Healthcare professionals must possess knowledge about the common accessory ossicles in the foot and ankle to avoid misdiagnosis and ensure proper treatment of related conditions.
Dr. Sudhir Shankar Mane, Department of Orthopaedics, S.V.S. Medical College, Mahabubnagar - 509 002, Telangana, India. E-mail: sdhrmane@gmail.com
Introduction: Accessory ossicles are well-corticated bony structures found close to bones or a joint. They may be unilateral or bilateral. The os tibiale externum is also known as accessory navicular bone, os naviculare secundarium, accessory (tarsal) scaphoid, or prehallux. It is found within the tibialis posterior tendon near its insertion on the navicular bone. The os peroneum is a small sesamoid bone located within the peroneus longus tendon, adjacent to the cuboid. We present a case series of five patients with accessory ossicles of the foot to demonstrate pitfalls in the diagnosis of foot and ankle pain.
Case Report: The case series includes four patients with os tibiale externum and one patient with os peroneum. Only one patient had symptoms related to os tibiale externum. The accessory ossicle in the rest of the cases was discovered incidentally after trauma to the ankle or foot. The symptomatic os tibiale externum was managed conservatively with analgesics and shoe inserts for medial arch support.
Conclusion: Accessory ossicles are considered developmental anomalies and they originate from ossification centers that have failed to fuse with the main bone. Clinical suspicion and awareness about the existence of the commonly occurring accessory ossicles of the foot and ankle are necessary. They can be a confounding factor in the diagnosis of foot and ankle pain. Failure to notice their presence might result in a misdiagnosis and unnecessary immobilization or surgery for the patients.
Keywords: Accessory ossicles, os tibiale externum, os peroneum.
Several accessory bones or ossicles have been described around the foot and ankle. Accessory ossicles are well-corticated bony structures found close to bones or a joint. They result from unfused ossification centers and are frequently congenital [1]. O’Rahilly, in his definition of accessory ossicles, stated that they should be “inconsistent, independent, and well-defined bones in an otherwise normally developed foot” [2]. They may be unilateral or bilateral. After trauma, asymptomatic ossicles may become symptomatic due to secondary loosening [3]. Failure to notice their presence might result in a misdiagnosis and unnecessary immobilization or surgery for the patients. The os tibiale externum is also known as accessory navicular bone, os naviculare secundarium, accessory (tarsal) scaphoid, or prehallux. It is found within the tibialis posterior tendon near its insertion on the navicular bone. It was first described by Caspar Bauhin in 1605. It is the second most common accessory ossicle with a prevalence of 2–21% [4]. The os peroneum is a small sesamoid bone located within the peroneus longus tendon, adjacent to the cuboid. Anatomic and radiographic studies have identified an os peroneum in 5–26% of the population [5]. We present a case series of five patients with accessory ossicles of the foot. Four patients had an os tibiale externum, of which only one was symptomatic. One patient had an asymptomatic os peroneum. The asymptomatic ossicles were discovered incidentally during routine imaging after an injury to the foot or ankle.
Case 1
A 28-year-old man presented to the out-patient clinic with a complaint of pain in the left foot for 1 day after a sprain while exercising in the gym. The pain was aggravated by bearing weight and relieved by taking rest. On examination, there was swelling over the medial aspect of the ankle and dorsum of the foot, but there was no bony tenderness, crepitus, or any abnormal mobility. Radiographs of the left ankle in anteroposterior (AP) and lateral views were normal. Radiographs of the left foot in AP (Fig. 1a) and oblique views (Fig. 1b) revealed a well-corticated bony structure on the medial aspect of the navicular bone which was diagnosed as an os tibiale externum.  The patient was prescribed analgesics and advised limb elevation and rest until the symptoms subsided. The patient was able to return to his regular activities after 5 days.
The patient was prescribed analgesics and advised limb elevation and rest until the symptoms subsided. The patient was able to return to his regular activities after 5 days.
Case 2
A 24-year-old man presented to the outpatient clinic with a complaint of pain in the right foot for 3 days after a sprain while running. The symptoms and examination findings were similar to Case 1. Radiographs of the right ankle in AP and lateral views were normal. Radiographs of the right foot in AP (Fig. 2a) and oblique views (Fig. 2b) revealed an os tibiale externum. The patient was prescribed analgesics and advised rest and limb elevation. Recovery was uneventful and the patient was able to return to his regular activities.
Case 3
A 28-year-old man presented to the outpatient clinic with a complaint of pain in the right foot for 10 days after a sprain while playing kabaddi. The symptoms and examination findings were similar to Cases 1 and 2. Radiographs of the right ankle in AP and lateral views were normal. Radiographs of the right foot in AP (Fig. 3a) and oblique views (Fig. 3b) revealed an os tibiale externum. The patient was prescribed analgesics and medial arch support with shoe insoles. There was significant improvement after treatment.
Case 4
An 11-year-old girl presented to the out-patient clinic with a complaint of pain in both the feet for 1 year. The pain was aggravated by running and walking for long distances and relieved by taking analgesics. There was no history of any trauma, fever, or weight loss. Physical examination of both the feet and ankle joints was normal. Radiographs of bilateral ankle joints in AP and lateral views were normal. Radiographs of both the feet in AP (Fig. 4a) and oblique views (Fig. 4b) revealed an os tibiale externum on both sides. The patient was prescribed analgesics and orthotic shoes. The patient showed improvement in symptoms at the follow-up visit after 3 months.
Case 5
A 56-year-old man presented to the emergency room with a complaint of pain and swelling in the left ankle after he was hit by a slow-moving motorcycle while walking on the road. Radiographs of the left foot and ankle were taken in AP and lateral views. A diagnosis of an undisplaced lateral malleolus fracture was made. A bean-shaped and well-corticated ossified mass was also noted close to the calcaneocuboid joint on the AP view of the left foot (Fig. 5a and Fig. 5b). There was no tenderness over the lateral aspect of the foot. Initially, the bony mass was assumed to be a bony fragment of the lateral malleolus. However, after careful examination, a diagnosis of os peroneum was made. A below-knee fiberglass cast was applied for 6 weeks. The fracture united well and the patient had no pain in the lateral aspect of the foot at follow-up.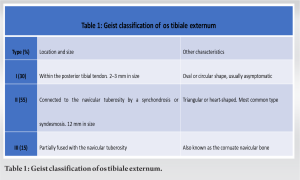
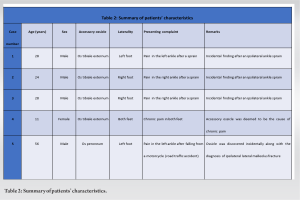
We report on a case series of five patients with accessory ossicles in the foot, consisting of four cases of os tibiale externum and one case of os peroneum (Table 2). Except for one patient (case 4), the accessory ossicles in the rest of the cases were asymptomatic and were incidental findings. Accessory ossicles are considered developmental anomalies [6] and they originate from ossification centers that have failed to fuse with the main bone [7,8]. The accessory ossicle forms a fibrous or cartilaginous junction with the parent bone; very rarely, a synovial cavity may be present [9]. It is critical to recognize the presence of these ossicles because they can be a significant contributor to a patient’s symptoms.
Os tibiale externum
A morphological classification of os tibiale externum was published in 1914 by Geist, identifying three types (Table 1). Genetic influence [10] and an autosomal inheritance have been suggested as etiological factors [11] by few researchers. It has also been suggested that it may resemble a vestige of a supernumerary 6th ray (prehallux), a modern os tibiale, or an os centrale found in amphibians, hence its Latin name ‘os tibiale externum’ [12]. The presence of this ossicle may also be associated with flat feet though none of the patients in our case series had flat feet. Conservative treatment options include wearing wide shoes with medial arch support, short-term immobilization, analgesics, and local corticosteroid injections. Operative management is indicated when conservative methods fail. The various surgical options include Kidner’s procedure (surgical excision with fixation of the posterior tibial tendon to the navicular) and augmented Kidner’s procedure (fusion of the os tibiale externum to the navicular body with a screw). In the presence of severe flat foot, other procedures such as transfer of the flexor digitorum longus tendon, arthroereisis, osteotomies, and midfoot fusions may be indicated [12].
Os peroneum
The os peroneum is embedded in the peroneus longus tendon and its origin is a point of contention; embryonic development of the ossicle [13] and development from a stress response have been advocated [14]. The os peroneum can be visualized as an oval, well-corticated ossicle located close to the calcaneocuboid joint. It is bean-shaped and has one or two concave articular surfaces. A bipartite bone is common and can be seen in around 30% of cases [15]. The os peroneum is usually asymptomatic. It may be a cause of lateral midfoot pain in some individuals. This condition is often underdiagnosed and overlooked by clinicians. Painful os peroneum syndrome can be due to fracture or degeneration of the ossicle within the tendon. It can result in a tear of the peroneus longus tendon. This condition can be diagnosed using magnetic resonance imaging or ultrasonography. It can be managed conservatively with analgesics or the use of a walking boot. Surgical options include fixation of the fractured os peroneum, excision of the ossicle with the repair of the peroneus longus tendon, and tenodesis of the peroneus longus to the peroneus brevis. Due to its location on the lateral aspect of the midfoot and its location within the peroneal tendons, the presence of an os peroneum is also a differential diagnosis for os vesalianum. The os vesalianum is an accessory ossicle of the foot that is found within the peroneus brevis tendon, proximal to the base of the fifth metatarsal and lateral to the cuboid bone, and forms an articulation with it. Physiotherapy can be used to address underlying foot and ankle muscle imbalances and to improve range of motion, function, and reduce pain in most patients. Orthotics can provide support and correct biomechanical abnormalities, especially in the case of os tibiale externum which is associated with flat foot. Insoles can cushion, support, and redistribute pressure away from the symptomatic area and are a less expensive and invasive option than custom orthotics. They can be used with other conservative measures, such as rest and physical therapy, to improve outcomes. While research is limited, insoles are generally considered safe and effective for foot and ankle pain. Surgery may be considered for patients with chronic pain, failure of conservative treatment, and the presence of a large or symptomatic accessory ossicle, confirmed by imaging studies. The decision to proceed with surgery should be based on individualized treatment, taking into account the patient’s symptoms, age, activity level, and overall health. Surgical approaches may involve excision or fixation of the bone in place to prevent movement and subsequent irritation.
Clinical suspicion and awareness about the existence of the commonly occurring accessory ossicles of the foot and ankle are necessary. They can be a confounding factor in the diagnosis of foot and ankle pain. Inadequate knowledge about these accessory ossicles may lead to wrong treatment including unnecessary immobilization or surgical intervention.
In summary, accessory bones in the foot and ankle are often discovered unexpectedly when imaging is done following an injury. Although they generally do not cause any noticeable symptoms, doctors need to be aware of their presence so they can accurately diagnose any related conditions. Failure to recognize these bones can lead to incorrect treatment, highlighting the importance of understanding, and identifying these structures in clinical practice.
References
- 1.Vora BM, Wong BS. Common accessory ossicles of the foot: Imaging features, pitfalls and associated pathology. Singapore Med J 2018;59:183-9. [Google Scholar | PubMed]
- 2.O’Rahilly R. A survey of carpal and tarsal anomalies. J Bone Joint Surg Am 1953;35-A:626-42. [Google Scholar | PubMed]
- 3.Rammelt S, Manke E. Symptomatisches os vesalianum. FussSprungg 2019;17:103-12. [Google Scholar | PubMed]
- 4.Nwawka OK, Hayashi D, Diaz LE, Goud AR, Arndt WF 3rd, Roemer FW, et al. Sesamoids and accessory ossicles of the foot: Anatomical variability and related pathology. Insights Imaging 2013;4:581-93. [Google Scholar | PubMed]
- 5.Smith JT, Johnson AH, Heckman JD. Nonoperative treatment of an os peroneum fracture in a high-level athlete: A case report. Clin Orthop Relat Res 2011;469:1498-501. [Google Scholar | PubMed]
- 6.Kalbouneh H, Alajoulin O, Shawaqfeh J, Mustafa A, Jaber S, Zaben S, et al. Accessory ossicles in the region of the foot and ankle: An epidemiologic survey in a Jordanian population. Medicina (Kaunas) 2021;57:1178. [Google Scholar | PubMed]
- 7.Li X, Shi L, Liu T, Wang L. Progress in the clinical imaging research of bone diseases on ankle and foot sesamoid bones and accessory ossicles. Intractable Rare Dis Res 2012;1:122-8. [Google Scholar | PubMed]
- 8.Chan BY, Markhardt BK, Williams KL, Kanarek AA, Ross AB. Os conundrum: Identifying symptomatic sesamoids and accessory ossicles of the foot. AJR Am J Roentgenol 2019;213:417-26. [Google Scholar | PubMed]
- 9.Jain AK. Turek’s Orthopaedics: Principles and their Applications. 7th ed., Vol. 2. Gurgaon, India: Wolters Kluwer; 2016. [Google Scholar | PubMed]
- 10.Cheong IY, Kang HJ, Ko H, Sung J, Song YM, Hwang JH. Genetic influence on accessory navicular bone in the foot: A Korean twin and family study. Twin Res Hum Genet 2017;20:236-41. [Google Scholar | PubMed]
- 11.Choi YS, Lee KT, Kang HS, Kim EK. MR imaging findings of painful Type II accessory navicular bone: Correlation with surgical and pathologic studies. Korean J Radiol 2004;5:274-9. [Google Scholar | PubMed]
- 12.Rammelt S, Sands AK. The accessory navicular and its association with flatfoot. FussSprungg 2020;18:60-71. [Google Scholar | PubMed]
- 13.Guimerá V, Lafuente A, Zambrana L, Rodriguez-Niedenführ M, Sañudo JR, Vazquez T. The peroneocuboid joint: Morphogenesis and anatomical study. J Anat 2015;226:104-12. [Google Scholar | PubMed]
- 14.Sobel M, Pavlov H, Geppert MJ, Thompson FM, DiCarlo EF, Davis WH. Painful os peroneum syndrome: A spectrum of conditions responsible for plantar lateral foot pain. Foot Ankle Int 1994;15:112-24. [Google Scholar | PubMed]
- 15.Bianchi S, Bortolotto C, Draghi F. Os peroneum imaging: Normal appearance and pathological findings. Insights Imaging 2017;8:59-68. [Google Scholar | PubMed]







