Bone grafting of the defects in the patella and tibia has been shown to decrease anterior knee pain and our technique is cost-effective, as there is neither requirement for special instrumentation nor requirement for allograft or bone substitutes, as we have used the bone generated during the procedure itself.
Dr. M L V Sai Krishna, Department of Orthopaedics, All India Institute of Medical Sciences, New Delhi, India. E-mail: krishna.mlv.sai@gmail.com
Introduction: The anterior knee pain is the most common post-operative complaint associated with anterior cruciate ligament reconstruction (ACLR) using bone patellar tendon bone graft. It has been attributed to various factors such as loss of terminal extension, infrapatellar branch neuroma, and also due to the bone harvest site defect itself. Bone grafting of the defects in the patella and tibia has been shown to decrease anterior knee pain. At the same time, it also prevents post-operative stress fractures.
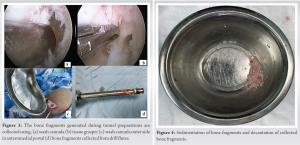
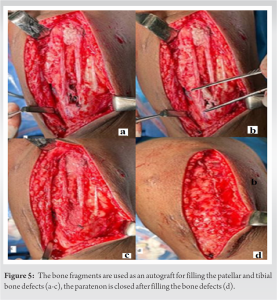
Surgical Technique: Numerous bone pieces were produced in the knee joint as a result of the drilling during ACL reconstruction. Using a wash cannula and tissue grasper, all the bone fragments were gathered into a kidney tray. The bony fragments with the saline which were collected in the metal container were allowed to sediment at the bottom. The bone that was sedimented in the metal container was collected by decantation and placed into the bony defects of the patellar and tibial sides.
Conclusion: Bone grafting of the defects in the patella and tibia has been shown to decrease anterior knee pain. Our technique is cost-effective as there is no requirement for special instrumentation like coring reamers, and no requirement for allograft or bone substitutes. Second, there is no morbidity associated with autografts harvested from elsewhere, we used the bone generated during the ACLR itself.
Keywords: Anterior cruciate ligament reconstruction, bone patellar tendon bone graft, anterior knee pain, bone graft.
One of the most frequent sports injuries to the knee is the anterior cruciate ligament (ACL) tear, which is best treated by ACL reconstruction (ACLR) [1]. Hamstring and bone-patellar tendon bone (BPTB) are the most often utilized grafts for ACLR. BPTB is a graft of choice for athletes and heavy laborers because of its high strength, stiffness, graft size consistency, early incorporation of bone to bone, and solid fixation. The problems of anterior knee pain and stress fractures at the bony harvest site are often reported with BPTB grafts. Patients who underwent ACLR using hamstrings can also experience anterior knee pain as a harvest site morbidity, though less frequently [2, 3]. To reduce the harvest site morbidities in BPTB ACLR, many surgical approaches including the mini-incision technique, double incision technique, and mobile window technique have been described [2, 3, 4]. However, leaving the bone defects after the BPTB harvest unaddressed has also been attributed to be a source of anterior knee pain, along with post-operative patellar stress fractures [4, 5, 6, 7]. Hence, bone grafting of the bone defects has been advocated to mitigate its donor site morbidity [5, 6, 7]. We have described a method to graft the bony defects created during the harvest of BPTB using autologous bone from the bone tunnels.
The patient was operated in a supine position under regional anesthesia with a tourniquet over the proximal thigh. To confirm an ACL tear, we performed a diagnostic arthroscopy after cleaning and draping the surgical site. Once the tear is confirmed, we proceeded with graft harvesting. We used an oblique linear skin incision from the center of the patella to the proximal medial tibia till the tibial tuberosity. After the skin incision, the subcutaneous tissue was dissected in line with the skin incision. The paratenon was incised in line with the patellar tendon and is elevated both medially and laterally exposing the patellar tendon in its entire length and width. A 10 mm wide patella tendon was harvested along with 10*20 mm bone plugs from the patella and tibia (Fig. 1a).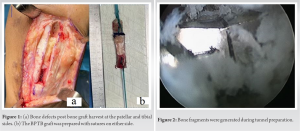
Jones was the first to suggest using the central one-third of the patellar tendon with bone plugs on either end as a graft of choice for ACLR [1]. Despite its rigid bone-to-bone healing, the usage of alternative grafts like hamstrings has been on the rise. This is mostly due to the graft site morbidities of BPTB graft such as anterior knee pain and rarely patellar fracture [2]. The anterior knee pain is the most common donor site morbidity. The reasons described in the literature are the loss of terminal extension and injury to the infrapatellar branch of the saphenous [2, 3]. Although hamstrings and BPTB ACLR patients can both experience donor site morbidity due to anterior knee pain, the incidence is not the same. Its incidence at 2-year follow-up is only 6% of hamstring ACLR whereas it is 31% in patients who underwent BPTB ACLR [3]. The bony defect itself is another factor contributing to anterior knee pain during BPTB ACLR [4]. Various techniques have been advised to avoid donor site morbidity in BPTB ACLR patients. These include using various modifications in skin incisions, closure of paratenon, and bone grafting of the harvested bony defects [5, 6, 7]. Patients who have had BPTB ACLR have a post-operative patellar fracture rate that ranges from 0.35 to 1.8%. It takes 2–6 years postoperatively for the defect to ossify when it was left without filling [8]. This can also be prevented by bone grafting the patellar bony defect [2, 7, 8]. The other benefit of bone grafting the patellar bony defect is to prevent the step-off due to a defect that may cause the soft tissue to roll into it and cause pain [7]. The development of bony spurs, which can cause pain if the defect is left unfilled, can be avoided by bone grafting or filling the defects with bony substitutes [7, 8, 9]. The incidence of anterior knee discomfort is reduced when the bone defects are filled, compared to non-grafted patients, according to the literature and systematic reviews [2, 6, 8]. For filling the bony defects after the BPTB graft harvest, various materials have been used. They consist of bone grafts and their alternatives. Coring the cancellous bone from the proximal tibia, curettage of the cancellous bone from the tibial tubercle defect, and the use of specialized equipment like coring reamers during tunnel preparation can all be used to acquire the bone graft [2, 6, 7]. To promote bone healing, fillers such as hydroxyapatite and their mixtures with bioactive glass and beta-tricalcium phosphate have also been employed in the graft harvest sites [6, 9]. The price of the surgery is increased by the use of artificial bone replacements and specialized equipment for harvesting grafts. The morbidity and duration of the treatment are further increased by removing additional cancellous bone from the proximal tibia. During the ACLR, several bone fragments are produced that can be used as a bone graft. These are produced during notchplasty and the reaming of the femoral and tibial tunnels. Using these bone fragments for filling the tibia and patella defects avoids wastage of bone autograft, the morbidity of bone graft harvesting from another site, the use of allografts or bone substitutes, and the need for any special coring instruments. In most cases, the bone fragments gathered are enough to fill the patella and tibia donor sites. If it is insufficient for both sites, the patella donor site is given priority to fill it while the tibial site is only half filled. Over drilling, the femoral tunnel by 5 mm in length can overcome the problem of inadequate bone graft without any significant morbidity.
Bone grafting of the defects in the patella and tibia has been shown to decrease anterior knee pain. Our technique is cost-effective as there is no requirement for special instrumentation like coring reamers, and no requirement for allograft or bone substitutes. Second, there is no morbidity associated with autografts harvested from elsewhere, we used the bone generated during the ACLR itself.
Without the use of any specialized equipment, bone substitutes, or bone harvesting from another location, we present our surgical technique for grafting bony deficiencies using the bony fragments produced during the drilling of bone tunnels. We have not observed any significant donor site pain or tenderness in the medium and long-term. All our patients were able to squat and kneel for social and religious reasons.
References
- 1.Koh E, Oe K, Takemura S, Iida H. Anterior cruciate ligament reconstruction using a bone-patellar tendon-bone autograft to avoid harvest-site morbidity in knee arthroscopy. Arthrosc Tech 2015;4:e179-84. [Google Scholar]
- 2.Ferrari JD, Bach BR Jr. Bone graft procurement for patellar defect grafting in anterior cruciate ligament reconstruction. Arthroscopy 1998;14:543-5. [Google Scholar]
- 3.Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy 2001;17:971-80. [Google Scholar]
- 4.Janani G, Suresh P, Prakash A, Parthiban J, Anand K, Arumugam S. Anterior knee pain in ACL reconstruction with BPTB graft-Is it a myth? Comparative outcome analysis with hamstring graft in 1,250 patients. J Orthop 2020;22:408-13. [Google Scholar]
- 5.Hacken BA, Keyt LK, Leland DP, LaPrade MD, Camp CL, Levy BA, et al. A novel scoring instrument to assess donor site morbidity after anterior cruciate ligament reconstruction with a patellar tendon autograft at 2-year follow-up using contemporary graft-harvesting techniques. Orthop J Sports Med 2020;8:2325967120925482. [Google Scholar]
- 6.Dhanakodi N, Thilak J, Varghese J, Menon KV, Varma H, Tripathy SK. Ceramic bone graft substitutes do not reduce donor-site morbidity in ACL reconstruction surgeries: A pilot study. SICOT J 2019;5:14. [Google Scholar]
- 7.Tsuda E, Okamura Y, Ishibashi Y, Otsuka H, Toh S. Techniques for reducing anterior knee symptoms after anterior cruciate ligament reconstruction using a bone-patellar tendon-bone autograft. Am J Sports Med 2001;29:450-6. [Google Scholar]
- 8.Lameire DL, Khalik HA, Zakharia A, Kay J, Almasri M, de Sa D. Bone grafting the patellar defect after bone-patellar tendon-bone anterior cruciate ligament reconstruction decreases anterior knee morbidity: A systematic review. Arthroscopy 2021;37:2361-76.e1. [Google Scholar]
- 9.Kato Y, Chavez J, Yamada S, Hattori S, Takazawa S, Ohuchi H. Beta-tricalcium phosphate block for donor site morbidity of the patella in anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft. Knee Surg Relat Res 2019;31:113-9. [Google Scholar]