Metacarpophalangeal (MCP) joint dislocation is rare entity in paediatric age. Attempts for close reduction to be done cautiously. knowledge of proper surgical approach is essential for early and good functional recovery.
Dr. Shubham Srivastava, Clinical Fellow, Department of Paediatric Orthopaedics, King George’s Medical University, Lucknow, Uttar Pradesh, India. E-mail: drshubhamortho@gmail.com
Introduction: Metacarpophalangeal (MCP) joint dislocation is a rare occurrence in the pediatric population. A few case reports are available globally. Understanding of anatomy of the MCP joint is necessary for the surgical approach. We report a case of complex volar MCP joint dislocation in a pediatric patient.
Case Report: We report a 13-year-old male child with traumatic dislocation of the MCP joint of the index finger. It was a complex volar dislocation that was surgically treated via a dorsal approach. On 6-month follow-up, child regained an almost normal range of motion at the MCP joint with a good functional outcome.
Conclusion: Complex MCP joint dislocation often needs open reduction. Out of the two described surgical approaches, we preferred the dorsal approach which allowed proper visualization of the volar plate and avoided risks to neurovascular bundles. Early management and early mobilization provide good functional outcomes.
Keywords: Metacarpophalangeal joint dislocation, complex dislocation, Kaplan approach, farabeuf.
Metacarpophalangeal joint (MCP) dislocation is a rare entity in pediatric age group. The most common mode of injury is forced hyperextension and fall on out stretch hand [1]. MCP joint has strong ligamentous complex support as compared to the thumb. A thick and strong volar plate and attached flexor tendon sheath keep the joint in a protected position [2]. Dislocations of MCP joints can be classified as simple and complex. Simple dislocations are more frequent and they can be reduced with closed methods. The association of fracture or soft-tissue interposition makes it difficult to reduce which classifies it into complex dislocations. Based on displacement, two types of dislocations are described dorsal and volar [3]. In dorsal dislocation, proximal phalanx is displaced dorsally relative to the metacarpal. Volar dislocations are difficult to reduce because of entrapment of the volar plate or associated fracture. Complex dislocation will need open reduction of the MCP joint. Two different surgical approaches are described the volar and dorsal approaches. The dorsal approach has the advantage of minimal risk to neurovascular bundles compared to the volar approach. Repair of osteochondral defects can be done by dorsal approach. While proponents of the volar approach advocate that this approach provides better viewing of joint and if needed repair of the volar plate can be done simultaneously [3].
We report a case of complex MCP joint dislocation of the right index finger in a 13-year-old male child. The patient sustained trauma 5 days before admission as a result of a fall on an outstretched hand while playing outdoors. On examination, the swelling was present over the right index finger with an inability to movements. Neurovascular status was intact and pinprick was present. An X-ray of hand was obtained and the diagnosis was confirmed (Fig. 1). Immediately after trauma patient was taken to the hospital where two attempts of close reduction were taken by the referring physician. The close reduction trial went unsuccessful and the patient was referred to us for further management. The patient was taken under general anesthesia. Under fluoroscopic guidance, one attempt was taken for a close reduction but it could not be achieved. We used a dorsal approach for the MCP joint (Fig. 2).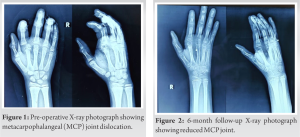 A 3 cm dorsal curvilinear incision was taken over the MCP joint with a curve toward the radial side [4]. After splitting the extensor mechanism, the neurovascular bundle was identified and saved. The joint capsule was split longitudinally. The head of the second metacarpal was found to be dislocated in the volar side. There was a buttonhole through the volar plate. Elevator was put beneath the metacarpal head. With longitudinal traction and slight flexi on, the dislocation was reduced. There was no osteochondral fragment or part entrapment seen. A fluoroscopic examination was done. Pre-operative range of movement was assessed. The reduction was found to be stable and satisfactory. The joint capsule, extensor mechanism, and skin were closed with appropriate sutures. Post-operative plaster of Paris (POP) volar slab was given for 3 weeks. After the removal of the slab, gentle range of motion physiotherapy was started. By the end of 6 weeks, the patient has regained almost normal range of motion of the MCP joint. Follow-up X-rays confirmed proper and stable reduction (Fig. 3 & 4). The pre-operative X-ray revealed dorsal dislocation of the MCP joint but while performing open reduction, the metacarpal head was found to be displaced toward the volar side. This might be due to the failed close reduction trials, during which excessive hyperextension at the MCP joint could have displaced it toward the volar side.
A 3 cm dorsal curvilinear incision was taken over the MCP joint with a curve toward the radial side [4]. After splitting the extensor mechanism, the neurovascular bundle was identified and saved. The joint capsule was split longitudinally. The head of the second metacarpal was found to be dislocated in the volar side. There was a buttonhole through the volar plate. Elevator was put beneath the metacarpal head. With longitudinal traction and slight flexi on, the dislocation was reduced. There was no osteochondral fragment or part entrapment seen. A fluoroscopic examination was done. Pre-operative range of movement was assessed. The reduction was found to be stable and satisfactory. The joint capsule, extensor mechanism, and skin were closed with appropriate sutures. Post-operative plaster of Paris (POP) volar slab was given for 3 weeks. After the removal of the slab, gentle range of motion physiotherapy was started. By the end of 6 weeks, the patient has regained almost normal range of motion of the MCP joint. Follow-up X-rays confirmed proper and stable reduction (Fig. 3 & 4). The pre-operative X-ray revealed dorsal dislocation of the MCP joint but while performing open reduction, the metacarpal head was found to be displaced toward the volar side. This might be due to the failed close reduction trials, during which excessive hyperextension at the MCP joint could have displaced it toward the volar side.
MCP joint has a design of synovial condyloid joint. MCP joint is formed by the convex metacarpal head and corresponding concave base of the proximal phalanges. The primary movements of the MCP joints are flexion, extension, abduction, adduction, and circumduction. These movements are facilitated by a joint capsule, ligaments, and associated musculotendinous tissues. The collateral ligaments are the main stabilizers of the MCP joint and they are present over both radial and ulnar borders. There is a fibrocartilaginous structure located at the palmer aspect of the MCP joint, also called volar plate [5]. Rupture of this volar plate entraps dislocated metacarpal head due to which difficulty in reduction occurs and it is called complex volar dislocation [3]. The clinical examination helps in diagnosing the type of dislocation. Swelling will be present over the MCP joint along with restriction of movements. Puckering over the skin is a sign of complex dislocation [5]. Hyperextension at the MCP joint will be exaggerated in simple dislocations as compared to complex dislocations. Closed reduction can be done in simple dislocations. The reduction should be attempted under the wrist, with metacarpal block, or under general anesthesia. The close reduction maneuver consists of flexing the wrist joint followed by applying pressure with the thumb over the metacarpal head. Care has to be taken so as not to hyperextend the joint. As hyperextension may lead to the conversion of simple dislocations into complex type [5]. The surgical reduction techniques are described by Kaplan [6] and Farabeuf [7]. Kaplan described the volar approach for the MCP joint while farabeuf advocated for the dorsal approach. The volar approach has the advantage of direct access to the surgical field. Furthermore, this approach is better for the release of volar entrapment of the MCP joint. The risk of neurovascular bundle injury is higher as compared to the dorsal approach. Kodama [8] has described an arthroscopic reduction technique for complex dorsal MCP dislocations. Another percutaneous reduction technique through the dorsal approach is described by Sodha et al. [9] This technique was done under regional anesthesia in the emergency room. Following surgical reduction, the joint is immobilized with splints for 3 weeks. Although the early range of motion exercises is to be encouraged after removal of the splint, because a longer duration of splinting will lead to a loss in regaining range of motion [10]. Complications associated with dorsal MCP joint dislocations are due to delayed presentation, associated fractures, and prolonged immobilization. Prolong immobilization increases the risk of stiffness. Repeated attempts at close reduction should be avoided [2]. Early degenerative arthritis may be seen in adult patients. As the metacarpal head is intracapsular, any injury to the MCP joint may result in disruption of vascular supply to the epiphysis. Growth arrest is a unique complication that occurs in the pediatric population due to damage to vascularity [1].
Complex MCP joint injury is uncommon in pediatric age. Prompt clinical and radiographic examination is warranted. Complex dislocations are unamenable to close reduction; hence, open reduction is often required. The dorsal approach provides better exposure and risk to the neurovascular structure is minimized. Early intervention provides good results in terms of regaining range of motion and prevents secondary complications.
MCP joint dislocation in pediatric age is rarely seen and reported. Simple dislocations are amenable for close reductions while complex ones will need open surgical reduction. Choosing surgical approach depends on type of dislocation and surgeon’s experience. Early diagnosis and timely management provide good functional outcomes.
References
- 1.Sumarriva G, Cook B, Godoy G, Waldron S. Pediatric complex metacarpophalangeal joint dislocation of the index finger. Ochsner J 2018;18:398-401. [Google Scholar]
- 2.Rubin G, Orbach H, Rinott M, Rozen N. Complex dorsal metacarpophalangeal dislocation: Long-term followup. J Hand Surg Am 2016;41:e229-33. [Google Scholar]
- 3.Barry K, McGee H, Curtin J. Complex dislocation of the metacarpo-phalangeal joint of the index finger: A comparison of the surgical approaches. J Hand Surg Br 1988;13:466-8. [Google Scholar]
- 4.Türker T, Sheppard JE. Emergency open reduction for an irreducible dislocation of the metacarpophalangeal joint of the thumb in a child. J Hand Microsurg 2015;7:166-9. [Google Scholar]
- 5.McDevitt ER, Roberts WO. Dorsal dislocations of the MCP joint. Physician Sports Med 1999;27:75-6. [Google Scholar]
- 6.Kaplan EB. Dorsal dislocation of the metacarpophalangeal joint of the index finger. J Bone Joint Surg Am 1957;39-A:1081-6. [Google Scholar]
- 7.Farabeuf LH. De la luxation du ponce en arrière. Bull Soc Chir 1876;11:21-62. [Google Scholar]
- 8.Kodama A, Iotani Y, Mizuseki T. Arthroscopic reduction of complex metacarpophalangeal dislocation of index finger. Arthrosc Tech 2014;3:e261-4. [Google Scholar]
- 9.Sodha S, Breslow GD, Chang B. Percutaneous technique for reduction of complex metacarpophalangeal dislocations. Ann Plast Surg 2004;52:562-5; discussion 566. [Google Scholar]
- 10.McLaughlin HL. Complex “locked” dislocation of the metacarpophalangeal joints. J Trauma 1965;5:683-8. [Google Scholar]







