Intraprosthetic dislocation (IPD) is a rare and unique complication associated with dual mobility-total hip arthroplasty, and therefore, one needs to keep a high index of suspicion to diagnose and manage it accordingly.
Dr. Mohan Desai, Department of Orthopaedics, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India. E-mail: md1964@gmail.com
Introduction: First introduced in Europe in the 1970s, dual mobility total hip arthroplasty (DM-THA) has gained popularity over years due to the reduced dislocation rates compared to standard THA. However, intraprosthetic dislocation (IPD), a rare complication where the femoral head separates from the polyethylene (PE) liner, remains a potential complication.
Case Report: A 67-year-old female presented with a transcervical neck of femur fracture. She was managed with a DM-THA. She dislocated her THA on post-operative day 18. Closed reduction was performed for the same under general anesthesia. However, she again dislocated her hip 2 days later. CT scan was done and an IPD was diagnosed. The PE liner was revised and the patient had a good outcome at 1 year follow-up.
Conclusion: When a DM-THA dislocates, it is important to consider the possibility of IPD which is a rare but unique complication associated with these systems. The recommended treatment for IPD is open reduction and replacement of the PE liner.
Keywords: Dual mobility, total hip arthroplasty, dislocation, intraprosthetic dislocation.
The rates of dislocation in primary total hip arthroplasty (THA) on 1 year follow-up range from 2% to as high as 10% [1]. On the other hand, these rates are 0.9% in Dual Mobility THA (DM-THA) explaining the increase in their popularity over years [2]. However, intraprosthetic dislocation (IPD) is a complication unique to the Dual Mobility System. Not only is it rare and not reported much, it can be difficult to diagnose on radiographs and can be easily missed. We present a case through which we wish to emphasize that dislocation of dual mobility system should raise the suspicion of an IPD and closed reduction of the same should be avoided.
A 67-year-old female presented to the outpatient department with alleged history of fall and acute pain in the right hip. She was diagnosed with a right-sided transcervical neck of femur fracture and was admitted to the hospital (Fig. 1). 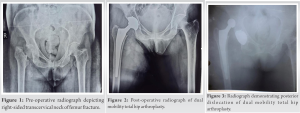

Dual Mobility Total Hip Replacements were first introduced in Europe in 1974 and subsequently in USA in 2009 [3]. It combines the advantages of small articulation to reduce wear with large articulation to minimize instability. Although DM has been effective in reducing the rates of dislocation after total hip replacements and has had a good long term record [4], IPD remains a rare unique complication. The separation of femoral head from the PE liner is called IPD. In the previous generations of DM designs, the primary cause of IPD was PE wear. Poor quality of ultra-high molecular weight PE and poorly designed femoral necks such as skirted neck and rough neck surfaces can accelerate PE [5]. The newer generations of DM have overcome these shortcomings which have reduced the rates of IPD. Nevertheless, extrinsic etiologies can still lead to IPD s even in the newer designs [6]. A long-term study with 17-year follow-up of the older generation DM by Philippot et al. showed a rate of 5.3% IPD [4]. A newer design of DM was developed in 2000 with an improved mechanism for head retention in the PE liner. It also had a smooth and tapered neck and improved coating on the acetabular shell [5, 6]. Epinette et al. [7] conducted a study on the newer generation of DM and reported 97.5 % survivorship at 5 years without any case of IPD or dislocation. De Martino et al. [8] found that a majority of the early cases of IPD occurred following a failed attempt at closed reduction. The likely cause of this was determined to be the “bottle-opener effect,” which occurs when the outer PE liner of the prosthesis becomes engaged on the rim of the acetabular cup or pelvic bone during closed reduction attempts. In addition, Addona et al. [9] reported a high rate of IPD (71%) after closed reduction, all of which required revision surgery. Furthermore, all instances of IPD occurred under conscious sedation with propofol, leading the researchers to suggest that general or regional anesthesia with complete paralysis may reduce the risk of IPD. In almost all studies, IPD has occurred with a femoral head size of 28 mm. There is only one case report by Payapapnon et al. [10], which describes IPD with a 22.2 mm femoral head. We used a femoral head size of 26 mm in our patient who sustained the IPD, which, to the best of our knowledge, has not been reported in the literature. IPDs can easily be missed on radiographs and need a high degree of clinical suspicion for diagnosis. Subtle signs in the form of femoral head being eccentrically placed within the acetabular shell must be recognized (Fig. 4). Moreover, the dislocated outer PE liner in the extra-articular soft tissue is seen on the plain radiograph as a “bubble sign” (Fig. 4). Recognizing an IPD immediately is important as surgical intervention is needed to manage this rare complication. A CT scan may be performed to confirm the diagnosis. In our case, the IPD most probably occurred during the attempted closed reduction of the DM-THA and the diagnosis was missed. It was only after the second episode of dislocation, did we realize that maybe the hip was never reduced after the initial attempted reduction.
The management of the IPD involves open reduction and revision of the DM bearing. Correcting the primary cause of the DM-THR dislocation is the key to successful management and prevention of IPD.
Closed reduction must be avoided in a dislocated DM-THA as it can lead to an IPD. However, when an IPD is diagnosed, it must be managed by open reduction and change of PE liner.
References
- 1.De Martino I, D’Apolito R, Soranoglou VG, Poultsides LA, Sculco PK, Sculco TP. Dislocation following total hip arthroplasty using dual mobility acetabular components: A systematic review. Bone Joint J 2017;99:18-24. [Google Scholar]
- 2.Dargel J, Oppermann J, Brüggemann GP, Eysel P. Dislocation following total hip replacement. Dtsch Arztebl Int 2014;111:884-90. [Google Scholar]
- 3.Bousquet G, Argenson C, Godeneche JL, Cisterne JP, Gazielly DF, Girardin P, et al. Recovery after aseptic loosening of cemented total hip arthroplasties with Bousquet’s cementless prosthesis. Apropos of 136 cases. Rev Chir Orthop Reparatrice Appar Mot 1986;72 Suppl 2:70-4. [Google Scholar]
- 4.Philippot R, Neri T, Boyer B, Viard B, Farizon F. Bousquet dual mobility socket for patient under fifty years old. More than twenty year follow-up of one hundred and thirty one hips. Int Orthop 2017;41:589-94. [Google Scholar]
- 5.Blakeney WG, Epinette JA, Vendittoli PA. Dual mobility total hip arthroplasty: Should everyone get one? EFORT Open Rev 2019;4:541-7. [Google Scholar]
- 6.Epinette JA, Beracassat R, Tracol P, Pagazani G, Vandenbussche E. Are modern dual mobility cups a valuable option in reducing instability after primary hip arthroplasty, even in younger patients? J Arthroplasty 2014;29:1323-8. [Google Scholar]
- 7.Epinette JA, Harwin SF, Rowan FE, Tracol P, Mont MA, Chughtai M, et al. Early experience with dual mobility acetabular systems featuring highly cross-linked polyethylene liners for primary hip arthroplasty in patients under fifty five years of age: An international multi-centre preliminary study. Int Orthop 2017;41:543-50. [Google Scholar]
- 8.De Martino I, D’Apolito R, Waddell BS, McLawhorn AS, Sculco PK, Sculco TP, et al. Early intraprosthetic dislocation in dual-mobility implants: A systematic review. Arthroplast Today 2017;3: 197-202. [Google Scholar]
- 9.Addona JL, Gu A, De Martino I, Malahias MA, Sculco TP, Sculco PK. High rate of early intraprosthetic dislocations of dual mobility implants: A single surgeon series primary and revision total hip replacements. J Arthroplasty 2019;34:2793-8. [Google Scholar]
- 10.Payapapnon P, Ruangsomboon P, Narkbunnam R, Chareancholvanich K, Pornrattanamaneewong C. Early intraprosthetic dislocation after closed reduction in modern dual-mobility total hip arthroplasty. Arthroplast Today 2022;13:89-92. [Google Scholar]











