In a country like India, were tuberculosis is endemic, osteoarticular tuberculosis should always be kept as a differential diagnosis, until unless proved otherwise, and histopathological confirmation along with newer diagnostic tests not only helps to confirm the diagnosis but also helps in ascertaining drug resistance if any.
Dr. Ruchit Khera, Department of Orthopaedics, Himalayan Institute of Medical Sciences, Swami Rama Himalayan University, Swami Ram Nagar, Dehradun, Uttarakhand, India. E-mail: ruchit1982@gmail.com
Introduction: Tuberculosis is one of the well-known diseases with significant morbidity and financial burden on the society and health care. Tubercular osteomyelitis constitutes about 10–11% of all extra-pulmonary tuberculosis cases. Disease is believed to be a great imposter, as disease may present in varied forms and/or in atypical sites, making it prone to be missed or misdiagnosed.
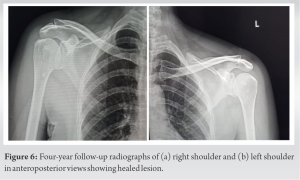
Case Report: We report a case of tuberculosis of bilateral acromion process in a 53-year-old female who was managed elsewhere for 18 months with physiotherapy. The patient presentation, diagnostic approach, and management along with follow have been discussed in details.
Conclusion: We conclude that tuberculosis could affect any bone of the body and may have unusual presentation. Deferential diagnosis of tubercular osteomyelitis/arthritis should always be kept as a differential and ruled out. Histopathological diagnosis is still a gold standard for confirmation of the same.
Keywords: Osteoarticular tuberculosis, acromion process, bone and joint infections, antitubercular therapy
Tuberculosis is one of the well-known diseases with significant morbidity and financial burden on the society and health care. It is believed that tuberculosis affects about 1/3rd of population at some point of the life [1]. Tubercular osteomyelitis and arthritis together account for about 1–4.7% of all cases and almost 11% of all extra-pulmonary cases, however, spine is most commonly affected extra-pulmonary site [2].
Atypical presentation of tubercular osteomyelitis is common and often misdiagnosed or missed diagnosed, being a great masquerader with variegated presentation [3]. We hereby present case of a 53-year-old female who presented in the outpatient department with the complaints of moderate pain involving right shoulder region for 18 months duration and in the left shoulder region for 6 months along with non-healing ulcer over posterior aspect of shoulder for 4 months duration. Patient’s symptoms were localized to anterior shoulder and along acromion process, where patient use to have pain on attempting movements on Shoulder beyond 90° of abduction. Examination revealed tenderness along acromion bilaterally, range of motion was complete but painful beyond 90° of abduction and flexion. Internal and external rotations were terminally painful. Non-healing ulcer of about 3 × 1.5 cm was present over posterior aspect of the left shoulder with bluish skin edges, margins were inverted with slough present on ulcer base with no active pus discharge. On probing the ulcer bed, exposed part of acromion could be appreciated (Fig. 1).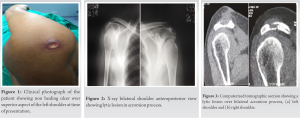
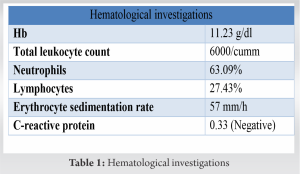
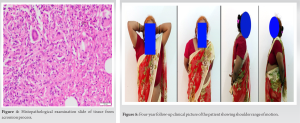
India has highest incidence of reported tuberculosis patients in the world accounting to 2.8 million cases per year, that is, more then quarter of world tuberculosis burden. India continues to be on high burden list of countries by the WHO for tuberculosis with almost 87% of new cases in 2018. One of the reasons for high incidence of tuberculosis is its varied presentation mainly in extra-pulmonary cases, often leading to misdiagnosis o missed diagnosis. Tubercular osteomyelitis accounts for about 1–4.7% of all tuberculosis cases and about 10–11% of extra-pulmonary tuberculosis cases, with spine and other weight-bearing joint most commonly being affected. Osteoarticular involvement is usually secondary to hematogenous spread from elsewhere in the body [2]. Early symptoms such as mild pain on range of motion or minimal swelling are often overlooked in absence of positive history, pulmonary symptoms, or systemic signs, leading to either misdiagnosis or missed diagnosis [4]. First case of tubercular osteomyelitis dates back to 1950 in a series of 1074 cases of unusual location of tubercular osteomyelitis. Only hand full of cases of tuberculosis of acromion process have been reported [3, 5]. Li et al. reported 14 out of 16 cases of tuberculosis of glenohumeral joint misdiagnosed as frozen shoulder. Author concluded that diagnosis of tuberculosis should be kept as a differential in all the cases of long-standing shoulder pain [6]. Gold standard for diagnosis is biopsy showing the typical tubercles [7]. ZN staining is the easy and quick diagnostic test but is limited by its low sensitivity (46–78%), although its specificity is virtually 100% [8]. Newer modified fluorescent such as auramine and rhodamine is believed to have better detection rate compared to ZN stain [9]. The treatment of tubercular osteomyelitis is primarily by chemotherapy, which has proven effective over years, until unless complicated with comorbid factors or with MDR or XDR strains of tuberculosis. Refractory cases may require debridement of the tissue to decrease bacterial load and enhance drugs penetration. Duration of chemotherapy for osteoarticular tuberculosis has been a matter of debate with regimen periods ranging from 9 to 18 months, still there is no consensus regarding the same [10]. In our case also, the patient has taken treatment from elsewhere for a period of 14 months for shoulder pain and was being managed with physiotherapy, until about 4 months back patient developed blister which ruptured to ooze out pus which was initially managed with local antibiotics and latter patient was referred to our center for further management. It is in the absence of constitutional symptoms and absence of any positive contact of tuberculosis that many patients are not diagnosed early. It is also important to understand that osteoarticular tuberculosis can be an isolated or a primary lesion also. In a country like India which is endemic for tuberculosis, diagnosis of tubercular osteomyelitis/arthritis should always be kept as a differential and ruled out.
We conclude that tuberculosis could affect any bone of the body and may have unusual presentation. Deferential diagnosis of tubercular osteomyelitis/arthritis should always be kept as a differential and ruled out. Histopathological diagnosis is still a gold standard for confirmation of the same.
Osteoarticular tuberculosis is well known entity for its varied presentation in terms of symptoms and site as well. We recommend that in a country like India, were tuberculosis is endemic, osteoarticular tuberculosis should always be kept as a differential diagnosis, until unless proved otherwise. Histopathological confirmation along with newer diagnostic tests not only helps to confirm the diagnosis but also helps in ascertaining drug resistance if any.
References
- 1.Abdelwahab IF, Kenan S, Hermann G, Lewis M, Klein M, Rabinowitz JG. Atypical skeletal tuberculosis mimicking neoplasm. Br J Radiol 1991;64:551-5. [Google Scholar]
- 2.World Health Organization. Global Tuberculosis Report 2017. Geneva: World Health Organization; 2017. Available from: https://www.who.int/tb/publications/global_report/gtbr2 017_main_text.pdf [Last assessed on 2021 Dec 01]. [Google Scholar]
- 3.Cheng J, Feng S, Lei H, Huo W, Feng H. Tuberculosis of acromioclavicular joint: A case report. BMC Infect Dis 2019;19:111. [Google Scholar]
- 4.Marudanayagam A, Gnanadoss JJ. Multifocal skeletal tuberculosis: A report of three cases. Iowa Orthop J 2006;26:151-3. [Google Scholar]
- 5.Agarwal A, Bhandari A, Maheshwari R Tuberculosis of acromioclavicular joint. J Clin Diagn Res 2017;11:RD03-4. [Google Scholar]
- 6.Li JQ, Tang KL, Xu HT, Li Q, Zhang SX. Glenohumeral joint tuberculosis that mimics frozen shoulder: A retrospective analysis. J Shoulder Elbow Surg 2012;21:1207-12. [Google Scholar]
- 7.Ellis ME, Ramahi KM, Dalaan AN. Tuberculosis of peripheral joints. A dilemma in diagnosis. Int J Tuberc Lung Dis 1993;74:399-404. [Google Scholar]
- 8.Morris BS, Varma R, Garg A, Awasthi M, Maheshwari M. Multifocal musculoskeletal tuberculosis in children: Appearances on computed tomography. Skeletal Radiol 2002;31:1-8. [Google Scholar]
- 9.Annam V, Kulkarni MH, Puranik, RB. Comparison of the modified fluorescent method and conventional Ziehl-Neelsen method in the detection of acid fast bacilli in lymphnode aspirates Cytojournal 2009;6:13. [Google Scholar]
- 10.Tuli SM. Tuberculosis of Skeletal System (Bones, Joints, Spine and Bursal Sheaths). 3rd ed. New Delhi: Jaypee Brothers; 2004. p. 167-8. [Google Scholar]