Eosinophilic granuloma affecting the vertebral body of the subaxial spine is a rare benign condition affecting the children. It requires a thorough radiological and histopathological work for confirmation of diagnosis.
Dr. Mantu Jain, Department of Orthopedics, All India Institute of Medical Sciences, 102/J, Cosmopolis, Dumduma, Bhubaneswar, Odisha, India. E-mail: montu_jn@yahoo.com
Introduction:Eosinophilic granuloma (EG) is a type of Langerhan cell histiocytosis (LCH) with unknown etiology. This benign tumorous lytic lesion affects mainly children or young adults, causing bone destruction. Although, the flat or the long bones are commonly affected, localized spinal involvement in pediatric age group is rare. A thorough workup is therefore necessary for this condition, which may mimic other severe conditions.
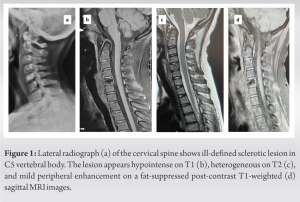
Case Report:A 10-year-old girl presented with neck pain for 4 months without any history of trauma, fever, or neurological weakness. An X-ray revealed radiolucency and sclerosis of the fifth cervical vertebral body, which was hypointense on T1 and heterogeneous on T2-weighted image, with mild peripheral enhancement on fat-suppressed post-contrast T1-weighted image. Biopsy histomorphology revealed a lymphohistiocytic lesion with scatted histiocytes with grooved nuclei, immunopositive for Langerin; thus consistent with LCH (EG). She was managed conservatively with a completely pain free course with full range of movement at 1-year follow-up. Her follow-up X-ray showed complete remodeling and ongoing fusion.
Conclusion:EG should be considered as a differential diagnosis in the evaluation of solitary lytic lesion involving spine in pediatric age group. This, although self-resolving, may occasionally need surgical intervention with or without adjuvant therapy.
Keywords:Eosinophilic granuloma, cervical spine, vertebral body.
Eosinophilic granuloma (EG) is the most common element in the spectrum of Langerhan cell histiocytosis (LCH) that also includes Hand-Schuller-Christian disease, and Letterer-Siwe disease [1]. This usually affects the flat and long bones in children but rarely involves the spine [2]. Due to the rarity, the non-specific lytic imaging of EG may mimic other pure lytic lesions secondary to infection and tumors, requiring further investigations for confirmation [1, 3]. We aim to describe a case of EG in a young child involving the cervical spine with clinicopathological, radiological, and follow-up data.
A 10-year-old girl presented with a 4-month history of neck pain which was dull, aching, constantly extending from mid-portion to occipital region without any features suggestive of radiculopathy, and increased with extremes of flexion and rotation. There was no history of trauma, fever, or neck rigidity. Although there was no associated neurological weakness, we could elicit local tenderness on the rotation of the spinous process. The neck pain was relieved with support like a collar. A plain radiograph revealed a suspicious radiolucent lesion with sclerosis involving the fifth cervical (C5) vertebral body (Fig. 1a). Magnetic resonance imaging (MRI) showed a T1W hypointense and T2W heterogeneous lesion in C5 vertebral body with mild peripheral enhancement on contrast-enhanced T1-fat suppressed sagittal (Fig. 1b-d). There were no associated soft-tissue shadows. Her routine blood investigations for infection screening were within normal limits (total leukocyte count: 7,000 cells/mm3, erythrocyte sedimentation rate: 10 mm/first hour, and C-reactive protein: 0.6 mg/dL). A complete skeletal survey and an abdomen ultrasound were also negative for any multifocal lesion. Considering the anterior positioning of the spinal lesion, a mini-open biopsy was planned.
An inch oblique incision was placed over the C5 vertebra, and a true cut biopsy was obtained using Jamshidi needle (mention size) under fluoroscopic guidance. The tissue was sent for microbial culture and histopathological examination (HPE). Cultures for pyogenic organisms, tuberculosis and fungi showed no growth. HPE showed a benign fibro-osseous lesion comprising of lymphomononuclear inflammatory cell collections admixed with scattered histiocytic cells with grooved and folded nuclei (Fig. 2a). On immunohistochemistry (IHC), the histiocytes with grooved nuclei showed weak staining, thus confirming the Langerhan cells. Histomorphology, in correlation with IHC, were in favor of LCH (EG) (Fig. 2b). The patient was reassured, sent home with an advice to wear a soft collar, and prescribed analgesics for 3 weeks. There was no restriction of activities thereafter. At 1-year follow-up, she was pain-free with a full range of movement (Fig. 3 a and b). The X-ray showed a partial collapse with complete remodeling and ongoing fusion (Fig. 3c and d). No further MRI was done in as patient was asymptomatic and X-ray showed sclerosis of vertebral body with ongoing fusion. (why not? You should comment the reason.)
Even though EG accounts for 1% of bony tumors, 80% of the affected patient are <10 years [2, 4]. The subaxial spine is more commonly affected in children than the upper cervical spine. The location is also in the body of the vertebra sparing the pedicles and the posterior spinal elements or the soft tissues. Thus, there is minimal instability and few neurological signs [3]. The clinical picture is mainly muscular symptoms with a restricted range of motion [3]. Radiological findings on an X-ray showed a lytic lesion of the vertebral body with a possible partial collapse. Sometimes, a complete collapse of the vertebral body produces ‘‘vertebra plana” picture [5]. However, unlike adults, children before skeletal maturity have adequate remodeling potential to reform the vertebral body [6].
Differential diagnoses of solitary EG of the spine include osteoblastoma, aneurysmal bone cyst, Ewing sarcoma, acute leukemia, Gaucher disease, and metastatic tumor [7]. Bone scintigraphy is, therefore, a recommended screening method to rule out multiple foci (even though low sensitivity) to exclude other severe differentials. Histopathology is confirmatory, with EG displaying scattered eosinophils (not necessary for diagnosis) and clusters/aggregates of lymphocytes, histiocytes, and hallmark Langerhan cells, often associated with areas of fibrosis. With passage of time, the lesion tends to be more fibrotic and less cellular, which may require ancillary tools such as IHC to highlight the scattered characteristic Langerhan cells [8]. Healed lesions become more sclerotic on radiographs or can entirely resolve.
Solitary EG is usually a self-limiting disorder and spontaneous healing is possible [2]. (? there are many case of spontaneous healing after biopsy) Capanna et al. described intralesional steroid infiltration for treatment [9]. Some authors advocate operative treatment such as surgical curettage and bone grafting of the lesion [2, 10]. Utility of local radiation therapy and chemotherapy is also reported, especially for lesions for which surgical complications would be high, and for cases with multifocal bone lesions [11]. Nevertheless, radiation poses a risk of radiation myelitis or secondary malignancy and is best avoided in children with growth potential [12]. Surgical treatment option should therefore be reserved for specific cases such as presence of neurologic defects or instability [3].
EG is a rare benign lesion sometimes seen the children. Since these have many radiological mimickers in the spine, these warrant proper investigation and histopathological correlation for accurate diagnosis and appropriate management. The lesions are self-resolving, though occasionally may need surgical, radiation, or chemotherapy in selective cases.
EG is a benign tumorous lesion that affects mostly children or young adults in the flat or the long bones, causing lysis. It is infrequent to affect the pediatric spine. A thorough workup is necessary in such a situation to rule out other severe conditions which can mimic EG.
References
- 1.Baber WW, Numaguchi Y, Nadell JM, Culicchia F, Robinson AE. Eosinophilic granuloma of the cervical spine without vertebrae plana. J Comput Tomogr 1987;11:346-9. [Google Scholar]
- 2.Scarpinati M, Artico M, Artizzu S. Spinal cord compression by eosinophilic granuloma of the cervical spine. Case report and review of the literature. Neurosurg Rev 1995;18:209-12. [Google Scholar]
- 3.Bertram C, Madert J, Eggers C. Eosinophilic granuloma of the cervical spine. Spine (Phila Pa 1976) 2002;27:1408-13. [Google Scholar]
- 4.Chadha M, Agarwal A, Agarwal N, Singh MK. Solitary eosinophilic granulome of the radius. An unusual differential diagnosis. Acta Orthop Belg 2007;73:413-7. [Google Scholar]
- 5.Compere EL, Johnson WE, Coventry MB. Vertebra plana (Calvé’s disease) due to eosinophilic granuloma. J Bone Joint Surg Am 1954;36-A:969-80. [Google Scholar]
- 6.Greenlee JD, Fenoy AJ, Donovan KA, Menezes AH. Eosinophilic granuloma in the pediatric spine. Pediatr Neurosurg 2007;43:285-92. [Google Scholar]
- 7.Reddy PK, Vannemreddy PS, Nanda A. Eosinophilic granuloma of spine in adults: A case report and review of literature. Spinal Cord 2000;38:766-8. [Google Scholar]
- 8.Mardi K, Thakur RC, Negi L. Intradural eosinophilic granuloma invading skull: Case report and review of the literature. Asian J Neurosurg 2017;12:698-700. [Google Scholar]
- 9.Capanna R, Springfield DS, Ruggieri P, Biagini R, Picci R, Bacci G, et al. Direct cortisone injection in eosinophilic granuloma of bone: A preliminary report on 11 patients. J Pediatr Orthop 1985;5:339-42. [Google Scholar]
- 10.Lauffenburger MD, Dull ST, Toselli R. Eosinophilic granuloma of the adult spine: A case report and review of the literature. J Spinal Disord 1995;8:243-8. [Google Scholar]
- 11.Olschewski T, Seegenschmiedt MH. Radiotherapy of Langerhans’ cell histiocytosis: Results and implications of a national patterns-of-care study. Strahlenther Onkol 2006;182:629-34. [Google Scholar]
- 12.Johansson L, Larsson LG, Damber L. A cohort study with regard to the risk of haematological malignancies in patients treated with x-rays for benign lesions in the locomotor system: II. Estimation of absorbed dose in the red bone marrow. Acta Oncol (Madr) 1995;34:721-6. [Google Scholar]