Robotic-assisted total knee arthroplasty for osteoarthritis with windswept deformity.
Dr. Takao Kaneko, Department of Orthopedic, Ichinomiya Onsen Hospital, Adult Reconstruction Center, Japan. E-mail: takao-knee@oha.toho-u.ac.jp
Introduction: Windswept deformity (WD) refers to valgus deformity in one knee and varus deformity in the other. We performed robotic-assisted (RA) total knee arthroplasty (TKA) for osteoarthritis of the knee with WD, made patient reported outcome measurements (PROMs), and performed gait analysis based on triaxial accelerometery.
Case Report: A 76-year-old woman presented to our hospital with bilateral knee pain. Image-free handheld RA TKA was performed on the left knee with severe varus deformity and severe pain during walking. RA TKA was performed on the right knee with severe valgus deformity 1 month later. The RA technique was used to determine implant positioning and the plan for osteotomy intraoperatively, taking into account soft-tissue balance. This made it possible to use a posterior stabilized implant instead of a semi-constrained implant for severe valgus knee deformity with flexion contracture (Krachow classification Type 2). At 1 year after TKA, PROMs were inferior in the knee with pre-operative valgus deformity. Gait ability improved after surgery. Even with the RA technique, it took 8 months to achieve left-right balance while walking and for the variability of the gait cycle to become equivalent to that of a normal knee.
Conclusion: Primary RA TKA is a viable option for osteoarthritis of the knee with WD. It took time for the gait ability of both knees to become equal and PROMs were better with the varus deformity compared to before surgery.
Keywords: Windswept deformity, robotic assisted total knee arthroplasty, patient reported outcome measurements, triaxial accelerometer, gait ability.
Windswept’ deformity (WD) refers to valgus deformity in one knee and a varus deformity in the other [1]. Current developments in robotic-assisted (RA) surgical techniques give surgeons intraoperative options for total knee arthroplasty (TKA) that improve accuracy [2, 3]. There have been no reports of primary RA TKA for WD. We performed RA TKA for osteoarthritis of the knee with WD and assessed patient reported outcome measurements (PROMs) and the changes in gait ability over time.
A 76-year-old woman with a body mass index of 20.9 kg/m2 with bilateral knee pain visited our hospital. Pre-operative characteristics of the patient are shown in Table 1. Preoperatively, the right knee had valgus deformity Krakow classification Type 2 [4] and the left knee had varus deformity (Kellgren-Lawrence classification Grade 4) (Fig. 1). 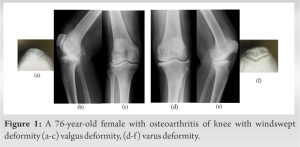
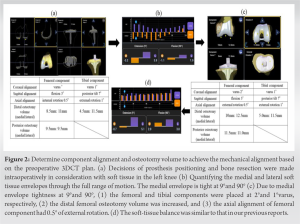
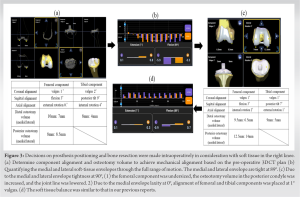

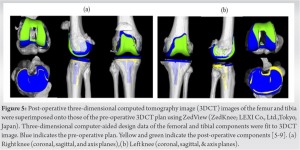
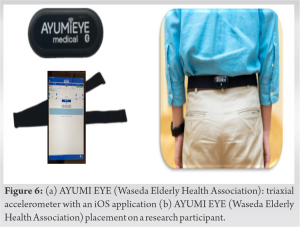
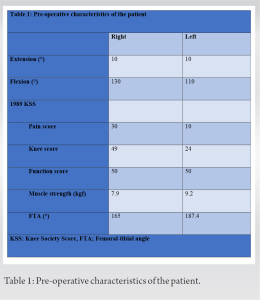
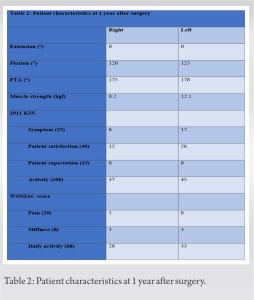
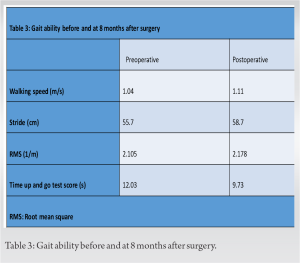
We performed RA TKA for osteoarthritis of the knee with WD. The pre-operative deformity of the valgus knee was more severe than of the varus knee in terms of PROMs (except for the 2011 KSS patient expectation score and the WOMAC stiffness score) at 1 after TKA. In addition, the valgus knee was inferior to the varus knee in terms of improvement in quadriceps muscle strength at 1 year after TKA. Gait ability improved after surgery, but even with the RA technique, it took 8 months to achieve left-right balance while walking and for the variability of the gait cycle to become equivalent to that of a normal knee. However, the use of RA technology to treat WD has some greatest advantages. To plan for the desired soft-tissue laxity with the RA technique, varus or valgus stress is applied to tension the soft tissues on the sides of the knee through a full range of flexion. This helps the surgeon plan for implant positioning and volume bone resection, taking into account “virtual” soft-tissue laxity before making any cuts [20, 21, 22, 23]. Similarly, we were able to determine the positioning of the prosthesis and plan for osteotomy intraoperatively to ensure the lack of medial laxity while taking soft-tissue balance into account. Krachow et al. 1991 [4] classified valgus deformity of the knee into three types. Type I was defined as valgus deformity secondary to bone loss in the lateral compartment and soft-tissue contracture with intact medial soft tissue. Type II was defined as obvious attenuation of the medial capsular ligament complex. Type III was defined as severe valgus deformity with valgus malpositioning of the proximal tibial joint line after proximal tibial osteotomy with overcorrection. This patient’s deformity was not passively correctable with the varus test. Ligament release and semi-constrained implants are more frequently used in TKA treatment of Krachow classification Type 2 or severe valgus knee [6, 7, 8]. There has been a report of revision surgery due to medial soft-tissue laxity [24]. In this case, osteotomy volume and component alignment were determined intraoperatively so that the medial soft tissue envelope would be loose and the lateral soft tissue envelope would not be stiff during extension, which allowed us to use a PS implant instead of a semi-constrained implant. On the other hand, Howell et al. 2021 [25] reported that cruciat-retaining implants can be used with calipered kinematically alignment TKA in most patients with WD with comparable outcomes scores and alignment in the paired varus and valgus deformities. Regarding reports that the use of RA technology contributes to rehabilitation, the RA lateral unicompartmental knee arthroplasty (UKA) resulted in significantly faster return to sport compared to conventional jig-based UKA [26] and robotic-arm assisted TKA (MAKO: robotic interactive orthopedic arm system, Stryker, Fort Lauderdale, Florida, USA) had significantly improved 2-year post-operative r- physical function, compared with the conventional jig-based TKA [27].
Primary RA TKA is a viable option for osteoarthritis of the knee with WD. It took time for the gait ability of both knees to become equal and PROMs were better with the varus deformity compared to before surgery. Long follow-up is needed.
Robotic-assisted total knee arthroplasty for osteoarthritis of the knee with wind swept deformity showed inferior pre-operative deformity in valgus compared with varus at 1 year postoperatively, and it took 8 months for the left-right balance and gait cycle variability during walking to become comparable to that of the normal knee.
References
- 1.Meding JB, Anderson AR, Ritter MA, Faris PM, Keating EM. Windswept deformity in bilateral total knee arthroplasty. J Arthroplasty 2000;15:562-6. [Google Scholar]
- 2.Lonner JH, Smith JR, Picard F, Hamlin B, Rowe PJ, Riches PE. High degree of accuracy of a novel image-free handheld robot for unicondylar knee arthroplasty in a cadaveric study. Clin Orthop Relat Res 2015;473:206-12. [Google Scholar]
- 3.Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2019;27:1232-40. [Google Scholar]
- 4.Krachow KA, Jones MM, Teeny SM, Hungerford DS. Primary total knee arthroplasty in patients with fixed valgus deformity. Clin Orthop Relat Res 1991;273:9-18. [Google Scholar]
- 5.Kaneko T, Igarashi T, Takada T, Yoshizawa S, Ikegami H, Musha Y. Robotic-assisted total knee arthroplasty improves the outlier of rotational alignment of the tibial prosthesis using 3DCT measurements. Knee 2021;31:64-76. [Google Scholar]
- 6.Mazzotti A, Perna F, Golinelli D, Quattrini I, Stea S, Bordini B, et al. Preoperative valgus deformity has twice the risk of failure as compared to varus deformity after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2019;27:3041-7. [Google Scholar]
- 7.Peters CL, Jimenez C, Erickson J, Anderson MB, Pelt CE. Lessons learned from selective soft-tissue release for gap balancing in primary total knee arthroplasty: An analysis of 1216 consecutive total knee arthroplasties: AAOS exhibit selection. J Bone Joint Surg Am 2013;16;95:e152. [Google Scholar]
- 8.Rossi R, Rosso F, Cottino U, Dettoni F, Bonasia DE, Bruzzone M. Total knee arthroplasty in the valgus knee. Int Orthop 2014;38:273-83. [Google Scholar]
- 9.Ueyama H, Minoda Y, Sugama R, Ohta Y, Yamamura K, Nakamura S, et al. Two-dimensional measurement misidentifies alignment outliers in total knee arthroplasty: A comparison of two-and three-dimensional measurements. Knee Surg Sports Traumatol Arthrosc 2019;27:1497-503. [Google Scholar]
- 10.Yamamura K, Minoda Y, Mizokawa S, Ohta Y, Sugama R, Nakamura S, et al. Novel alignment measurement technique for total knee arthroplasty using patient specific instrumentation. Arch Orthop Trauma Surg 2017;137:401-7. [Google Scholar]
- 11.Kaneko T, Kono N, Mochizuki Y, Hada M, Sunakawa T, Ikegami H, et al. The influence of compressive forces across the patellofemoral joint on patient-reported outcome after bi-cruciate stabilized total knee arthroplasty. Bone Joint J 2018;100-B:1585-91. [Google Scholar]
- 12.Kaneko T, Kono N, Mochizuki Y, Hada M, Toyoda S, Musha Y. Bi-cruciate substituting total knee arthroplasty improved medio-lateral instability in mid-flexion range. J Orthop 2017;14:201-6. [Google Scholar]
- 13.Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott WM. The new knee society knee scoring system. Clin Orthop Relat Res 2012;470:3-19. [Google Scholar]
- 14.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833-40. [Google Scholar]
- 15.Behrend H, Giesinger K, Giesinger JM, Kuster MS. The “forgotten joint” as the ultimate goal in joint arthroplasty: Validation of a new patient- reported outcome measure. J Arthroplasty 2012;27:430-6.e1. [Google Scholar]
- 16.“AYUMIEYE,” Waseda Elderly Health Association Co., Ltd. Available: https://ayumieye.com [Last accessed on 30 Apr 30]. [Google Scholar]
- 17.Kavanagh JJ, Menz HB. Accelerometry: A technique for quantifying movement patterns during walking. Gait Posture 2008;28:11-5. [Google Scholar]
- 18.Osaka H, Shinkoda K, Watanabe S, Fujita D, Kobara K, Yoshimura Y, et al. Association between trunk acceleration during walking and clinically assessed balance in patients with stroke. NeuroRehabilitation 2017;41:783-90. [Google Scholar]
- 19.Ito T, Ota Y. Comparison of gait analysis between a triaxial accelerometer-based device and an optical motion capture system. Preprints 2020;2020120336. [Google Scholar]
- 20.Battenber AK, Netravali NA, Lonner JH. A novel handheld robotic-assisted system for unicompartmental knee arthroplasty: Surgical technique and early survivorship. J Robot Surg 2020;14:55-60. [Google Scholar]
- 21.Mergenthaler G, Batailler C, Lording T, Servien E, Lustig S. Is robotic-assisted unicompartmental knee arthroplasty a safe procedure? A case control study. Knee Surg Sports Traumatol Arthrosc 2021;29:931-8. [Google Scholar]
- 22.Bollars P, Boeckxstaens A, Mievis J, Kalaai S, Schotanus MG, Janssen D. Preliminary experience with an image-free handheld robot for total knee arthroplasty: 77 cases compared with a matched control group. Eur J Orthop Surg Traumatol 2020;30:723-9. [Google Scholar]
- 23.Oussedik S, Abdel MP, Victor J, Pagnano MW, Haddad FS. Alignment in total knee arthroplasty. Bone Joint J 2020;102-B:276-9. [Google Scholar]
- 24.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: Just how important is it? J Athroplasty 2009;24 (6 Suppl):39-43. [Google Scholar]
- 25.Howell SM, Shelton TJ, Gill M, Hull ML. A cruciate-retaining implant can treat both knees of most windswept deformities when performed with calipered kinematically aligned TKA. Knee Surg Sports Traumatol Arthrosc 2021;29:437-45. [Google Scholar]
- 26.Canetti R, Betailler C, Bankhead C, Neyret P, Servien E, Lustig S. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: A comparative study. Arch Orthop Trauma Surg 2018;138:1765-71. [Google Scholar]
- 27.Marchand KB, Moody R, Scholl LY, Stoker MB, Taylor KB, Mont MA, et al. Results of robotic-assisted versus manual total knee arthroplasty at 2-year follow-up. J Knee Surg 2023;36:159-66. [Google Scholar]