Scapula fracture should be suspected in a patient with insidious development of shoulder pain with restricted movements following a seizure episode and surgical intervention when indicated with a deliberate planning and execution can provide excellent outcomes.
Dr. Amir Ratna Shakya, Department of Orthopaedics, Shree Birendra Hospital, Chhauni, Kathmandu, Nepal. E-mail: anmishakya@hotmail.com
Introduction: Scapula fractures are very rare and bilateral reciprocal involvement is rarest of all. Due to the protective nature of surrounding musculature, it is least prone to fracture with reported incidence of 1% of all skeletal fractures. However, synchronized firing of the periscapular muscles could overcome the bone strength resulting into the fracture as in the cases of electrocution and seizure attack.
Case Report: We present a case of 54-year-old ex-military male patient with a history of acute onset seizure of multiple episodes. Magnetic resonance imaging showed cerebrovascular thrombosis. The patient was admitted in the intensive care and complained pain over bilateral shoulder with restricted movement in the post-ictal phase. X-ray showed bilateral comminuted extra-articular scapular fractures. The severity of the injury and displacement of the fracture pronounced operative intervention. Modified Judet approach was used to approach the fractures. After a successful surgery, rehabilitation protocol constituted of passive range of motion exercises with gradual active exercises of shoulder. One-year follow-up showed good consolidation of both fracture with full recovery of function.
Conclusion: Periscapular musculature protects the scapula from traumatic events due to the significant bulk that it provides but these can on the other hand be source of deforming force in the patient who has history of simultaneous contraction as in the case of recurrent episodic seizure or electrocution. Scapular fracture should always be suspected in the patient with insidious development of shoulder pain following strong seizure attack. These fractures if indicated should be managed operatively.
Keywords: Scapula, non-traumatic, fracture, seizure.
Scapula fracture consists of only 1% of all skeletal fracture and bilateral scapula fracture is even rarest of all. High-velocity trauma like road traffic injury with injury to the shoulder is the most common cause for the scapula fracture. Scapula is shielded from traumatic sources due to the surrounding bulky musculature. Atraumatic presentation of scapula fractures is reported in the literature following seizure or electrocution, but non-traumatic bilateral and reciprocal scapular fractures is extremely rare occurrence. We report a case of bilateral reciprocal scapula fracture, who was managed surgically and had an uneventful and near-complete functional recovery.
A 54-year-old retired military professional, known hypertensive controlled on medication with recent history of recovered COVID-19 infection, presented in the emergency department with history of recurrent generalized tonic-clonic seizure thrice in a span of 8 h. Further, evaluation showed features of cerebrovascular thrombosis on magnetic resonance imaging. The patient was admitted in the intensive care for further management, where he started appreciating pain over both the shoulder on next day with restricted movement. No such symptoms were appreciated in the interim period between the seizures. 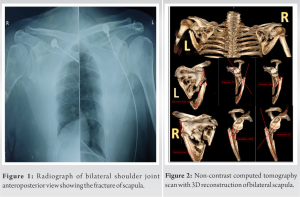
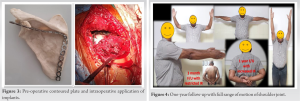
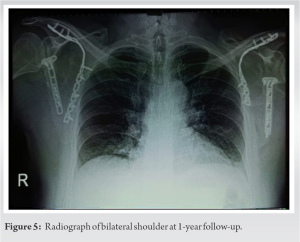
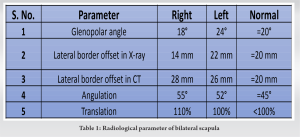
Scapula fracture is one of rarest skeletal injury accounting about 2–3% of the fracture of shoulder girdle and only 1% of fracture of overall skeletal fractures [1]. Literature describes two mechanism of scapula fracture: Direct injury or indirect injury. Former being direct impact to the scapula whereas latter occurs due to transmission of forces to the scapula during falls through axial forces from the hand resulting to glenoid region fracture [2]. Authors have reported vigorous contraction of scapular musculature following the electrocution or an episode of seizure as common cause for the non-traumatic bilateral scapula fracture with very few cases reported so far [3]. Most of these patients were managed conservatively. Seizures patients are at risk for injuries which may be due to direct forceful contraction of musculature or indirectly due to fall following the episode [4]. Grzonka et al. reported in his systemic review of 34 case reports of fractures resulting from seizures; the most common being bilateral posterior fracture–dislocations of the shoulders followed by thoracic and lumbar vertebral compression fractures with only one case of bilateral scapula fracture [5]. Tuček et al. did a review of 17 patients with bilateral scapular fractures of which six patients had muscle spasm; out of them two were due to seizure and four were secondary to electrical shock [6]. Scapula fracture is one of the most difficult fractures to be diagnosed in normal radiograph due to rib bones interface and it may be initially overlooked [7]. Three-dimensional computed tomographic scan is considered as gold standard tool [8]. Various measurement tools are required to decide upon conservative management and surgical fixation to prevent shortening and medialization of scapular body and to improve quality of life and shoulder function . Scapula fractures are broadly classified according to the region involved like body, neck, glenoid, acromion, and coracoid. Although classification system exists for others, none exists for body fractures. The management of scapula body fracture is dictated by the amount of displacement of the fragments. Our case had sustained a bilateral extra-articular fracture of the body with increase in lateral border offset of more than 20 mm with angulation of fragment of more than 45° and translation of more than 100% with increased glenopolar angle demanding surgical management to prevent shortening and medialization of scapular body (Table 1). Literature supports non-operative management for most of the scapula fracture and due to large muscle bulk, healing is decent [10]. Malunion after non-operative treatment of a displaced scapula fracture has been shown to be associated with poor functional and cosmetic outcomes [11]. The severity of the injury and displacement of the fracture in our patient mandated operative intervention. We did a thorough literature search, and we believe our case to be first of non-traumatic reciprocal scapula fracture to undergo operative management for both sides and have excellent functional outcome. Obremskey and Lyman described the modified Judet approach with boomerang incision preserving infraspinatus attachment with reduction of fracture fragment and plating of fracture site [12]. We applied the same principle, and both the side fracture was fixed with pre contoured plate with the goal of early mobilization and full recovery with full range of motion of shoulder.
A non-traumatic reciprocal scapula fracture is an extremely rare event but can be encountered in orthopedic practice. Most of the scapular injuries are managed non-operatively, but at times, the displacement of the fragments may indicate operative intervention like in our case. A deliberate approach to such an injury shall result in favorable and excellent outcome. Our case resulted in excellent outcome after surgery and shall be a useful guide to any orthopedic surgeon under similar circumstances.
Although literature report posterior shoulder dislocation to be the most common association secondary to the seizure activities, the presence of the unilateral or bilateral scapular fractures even though unusual, should be consider as a potential orthopedic injury. When indicated for the surgery, early intervention with meticulous planning of open reduction and internal fixation can yield satisfactory outcome.
References
- 1.Blondiaux J, Fontaine C, Demondion X, Flipo RM, Colard T, Mitchell PD, et al. Bilateral fractures of the scapula: Possible archeological examples of beatings from Europe, Africa and America. Int J Paleopathol 2012;2:223-30. [Google Scholar]
- 2.Berritto D, Pinto A, Russo A, Urraro F, Laporta A, Belfiore MP, et al. Scapular fractures: A common diagnostic pitfall. Acta Biomed 2018;89 Suppl 1:102-10. [Google Scholar]
- 3.Rana M, Banerjee R. Scapular fracture after electric shock. Ann R Coll Surg Engl 2006;88:W3-4. [Google Scholar]
- 4.Betten DP, Batson IS, Babiarz LN, Owen KN. Bilateral scapular fractures occurring as a result of a first-time seizure. Case Rep Emerg Med 2022;2022:9186275. [Google Scholar]
- 5.Grzonka P, Rybitschka A, De Marchis GM, Marsch S, Sutter R. Bone fractures from generalized convulsive seizures and status epilepticus-a systematic review. Epilepsia 2019;60:996-1004. [Google Scholar]
- 6.Tuček M, Bartoníček J, Novotný P, Voldřich M. Bilateral scapular fractures in adults. Int Orthop 2013;37:659-65. [Google Scholar]
- 7.Harris RD, Harris JH Jr. The prevalence and significance of missed scapular fractures in blunt chest trauma. AJR Am J Roentgenol 1988;151:747-50. [Google Scholar]
- 8.Armitage BM, Wijdicks CA, Tarkin IS, Schroder LK, Marek DJ, Zlowodzki M, et al. Mapping of scapular fractures with three-dimensional computed tomography. J Bone Joint Surg Am 2009;91:2222-8. [Google Scholar]
- 9.Rollo G, Huri G, Meccariello L, Familiari F, Çetik RM, Cataldi C, et al. Scapular body fractures: Short-term results of surgical management with extended indications. Injury 2021;52:481-6. [Google Scholar]
- 10.Cole PA, Gauger EM, Schroder LK. Management of scapular fractures. J Am Acad Orthop Surg 2012;20:130-41. [Google Scholar]
- 11.Cole PA, Talbot M, Schroder LK, Anavian J. Extra-articular malunions of the scapula: A comparison of functional outcome before and after reconstruction. J Orthop Trauma 2011;25:649-56. [Google Scholar]
- 12.Pires RE, Giordano V, de Souza FS, Labronici PJ. Current challenges and controversies in the management of scapular fractures: A review. Patient Saf Surg 2021;15:1-18. [Google Scholar]