When the femoral head dislodges from the trunnion and is allocated on the anterior acetabular rim, it should be handled carefully, due to the serious risk of intrapelvic migration.
Dr. Sérgio Pita, Department of Orthopaedics and Traumatology, Avenida Artur Ravara 35, 3810-164 Aveiro, Portugal. E-mail: sergioenfpita@gmail.com
Introduction: Intrapelvic migration of the femoral head is a rare complication of total hip arthroplasty (THA).
Case Report: A 54-year-old Caucasian female was submitted to revision THA. She suffered an anterior dislocation and avulsion of the prosthetic femoral head that required open reduction. Intraoperatively, the femoral head migrated into the pelvis, along the psoas aponeurosis. The migrated component was retrieved on a subsequent procedure, through an anterior approach to the iliac wing. The patient had a good post-operative course and 2 years after surgery she has no complains related to this complication.
Conclusion: Most of the cases described in the literature are of intraoperative migration of trial components. The authors found only one case described involving a definitive prosthetic head, but during primary THA. No case was found due to post-operative dislocation or definitive femoral head migration after revision surgery. Due to the lack of long-term studies of intra pelvic implant retention, we recommend to remove these implants, particularly in younger patients.
Keywords: Intrapelvic migration, femoral head, total hip arthroplasty, revision total hip arthroplasty.
Total hip arthroplasty (THA) is a safe, reliable, and cost-efficient treatment for symptomatic hip osteoarthritis [1, 2]. Many complications related to this procedure have been extensively described in the literature [3, 4]. Intrapelvic migration of the femoral head is a very rare complication, only described in a few case reports [1], and most of them involve trial heads. Dealing with such complication and making decisions regarding its management is challenging for every surgeon [2]. We report a unique case of intrapelvic migration of the definitive femoral head, after revision THA, and the strategy to retrieve it.
A 54-year-old Caucasian female presented with atraumatic, chronic, and painful left hip. She had an uncemented metal-on-polyethylene THA performed 19 years priorly, due to osteoarthritis secondary to developmental hip dysplasia, with no other medical history of relevance for this case. The radiological study revealed asymmetrical wearing of the polyethylene liner, without other apparent complications. She was, then, proposed for revision surgery (Fig. 1).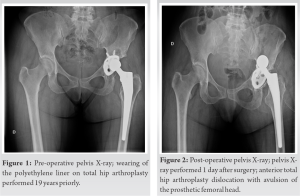
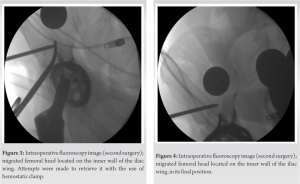
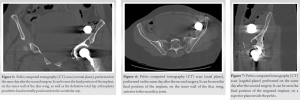
A literature review was performed on PubMed database, using the keywords “intrapelvic migration,” “femoral head,” “THA,” and “revision THA.” Fifteen articles, comprising a total of 26 clinical case reports, were found relevant for the discussion of this clinical case. Intraoperative complications may occur during THA in up to 5, 4% of cases, being iatrogenic fractures of the femur the most common scenario [1]. Intrapelvic migration of the femoral head is a much more uncommon event, only described in a few case reports. Siddiqi et al. described an incidence of <0.001% [1], while Rachbauer et al. reported four cases in a total of 6207 procedures [3]. This incidence may actually be higher, but in most cases, the dislocated femoral head is visualized in the operative field and immediately retrieved, so they are probably not described in the literature [5]. Besides its low incidence, it is one of the most frustrating (yet avoidable) situations to manage during THA [5] and is a very challenging situation, where the surgeon needs to make a decision whether to leave the lost component in its place or remove it [6]. Intrapelvic migration of the femoral head does not seem to be surgical approach related – we found cases described for posterior [1, 2, 4, 7, 8, 9], lateral [5, 6, 10, 11, 12], and anterolateral [1, 13, 14, 15] approaches. One common fact to all approaches is that small incisions may lead to increased prevalence of such complication, due to the limited size of the surgical field [14] but also as a result of the higher soft-tissue tension [13]. There are three mechanisms that usually lead to femoral head dislodgement from the femoral stem: separation either during reduction maneuvers, while assessing anterior stability or during dislocation after completing the implant trialing. The latter seems to be the most common mechanism for intrapelvic migration of the femoral head [1]. Our case is quite unique in the way that the dislodgement occurred during anterior hip dislocation, after the surgery. This fact was probably due to the head not having been correctly hammered into the femoral stem. The path for the intrapelvic migration is usually the soft-tissue gap created after anterior capsulotomy [3], performed in lateral and anterolateral approaches or even the small rentcreated for retractor placement in these approaches and in posterior approaches as well [1]. The plane of the psoas muscle bursa seems to be the path of least resistance and the final position of the implant is commonly in the posterior pelvis, anterior to the sacroiliac joint [15] in the retroperitoneal space. There is only one report, where the femoral head was found inside the peritoneal space [14]. In most cases, the simple dislodgement of the prosthetic head is not enough for intrapelvic migration, but as the surgeon or his assistant try to grasp it, they may inadvertently push it further into the pelvis [1, 4, 5, 6, 7, 8, 10, 11, 13, 14, 15]. Two distinctive features in our case are that occurred after revision THA and the dislodged implant was the prosthetic femoral head. There are only two other cases described after revision THA, but involved trial heads [6, 9], and only one other that involved migration of the definitive implant, but after primary THA and the head was not retrieved [11]. The vast majority of the cases in the literature involve migration of trial implants and during primary THA. When dealing with such complication, a decision has to be made whether to remove the migrated femoral head or not. Interestingly, in the report by Ozkan et al., that involved a prosthetic head, due to the patient old age the implant was not removed, and she did not developed symptoms related to it [11]. There are other cases, in which it was decided not to remove the implants, but they happened with trial heads [7, 8, 9, 10, 11]. It is stated that due to the lack of studies about the effects of long-term retention of these implants, they should be removed [1]. Some more straightforward indications seem to be the compression of neurovascular structures or the ureter, patient’s young age [10, 13] or the development of peritoneal irritation signs [14]. In the present case, given the patient’s young age and the fact that the metallic component could give rise to an inflammatory local response, it was decided to remove it. There is no consensus on the surgical timing to remove the implant [1]. It seems logical that would be optimal to retrieve it on the same surgical procedure, but the implant may acquire a position not completely clear to the surgeon, and an imagiological study can help on the pre- operative planning. As we were not familiar with such complication and could not retrieve the femoral head even with the aid of fluoroscopy, the CT scan was advantageous to identify its final position and plan on how to remove it. Hamoui et al. also performed a CT scan before the removal, but were able to do it with the patient under anesthesia and did the procedure on the same surgical timing [4]. However, in most cases described in the literature, the implant was removed on the same surgery [1, 4, 6, 8, 9, 12, 13, 15]. It is not always possible to retrieve the femoral head through the same initial incision, but some authors describe such situation. Ikeuchi et al. were successful by applying pressure on the hypogastrium and inserting a Kocher clamp on the anterior capsular defect to prevent any further migration and could retrieve it with fingers [8]. Madsen et al. used a Satinsky clamp through the capsular defect to block further migration and were able to retrieve the implant with a Kocher clamp (15). Princep enlarged a lateral incision proximally, flexed the hip to decrease muscle tension, and were able to push the femoral head with fingers back to the surgical field [12]. However, when this is not possible through the same incision, an anterior approach to the iliac wing [2, 4, 13] or ilioinguinal approach [1, 5, 9] seem to be the more direct pathways (depending on the final position of the implant) and, therefore, the most commonly described approaches. Of notice, are also the strategies described by Kalra et al., that experienced this complication while performing a lateral approach, and were able to push the implant posteriorly and retrieved it through a posterior approach on the same surgical timing [6]; and by Alfonso et al., that retrieved the implant laparoscopically, performed by a General Surgeon, after the implant had acquired an intraperitoneal position [14].
Most of the cases described in the English literature are of intraoperative migration of trial components. The authors only found one case described involving a definitive prosthetic head, but during primary THA. No case was found due to post-operative dislocation or definitive femoral head migration after revision surgery. Femoral head dislodgment from the trunnion is a complication possible not only during intraoperative implant trialling but also after closed hip dislocation. When this happens, particularly during anterior dislocation, surgeon and assistant should be aware of the expected positioning of the implant on the anterior acetabular rim and the possibility of intrapelvic migration. Therefore, they should handle the femoral head carefully. If the femoral head migrates into the pelvis, a CT scan can be useful for the pre-operative planning, and the surgeon should be familiar with anterior approaches to the iliac wing. Due to the lack of long-term studies of intra pelvic implant retention, the recommendation at our institution is to remove these implants, particularly in younger patients.
Intrapelvic migration of the femoral head is a very rare, but yet possible, complication during THA. Surgeons that perform this surgery on a regular basis should be aware of such possible event and handle this implant with care when it is inside the surgical field and dissociates from the trunnion, particularly when it is positioned on the anterior rim of the acetabulum. The path of least resistance, and hence the most common pathway for migration, is the psoas muscle bursa and the final position of the implant is commonly in the posterior pelvis, anterior to the sacroiliac joint. CT scan of the pelvis is a useful tool for pre-operative planning and surgeons should be familiar with anterior approaches to the iliac wing for retrieval of the migrated component.
References
- 1.Siddiqi A, Talmo CT, Bono JV. Intraoperative femoral head dislodgement during total hip arthroplasty: A report of four cases. Arthroplasty Today 2018;4:44-50. [Google Scholar]
- 2.Citak M, Klatte TO, Zahar A, Day K, Kendoff D, Gehrke T, et al. Intrapelvic dislocation of a femoral trial head during primary total hip arthroplasty requiring laparotomy for retrieval. Open Orthop J 2013;7:169-71. [Google Scholar]
- 3.Rachbauer F, Nogler M, Krismer M, Moritz M. Intraoperative migration of the trial femoral head into the pelvis during total hip arthroplasty: Prevention and retrieval. J Bone Joint Surg Am 2002;84:880-1. [Google Scholar]
- 4.Hamoui M, Larbi A, Delannis Y, Roche O, Fauré P, Canovas F. Pitfall in total hip arthroplasty: Intraoperative migration of the trial femoral head through the iliopsoas muscle. Eur J Orthop Surg Traumatol 2012;22:713-6. [Google Scholar]
- 5.Bicanic G, Crnogaca K, Simunovic M, Delimar D. Dislocated trial femoral head during total hip arthroplasty: Review of the literature and the new algorithm for treatment. BMJ Case Rep 2015;2015:bcr2014208693. [Google Scholar]
- 6.Kalra K, Ries MD, Bozic KJ. Intrapelvic displacement of a trial femoral head during total hip arthroplasty and a method to retrieve it. J Arthroplasty 2011;26:338.e21-3. [Google Scholar]
- 7.Vertelis A, Vertelis L, Tarasevicius S. Trial femoral head loss in to the soft tissues of pelvis during primary total hip replacement: A case report. Cases J 2008;1:151. [Google Scholar]
- 8.Ikeuchi K, Hasegawa Y, Warashina H, Seki T. Intraoperative migration of the trial femoral head into the pelvis during total hip arthroplasty-report of two cases. Nagoya J Med Sci 2014;76:203-10. [Google Scholar]
- 9.Callaghan J, Mcandrew C, Boese KC, Forest, E. Intrapelvic migration of the trial femoral head during total hip arthroplasty: Is retrieval necessary? A report of four cases. Iowa Orthop J 2006;26:60-2. [Google Scholar]
- 10.Batouk O, Gilbart M, Jain R. Intraoperative dislocation of the trial femoral head into the pelvis during total hip arthroplasty-a case report. J Bone Joint Surg Am 2001;83:1549-51. [Google Scholar]
- 11.Ozkan K, Ugutmen E, Altintas F, Eren A, Mahirogullari M. Intraoperative dislocation of the prosthetic femoral head into the pelvis during total hip arthroplasty. Acta Orthop Belg 2008;74:553-5. [Google Scholar]
- 12.Princep A. Intraoperative migration of the trial femoral head into the pelvis during total hip arthroplasty: Prevention and retrieval. J Bone Joint Surg Am 2002;84:880-1. [Google Scholar]
- 13.Ziv YB, Backstein D, Safir O, Kosashvili Y. Intraoperative dislocation of a trial femoral head into the pelvis during total hip arthroplasty. Can J Surg 2008;51:E73-4. [Google Scholar]
- 14.Alfonso D, Idjadi J, Lamont JG. Retrieval of a trial femoral head that displaces into the periacetabular soft tissue during mini-incision total hip arthroplasty: A case report. J Bone Joint Surg 2006;88:866-8. [Google Scholar]
- 15.Madsen WY, Mitchell BS, Kates SL. Successful intraoperative retrieval of dislocated femoral trial head during total hip arthroplasty. J Arthroplasty 2012;27:820.e9-11. [Google Scholar]