the supracondylar ridge, and dissection is carried by elevating medial triceps from the medial intermu scular septum and posterior surface of the medial distal humerus up to medial epicondyle. Brachialis fascia presents over the medial triceps and the intermuscular septum must be left intact. A Medial Second Window (Fig. 1) is now created on the medial side between the medial head of the triceps and the medial intermuscular septum. Initially, the medial epicondyle is palpated and identified, the triceps muscle is elevated from the posterior surface of the medial intermuscular septum 4 cm proximal to the medial epicondyle, and a periosteal elevator is passed to free the remaining soft tissues from the medial supracondylar ridge; then, a blunt artery forceps is passed along the supracondylar ridge and the superior surface of the medial epicondyle piercing the fascia superior to the medial epicondyle by a blunt method. Communicating the second medial window and posterior humerus from the medial side (Fig. 2), Struthers ligament needs to be cleared from the superior portion of the medial epicondyle for the plate to sit properly on the medial supracondylar ridge and medial epicondyle. The second medial window is widened by 3–4 cm to pass the plate (Fig. 3). This will allow medial distal humerus anatomical plates to slide through the second medial window to the first medial window (Fig. 4). Olecranon osteotomy can be added if the reduction is difficult due to severe comminution of the fracture fragments. We have also studied this on the cadaver (Fig. 1). A case from our series is shown in Fig. 5. Extension: Proximal extension of the first medial window along the triceps can be done up to the proximal humerus to fix associated shaft fractures or to include the proximal extension of the distal humerus fracture. Distal extension of the approach can be made along the medial border of ulna to fix ulna shaft fractures and along the lateral border of the ulna to fix radial head fractures.
Between January 2017 and December 2019, seven patients (males – 5 and females – 2) aged between 22 and 62 years with AO type B and C closed intra-articular fracture of the distal humerus were managed using our new technique without exposing ulnar nerve by posterior approach. Fractures were fixed as per AO principles. Postoperatively, all the patients have been examined for ulnar neuropathy symptoms. All patients were followed up for 2 years (range, 2–4 years).
Two cases were lost to follow-up after 6 months, five had follow-up of 2 years. All patients at 2-year follow-up were examined clinically for ulnar neuropathy. Functional outcome was measured using the oxford elbow score, range of motion, and complications were noted.
We have no ulnar nerve neuropathy either in the early post-operative period or at 2 years (5 cases were followed up for 2 years and 2 patients lost to follow-up after 6 months). Union achieved by the end of 6 months with a mean duration of 22 weeks. At the end of 2 years, 134° mean flexion was achieved with a mean extension lag of 6°. The mean Oxford elbow score was 45.2 (42–47). Heterotopic ossification (HO) and infection was not found in any of our cases.
Incidence of post-ORIF ulnar nerve neuropathy is reported by various authors ranging between 0% and 38% [13]. Holdsworth and Mossad [14] reported 51% incidence. Ulnar nerve exploration, mobilization, and in situ release without mobilzation and anterior transposition are the established causes of post-operative ulnar nerve neuropathy [8, 9, 10, 11]. Ulnar nerve contusion, laceration by sharp bony fragments, and hematoma are the causes due to injury. Iatrogenic causes of ulnar nerve injury include exposure and mobilization from its bed, anterior transposition [11] excessive retraction or inadvertent injury during surgical exposure, fracture manipulation, or implant irritation [12]. Post-operative swelling and hematoma formation contribute to compression of the ulnar nerve. Delayed causes of ulnar neuropathy can be related to soft tissue scarring, HO, and prominent hardware. Unfortunately, no surgical technique has been described standardizing the surgical handling of the ulnar nerve to prevent ulnar nerve neuropathy. In our new technique, adequate exposure of the distal humerus intra-articular region is achieved without the need for exposure of the ulnar nerve, significantly decreasing the chances of iatrogenic ulnar nerve injury. In this approach, the muscular coverage of the ulnar nerve over a length of 8 to 9 cm from cubital fossa to Struthers ligament is preserved. The muscular cuff around the ulnar nerve, which is left intact, prevents devascularization and hardware-related injury to the ulnar nerve. None of our cases had immediate post-operative or delayed ulnar nerve injury at a minimum follow-up of 2 years.
Limitations
Our study is on a small group of patients. Further, multicenter randomized control studies with larger sample size are required to substantiate our findings.
Our new technique does not need the exposure of the ulnar nerve during exposure for intra-articular fractures of the distal humerus by posterior approach. This helps in minimizing injury to theulnar nerve during surgery without compromising on the exposure of the fracture for fixation.
Three window posterior ulnar nerve sparring approach described by us is unique in a way that the ulnar nerve need not be exposed; rather, the medial first window can be used to expose the humeral shaft proximally up to proximal humerus by creating a plane between medial head distally, long head of triceps medially, and lateral head of triceps muscles laterally thereby sparing innervation of the radial nerve to the whole of triceps. The medial second window also goes through the inter nervous plane and can be extended proximally up to 5 cm and not beyond that to prevent damage to the blood supply of ulnar nerve. These windows allow the surgeon to attain reduction, fix fracture, preserve vascularity of ulnar nerve, preserve innervation of the triceps muscle, protect the ulnar nerve from direct handling by the surgeon, and implant irritation. Olecranon osteotomy can always be added in severely comminuted fractures to get a perfect reduction.
References
- 1.Amir S, Jannis S, Daniel R. Distal humerus fractures: A review of current therapy concepts. Curr Rev Musculoskelet Med 2016;9:199-206. [Google Scholar]
- 2.Campbell WC. Incision for exposure of the elbow joint. Am J Surg 1932;15:65-7. [Google Scholar]
- 3.Alonso-Llames M. Bilaterotricipital approach to the elbow. Its application in the osteosynthesis of supracondylar fractures of the humerus in children. Acta Orthop Scand 1972;43:479-90. [Google Scholar]
- 4.MacAusland WR. Ankylosis of the elbow: With report of four cases treated by arthroplasty. JAMA 1915;LXIV:312-8. [Google Scholar]
- 5.Deakin DE, Deshmukh SC. The triceps-flexor carpi ulnaris (TRIFCU) approach to the elbow. Ann R Coll Surg Engl 2010;92:240-2. [Google Scholar]
- 6.Grogan BF, Blair JA, Blease RE, Cho MS, Hsu JR. Exposure of the distal humerus using a triceps hemi-peel approach. Orthopedics 2014;37:e455-9. [Google Scholar]
- 7.Korner J, Lill H, Müller LP, Hessmann M, Kopf K, Goldhahn J, et al. Distal humerus fractures in elderly patients: Results after open reduction and internal fixation. Osteoporos Int 2005;16:S73-9. [Google Scholar]
- 8.Chen RC, Harris DJ, Leduc S, Borrelli JJ Jr., Tornetta P 3rd., Ricci WM. Is ulnar nerve transposition beneficial during open reduction internal fixation of distal humerus fractures? J Orthop Trauma 2010;24:391-4. [Google Scholar]
- 9.Ruan HJ, Liu JJ, Fan CY, Jiang J, Zeng BF. Incidence, management, and prognosis of early ulnar nerve dysfunction in Type C fractures of the distal humerus. J Trauma 2009;67:1397-401. [Google Scholar]
- 10.Shin R, Ring D. The ulnar nerve in elbow trauma. J Bone Joint Surg Am 2007;89:1108-16. [Google Scholar]
- 11.Shearin JW, Chapman TR, Miller A, Ilyas AM. Ulnar nerve management with distal humerus fracture fixation: A meta-analysis. Hand Clin 2018;34:97-103. [Google Scholar]
- 12.Ahmed AF, Parambathkandi AM, Kong WJ, Salameh M, Mudawi A, Ahmed GO, et al. The role of ulnar nerve subcutaneous anterior transposition during open reduction and internal fixation of distal humerus fractures: A retrospective cohort study. Int Orthop 2020;44:2701-8. [Google Scholar]
- 13.Vazquez O, Rutgers M, Ring DC, Walsh M, Egol KA. Fate of the ulnar nerve after operative fixation of distal humerus fractures. J Orthop Trauma 2010;24:395-9. [Google Scholar]
- 14.Holdsworth BJ, Mossad MM. Fractures of the adult distal humerus. Elbow function after internal fixation. J Bone Joint Surg Br 1990;72:362-5. [Google Scholar]