This article describes the rare occurrence of a discoid lateral and medial meniscus in bilateral knees and notes that asymptomatic discoid menisci typically have a good course and do not require treatment, while symptomatic discoid menisci do.
Dr. Kazuya Kaneda, Department of Orthopedic Surgery, National Hospital Organization Tokyo Medical Center, Meguro 152-8902, Tokyo, Japan. E-mail: kazpleasure@gmail.com
Introduction: A discoid meniscus is a typical anatomical variation of the knee. There are several cases of either lateral or medial discoid menisci; however, their combination is rare. We describe a rare instance of bilateral discoid medial and lateral menisci.
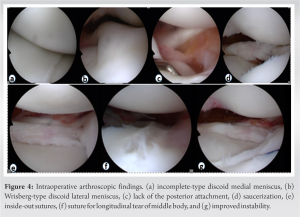
Case Report: A 14-year-old boy who developed left knee pain after twisting his knee at school was referred to our hospital. He had limited extension of –10°, lateral clicking, and pain on the McMurray test in the left knee and complained of slight clicks in the right knee. Magnetic resonance imaging results for both knees revealed discoid medial and lateral menisci. Surgery was performed on the symptomatic left knee. Arthroscopically, a Wrisberg-type discoid lateral meniscus and an incomplete-type medial discoid meniscus were confirmed. The symptomatic lateral meniscus was saucerized and sutured and only the asymptomatic medial meniscus was observed. The patient was doing well 24 months after surgery.
Conclusion: We report a rare case of bilateral medial and lateral discoid menisci.
Keywords: Discoid lateral meniscus, discoid medial meniscus, bilateral discoid menisci, arthroscopic surgery.
A discoid meniscus is a typical anatomical variation of the knee. Asian populations are more likely to have a discoid lateral meniscus than Western and American population [1]. Many discoid lateral menisci (DLM) and discoid medial menisci (DMM) have been reported. The combination of DMM and DLM is rare and only two cases of bilateral DMM and DLM have been reported [2, 3]. Here, we report a rare case of bilateral DMM and DLM.
A 14-year-old boy twisted his left knee while at school and developed left knee pain. Two months of rest showed no improvement; therefore, the patient visited a local clinic. Examination and magnetic resonance imaging (MRI) at a local clinic revealed a lateral meniscus injury in his left knee. He was immediately referred to our hospital because of worsening pain in the left knee joint. At our hospital, a physical examination revealed pain at the lateral femorotibial joint of his left knee as well as a restriction in the range of motion (ROM), with an extension and flexion range of -10° and 150°, respectively. The McMurray test revealed left knee lateral discomfort and lateral clicking during flexion and extension of the knee joint. No signs of intra-articular effusion were observed. As for the right knee, there was no ROM limitation or pain, although clicking was observed on the lateral side of the femorotibial joint. The lateral femoral condyles in both knees were hypoplastic, but there were no additional indirect indications of a discoid lateral meniscus, such as an increased joint space, a high fibular head, or hypoplasia of the lateral tibial plateau, as seen on the X-ray (Fig. 1). 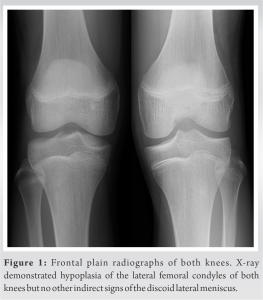

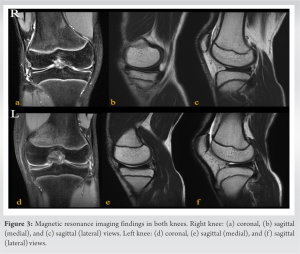
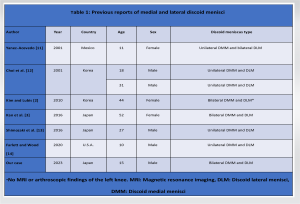
A discoid meniscus is a congenital deformity of the knee joint that is associated with mechanical abnormalities, sometimes causing pain, ROM limitation, or locking. Smillie reported that a discoid meniscus may be caused by an interruption in the process of normal meniscus formation from the originally complete disc-shaped meniscus during the late fetal period [4]. In contrast, Clark and Ogden reported that in the early stages of fetal development, the meniscus had a normal form [5], and the process of discoid meniscus development remains unknown. The incidence of DLM is reported to range from 0.4% to 17%, and 5% to 25% of patients have bilateral DLM [1, 3, 6, 7, 8]. According to reports, people in Asian countries are more likely than people in Western countries to experience discoid meniscus [1], with reports from South Korea indicating that 79–97% of symptomatic DLM patients have DLM in the contralateral knee [9]. The incidence of DMM is reported to be 0.03–0.3% [3, 6, 7], and that of bilateral DMM is 0.0056–0.012% [10]. The coexistence of DMM and DLM in the same knee is rare and bilateral cases have rarely been reported. Our case is the third reported [2, 3, 11, 12, 13, 14] (Table 1). The patient may have joint effusion, a lack of terminal extension, a positive McMurray test, or joint line discomfort on physical examination. Signs of clicking or popping on extension may occur, which is a specific sign of discoid meniscus [15]. Radiographs are not necessary, but may lead to diagnosis [7]. Some patients may exhibit the following symptoms: Widening of the lateral joint space, squaring of the lateral femoral condyle, cupping of the lateral tibial plateau, hypoplasia of the tibial eminence, the condylar cutoff sign, and a high fibular head [6, 7, 8]. MRI is the most important support tool for surgeons. Samoto et al. advocated diagnostic criteria based on MRI [16]. The accurate diagnostic criterion was either the ratio of the minimum meniscal width to the maximum tibial width on the coronal slice of >20% or the ratio of the sum of the width of the anterior and posterior horns to the meniscal diameter on the sagittal slice showing a maximum meniscal diameter of >75%. The present case also met these diagnostic criteria. Ahn et al. suggested an MRI classification that can predict meniscal peripheral tears and instability [17] and can be used for surgical planning. Asymptomatic patients require non-surgical treatment and follow-up. Conventionally, total meniscectomy was chosen for symptomatic patients; however, it is not easily recommended because it may lead to a high risk of osteoarthritis [6, 7, 8]. Currently, arthroscopic partial meniscectomy, i.e., saucerization to make the abnormal meniscus into a normal shape and size is preferred for symptomatic torn discoid menisci [7]. The width of the remaining peripheral rim during saucerization is an important factor [7]. Yamasaki et al. reported that a residual peripheral rim smaller than 5 mm wide caused meniscal extrusion and degenerative alterations in the knee joint [18]. Furthermore, Zhang et al. studied increased valgus alignment after total meniscectomy or meniscoplasty for DLM [19]. Although no clinical conclusion has yet been reached, there are reports of short-term results for discoid meniscus with centralization, in addition to saucerization [20]. It is also known that osteochondritis dissecans may occur after discoid meniscus surgery [6, 7, 8], and continuous follow-up is required even after surgery.
Here, we report a rare case of bilateral DLM and DMM. The left torn lateral discoid meniscus was arthroscopic saucerized and sutured, while the remaining asymptomatic menisci were left alone. 24 months postoperatively, the patient was able to engage in fitness activities.
We have reported the rare but common presence of bilateral DMM and DLM. Treatment is necessary for discoid menisci with symptoms, while it is not necessary and has a favorable outcome for those with asymptomatic menisci.
References
- 1.Yaniv M, Blumberg N. The discoid meniscus. J Child Orthop 2007;1:89-96. [Google Scholar]
- 2.Kim SJ, Lubis AM. Medial and lateral discoid menisci: A case report. Sports Med Arthrosc Rehabil Ther Technol 2010;2:21. [Google Scholar]
- 3.Kan H, Arai Y, Nakagawa S, Inoue H, Minami G, Ikoma K, et al. Medial and lateral discoid menisci of both knees. Knee Surg Relat Res 2016;28:330-3. [Google Scholar]
- 4.Smillie IS. The congenital discoid meniscus. J Bone Joint Surg Br 1948;30B:671-82. [Google Scholar]
- 5.Clark CR, Ogden JA. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am 1983;65:538-47. [Google Scholar]
- 6.Kim JG, Han SW, Lee DH. Diagnosis and treatment of discoid meniscus. Knee Surg Relat Res 2016;28:255-62. [Google Scholar]
- 7.Kim JH, Ahn JH, Kim JH, Wang JH. Discoid lateral meniscus: Importance, diagnosis, and treatment. J Exp Orthop 2020;7:81. [Google Scholar]
- 8.Flouzat-Lachaniette CH, Pujol N, Boisrenoult P, Beaufils P. Discoid medial meniscus: Report of four cases and literature review. Orthop Traumatol Surg Res 2011;97:826-32. [Google Scholar]
- 9.Ahn JH, Lee SH, Yoo JC, Lee HJ, Lee JS. Bilateral discoid lateral meniscus in knees: Evaluation of the contralateral knee in patients with symptomatic discoid lateral meniscus. Arthroscopy 2010;26:1348-56. [Google Scholar]
- 10.Lukas K, Livock H, Kontio K, Carsen S. Bilateral discoid medial menisci: A case report and review of the literature. J Am Acad Orthop Surg Glob Res Rev 2020;4:e20.00069. [Google Scholar]
- 11.Yáñez-Acevedo A. Bilateral discoid lateral menisci and unilateral discoid medial menisci. Arthroscopy 2001;17:772-5. [Google Scholar]
- 12.Choi NH, Kim NM, Kim HJ. Medial and lateral discoid meniscus in the same knee. Arthroscopy 2001;17:E9. [Google Scholar]
- 13.Shimozaki K, Nakase J, Ohashi Y, Numata H, Oshima T, Takata Y, et al. Ipsilateral medial and lateral discoid meniscus with medial meniscus tear. J Orthop Case Rep 2016;6:9-12. [Google Scholar]
- 14.Farlett J, Wood JR. Ipsilateral medial and lateral discoid menisci: A rare combination of infrequent anatomic variants. J Clin Imaging Sci 2020;10:11. [Google Scholar]
- 15.Harato K, Niki Y, Nagashima M, Masumoto K, Otani T, Toyama Y, et al. Arthroscopic visualization of abnormal movement of discoid lateral meniscus with snapping phenomenon. Arthrosc Tech 2015;4:e235-8. [Google Scholar]
- 16.Samoto N, Kozuma M, Tokuhisa T, Kobayashi K. Diagnosis of discoid lateral meniscus of the knee on MR imaging. Magn Reson Imaging 2002;20:59-64. [Google Scholar]
- 17.Ahn JH, Lee YS, Ha HC, Shim JS, Lim KS. A novel magnetic resonance imaging classification of discoid lateral meniscus based on peripheral attachment. Am J Sports Med 2009;37:1564-9. [Google Scholar]
- 18.Yamasaki S, Hashimoto Y, Takigami J, Terai S, Takahashi S, Nakamura H. Risk factors associated with knee joint degeneration after arthroscopic reshaping for juvenile discoid lateral meniscus. Am J Sports Med 2017;45:570-7. [Google Scholar]
- 19.Zhang P, Zhao Q, Shang X, Wang Y. Effect of arthroscopic resection for discoid lateral meniscus on the axial alignment of the lower limb. Int Orthop 2018;42:1897-903. [Google Scholar]
- 20.Ohnishi Y, Nakashima H, Suzuki H, Nakamura E, Sakai A, Uchida S. Arthroscopic treatment for symptomatic lateral discoid meniscus: The effects of different ages, groups and procedures on surgical outcomes. Knee 2018;25:1083-90. [Google Scholar]