In patients with posterolateral pain and discomfort or catching of the elbow, posterior arthroscopic confirmation of the intra-articular structure is recommended after debridement of the ECRB tendon.
Dr. Taku Suzuki, Department of Orthopaedic Surgery, Keio University School of Medicine, Shinjuku, Tokyo 160-8582, Japan. E-mail: sutaku49@gmail.com
Introduction: Posterior radiocapitellar synovial plica excision is sometimes performed for lateral epicondylitis after debridement of the extensor carpi radialis brevis (ECRB) tendon. We describe a rare intra-articular abnormality of the posterior radiocapitellar joint diagnosed on posterior arthroscopic observation.
Case Report: A 48-year-old man presented with posterolateral pain and discomfort in his left elbow. A diagnosis of lateral epicondylitis was made, and arthroscopic debridement of the ECRB tendon was performed. Posterior arthroscopic examination revealed a tendon-like abnormality running longitudinally along the articular surface of the capitulum of the humerus. The abnormality was resected using a shaver, and symptoms improved postoperatively.
Conclusion: In patients with posterolateral pain and discomfort or catching of the elbow, posterior arthroscopic confirmation of the intra-articular structure is recommended after debridement of the ECRB tendon.
Keywords: Abnormality, intra-articular abnormality, lateral epicondylitis, synovial plica, tennis elbow
Lateral epicondylitis is a common elbow disorder characterized by microtears within the extensor carpi radialis brevis (ECRB) tendon, resulting in chronic pain in the lateral elbow [1]. Arthroscopic debridement of the ECRB tendon and synovial fold through an anterior portal is a reliable technique for pain improvement (Baker’s technique) [2]. Posterior radiocapitellar synovial plica excision is sometimes performed after Baker’s technique [3]. In this case report, we describe a rare intra-articular abnormality of the posterior radiocapitellar joint diagnosed on posterior arthroscopic observation.
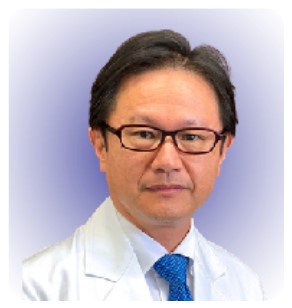
A 48-year-old man presented with lateral pain in his left elbow. A diagnosis of lateral epicondylitis was made and the patient was initially treated conservatively with physiotherapy, elbow straps, and corticosteroid injections at another institution. However, the pain did not improve and the patient was referred to our hospital. Physical examination revealed tenderness over the lateral epicondyle of the humerus and pain induced by resistance to the middle finger or on wrist extension. He also experienced discomfort and catching around the posterior radiocapitellar joints during extension and flexion of the elbow. Although there were no restriction of range of motion of the elbow, the patient’s grip strength had decreased to 45 kg on the left side compared with 52 kg on the right side. A radiograph of the elbow showed no abnormal findings. Magnetic resonance imaging (MRI) showed increased effusion in the humeroradial joint, but there was no marked signal change at the origin of the ECRB tendon (Fig. 1). No obvious intra-articular abnormal tissue, except for posterior synovial plicas, was identified on pre-operative MRI. Arthroscopic surgery was planned for debridement of the ECRB tendon and to examine the cause of posterolateral discomfort and catching in the elbow. Intra-articular observation of the radiocapitellar joint was performed through the anteromedial portal. Degenerative changes in the lateral capsule with synovitis were observed, but there was no synovial plica interposed in the humeroradial joint (Fig. 2a).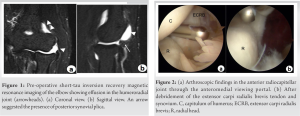
We identified a tendon-like tissue running longitudinally along the articular surface of the capitulum of the humerus, which is a rare intra-articular abnormality in the posterior radiocapitellar joint, through posterior arthroscopic observation. Various intra-articular soft-tissue abnormalities of the radiocapitellar joint have been reported in clinical and cadaveric studies [4, 5, 6]. These abnormalities include synovial plicas, folds, masses, cords, bands, and fringes; menisci; meniscoids; and meniscocapsular complexes. The most common abnormalities are synovial plicas or synovial folds. Synovial plicas are embryological remnants of the synovial septum, and in the radiocapitellar joint, the synovial plica may be located anterolateral, posterolateral, or lateral to the olecranon [7]. The frequency of synovial plica in the posterolateral region ranges from 86% to 100% [8, 9, 10]. Mullett arthroscopically evaluated radiocapitellar joints in cadaveric elbows through anterior viewing and classified synovial folds into four types: Type 1 (56%): The radial head is completely exposed; Type 2 (21%): The radial head is partially covered by a loose fold that is not interposed in the humeroradial joint during flexion and extension; Type 3 (15%): The radial head is obscured by the humeroradial capsular complex, which becomes interposed in the humeroradial joint during flexion and extension; and Type 4 (9%): there is a fully developed thickened band that completely obscures the radial head [11]. Unlike anterior synovial folds, which have been arthroscopically classified, posterior synovial folds or other abnormalities have not been classified. Most posterior intra-articular abnormalities are interposed in the radiocapitellar joint, leading to catching or locking of the elbow [4, 5, 6]. To the best of our knowledge, tendon-like intra-articular abnormalities similar to that in this case have not been reported in clinical or cadaveric studies. Although the structure in this case was not interposed in the humeroradial joint, we hypothesized that tissue mobility along the articular surface during elbow motion might have led to the patient’s symptoms. Based on the easy resection of the tissue with a shaver, we suspect that this soft tissue may be of synovial origin. However, no histopathological examination of this tissue was performed, and the accurate diagnosis of the abnormality in this case was unclear. Arthroscopic debridement of the origin of the ECRB tendon through an anterior portal is a reliable technique for lateral epicondylitis [2]. However, the necessity of posterior synovial fold excision remains controversial [3]. Rhyou and Kim reported that additional debridement of posterior synovial folds did not enhance pain relief or function [3]. In patients with pain at the lateral epicondyle and posterolateral discomfort or catching in the elbow, as in this case, arthroscopic evaluation of the posterior articular structure is recommended after debridement of the ECRB tendon.
We described a rare abnormality in the posterior radiocapitellar joint in patients with lateral epicondylitis. Debridement of the ECRB tendon and posterior abnormality provided satisfactory results.
In patients with lateral epicondylitis with posterolateral discomfort or catching of the elbow, arthroscopic confirmation of the intra-articular structure through the posterior viewing portal is recommended after debridement of the ECRB tendon.
References
- 1.Ahmad Z, Siddiqui N, Malik SS, Abdus-Samee M, Tytherleigh-Strong G, Rushton N. Lateral epicondylitis: A review of pathology and management. Bone Joint J 2013;95-B:1158-64. [Google Scholar]
- 2.Baker CL, Jones GL. Arthroscopic management of miscellaneous elbow disorders. Oper Tech Sports Med 1998;6:16-21. [Google Scholar]
- 3.Rhyou IH, Kim KW. Is posterior synovial plica excision necessary for refractory lateral epicondylitis of the elbow? Clin Orthop Relat Res 2013;471:284-90. [Google Scholar]
- 4.Jeon IH, Liu H, Nanda A, Kim H, Kim DM, Park D, et al. Systematic review of the surgical outcomes of elbow plicae. Orthop J Sports Med 2020;8:2325967120955162. [Google Scholar]
- 5.Lubiatowski P, Wałecka J, Dzianach M, Stefaniak J, Romanowski L. Synovial plica of the elbow and its clinical relevance. EFORT Open Rev 2020;5:549-57. [Google Scholar]
- 6.Kholinne E, Nanda A, Liu H, Kwak JM, Kim H, Koh KH, et al. The elbow plica: A systematic review of terminology and characteristics. J Shoulder Elbow Surg 2021;30:e185-98. [Google Scholar]
- 7.Cerezal L, Rodriguez-Sammartino M, Canga A, Capiel C, Arnaiz J, Cruz A, et al. Elbow synovial fold syndrome. AJR Am J Roentgenol 2013;201:W88-96. [Google Scholar]
- 8.Koh S, Morris RP, Andersen CL, Jones EA, Viegas SF. Ultrasonographic examination of the synovial fold of the radiohumeral joint. J Shoulder Elbow Surg 2007;16:609-15. [Google Scholar]
- 9.Isogai S, Murakami G, Wada T, Ishii S. Which morphologies of synovial folds result from degeneration and/or aging of the radiohumeral joint: An anatomic study with cadavers and embryos. J Shoulder Elbow Surg 2001;10:169-81. [Google Scholar]
- 10.Duparc F, Putz R, Michot C, Muller JM, Fréger P. The synovial fold of the humeroradial joint: Anatomical and histological features, and clinical relevance in lateral epicondylalgia of the elbow. Surg Radiol Anat 2002;24:302-7. [Google Scholar]
- 11.Mullett H, Sprague M, Brown G, Hausman M. Arthroscopic treatment of lateral epicondylitis: Clinical and cadaveric studies. Clin Orthop Relat Res 2005;439:123-8. [Google Scholar]