The Brostöm/Gould surgical technique for treatment of lateral ankle instability can be modified and the ATFL can be reattached to the talus instead of the fibula if pathological anatomical changes make the fibular anchor placement more difficult.
Miss. Dorothea Grade, Department of Paediatric Orthopaedics, Children’s Hospital of Eastern Switzerland, St. Gallen, Claudiusstrasse 6, 9000 St. Gallen, Switzerland. E-mail: dorothea.grade@kispisg.ch
Introduction: Patients with lateral instability of the ankle have a much higher prevalence of an os subfibulare compared with the general population. In children and adolescents with known os subfibulare and chronic instability of the ankle, surgical resection of the os subfibulare and the Broström/Gould procedure to reattach the ATFL to the fibula has been described if conservative therapy fails.
Case Report: Our case is about a 10-year-old girl with chronic instability of the ankle and a symptomatic os subfibulare, with additional cystic and edematous changes in the distal fibula in the MRI. Due to the reduced bone density, we assumed a higher risk of anchor pullout with the normal refixation at the distal fibula. Therefore, the surgical technique according to Broström/Gould was modified and the ATFL was refixed on the talar side.
Conclusion: In cases of symptomatic os subfibulare with clinical instability of the ankle, a Broström/Gould operation and resection of the os subfibulare is recommended after failure of conservative therapy. Our case showed that a very satisfying post-operative result can be achieved with a modification of the Broström/Gould operation, with reattachment of the ATFL to the talus instead of the fibula.
Keywords: Instability of the ankle, os subfibulare, Broström/Gould technique, ATFL.
Two different theories can be found in the literature regarding the exact origin of the os subfibulare. On the one hand, a traumatic origin is discussed in the context of bony avulsion fractures of the anterior talo-fibular ligament (ATFL). On the other hand, an accessory bone originating from a secondary ossification center is hypothesized [1, 2, 3]. The subfibulare bone can be found in a variety of shapes and sizes, with a prevalence rate ranging from 0.2% to 6.7% in the general population. In patients with lateral instability of the ankle, the prevalence is much higher with 10% to 38.5%. Therefore, a connection between chronic lateral ankle instability and the presence of a subfibulare bone is assumed [1, 2, 4]. If conservative treatment fails to respond, the common surgical procedure is a combination of the resection of the subfibulare bone and reinsertion of the ATFL with a modified Broström/Gould operation [3, 5, 6, 7, 8]. In general, the Broström/Gould operation is the first-line therapy for chronic instability of the lateral ankle. The technique of direct reattachment of the ATFL on the distal fibula was described by Broström. Gould et al. suggested additional reinforcement using a mobilized lateral extensor retinaculum [5, 9].
In 2018, the 7-year-old girl was referred to our outpatient clinic, due to recurrent left ankle sprain and pain in the lateral malleolus area. Two years before, in 2016, the patient suffered a severe supination-distortion trauma of the left ankle after another child jumped on her left foot on the trampoline. Ankle pain and instability resulted during sports and normal walking. The X-ray showed an os subfibulare, a supernumerary bone of the lateral malleolus, with no other radiological abnormalities. A conservative treatment was started with physical therapy for proprioception training and strengthening of the lateral ligaments. Initially, the symptoms improved. Three years later, she was sent again by her pediatrician due to persistent and progressive symptoms. The patient meanwhile suffered from left ankle pain during activities of daily living, for example, with normal walking and cycling. Sports were no longer possible.
Physical examination
A tenderness over the subfibulare bone, the tip of the fibula and at the ATFL on the left, was reported. In addition, there was a significant lateral instability of the left ankle with a positive anterior drawer sign. The peripheral sensorimotor function and blood circulation were intact.
Diagnosis
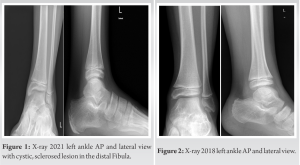
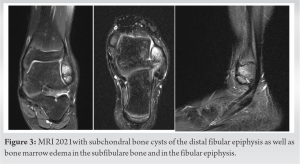
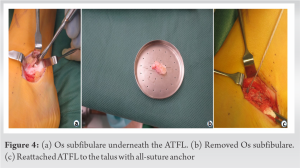
The X-ray (left ankle, AP and lateral view, standing) showed the os subfibulare and an otherwise normal upper ankle joint (Fig. 1). Meanwhile, compared to the X-rays from 2018 (Fig. 2), there was a marked cystic, sclerosed lesion in the marginal portion of the distal fibular epiphysis adjacent to the os subfibulare. In addition, subchondral bone cysts of the distal fibular epiphysis as well as bone marrow edema in the subfibulare bone and in the fibular epiphysis were found in magnetic resonance imaging of the left upper ankle. The lateral ligaments were elongated and the ATFL was attached to the os subfibulare (Fig. 3).
Further course and therapy
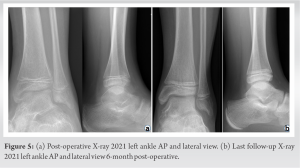
As in 2018, we first started again with a conservative treatment. We advised her to do without sports and to wear an ankle brace for 6 weeks. We reinstalled the physiotherapy for strengthening of the musculature and proprioception training. The patient was then seen in our outpatient clinic after 6 and 12 weeks without any improvement. Due to the lack of response to conservative management, the high level of suffering of the patient, the significant instability of the ankle and the radiological findings, the decision was made to proceed with surgical treatment. In similar cases without edema or cysts in the distal fibular epiphysis, we usually perform a resection of the os subfibulare and a Broström/Gould operation with reattachment of the ATFL to the fibula [1]. Due to the pathological changes at the desired anchor entry point in the distal fibula with suspected questionable stable fixation at the anatomically correct attachment point of the ATFL, we made the decision to reattach the ATFL to the talus instead. The operation was performed in the supine position under general anesthesia. Non-sterile thigh tourniquet was used. First, we marked the anatomical landmarks and the os subfibulare using the portable X-ray. A slightly curved incision was made from the anterior edge of the fibula in line with the ATFL in an anteroventral direction onto the talus of approximately 4 cm. The individual layers were split until the extensor retinaculum was clearly visible. We slightly detached the distal portion of the retinaculum. Next, we exposed the anterior talofibular ligament, which was intact. In the neutral position of the foot, the ATFL was elongated without tension and the lateral instability could be reproduced intraoperatively. The subfibulare bone was located underneath the ATFL (Fig. 4a). We detached the ATFL from the subfibulare bone while the attachment at the distal fibula was left intact and untouched. The subfibulare bone could be gradually removed from the ATFL in toto (Fig. 4b). We followed the ligament to the talar attachment, which was then detached. A 1.8 mm Q-Fix anchor (All-Suture Anchor; Smith and Nephew) was placed at the anatomic talar attachment point. Using the sutures form the anchor, the ATFL was reinforced in a baseball-stitch manner and secured to the anchor. This was performed in a neutral position of the ankle (0° dorsiflexion) and slight pronation of the foot putting the ATFL under moderate tension (Fig. 4c). For reinforcement, the extensor retinaculum was stretched over the ATFL with a 3.0 Vicryl suture. Finally, a layered wound closure was done. Postoperatively, the ankle was immobilized in a high walker boot for a total of 6 weeks with a partial weight-bearing of 15 kg. After 2 weeks, the foot was allowed to be carefully mobilized passively and actively-assisted from the walker boot with physiotherapy while strictly avoiding supination and forced plantar flexion movements. Six weeks after the operation, the boot was changed to a simple laced upper ankle joint orthosis, with transition to full weight-bearing. The X-ray showed complete removal of the os subfibulare (Fig. 5a). Physiotherapy was adapted to improve mobility and to gain muscle strength with proprioception and coordination training. Return to sports 3 months postoperatively was encouraged.
Six months postoperatively, the patient was completely symptom-free in activities of daily living. She no longer felt instability and had no ankle sprain since the operation. The scar was completely free of irritation. The peripheral sensorimotor function and blood circulation were intact. Mobility of the ankle was free and the anterior drawer test negative. Neither clinical nor radiological signs of persistent ankle instability were seen (Fig. 5b).
The presence of an os subfibulare is highly associated with recurrent ankle sprain and instability (10%–38.5% vs. 0.2%–6.7% in the general population) [2, 3, 5]. The first-line therapy of patients with ankle sprain is non-operative. In the 1st post-traumatic weeks, functional bracing and physiotherapy for proprioception training and strengthening of the lateral ligaments is recommended. The goal is first to improve the range of motion and to strengthen the surrounding muscles, before focusing on exercises for dynamic stability of the ankle [9, 10, 11]. Should the conservative treatment fail and the patient continue to suffer from persistent instability and pain, an operative management is indicated. The technique of direct reattachment of the ATFL to the distal fibula was described by Broström. Gould et al. suggested additional reinforcement using a mobilized lateral extensor retinaculum. This anatomic repair of the lateral ligament complex is described in the literature as the preferred method of surgical treatment, with an 85%–95% success rate [5, 6, 9]. Kubo et al. as well as Pill et al. also got excellent results with the simultaneous ossicle resection during a Broström/Gould operation [4, 8]. According to the literature, our normal operative procedure would be a resection of the os subfibulare and a Broström/Gould operation with reattachment of the ATFL to the fibula [1]. Ergün et al. describe in their review paper that different insertion sites for all-suture anchors (ASA) can result in different outcomes. These differences can be explained by different bone density at the anchor placement. Cortical bone density seems to be the main determinant of the initial fixation strength of an ASA [10]. Due to the edema and cystic changes in the distal fibula shown in the MRI of our patient, we suspected a higher risk of anchor pullout due to the reduced bone density at the insertion site. An increased risk of insufficient support in the bone for the suture anchor was postulated by the authors; therefore, the decision was made to reattach the ATFL to the talus.
In cases of symptomatic os subfibulare with clinical instability of the ankle, surgical treatment is recommended after failure of conservative therapy. First-line therapy is the removal of the os subfibulare and an operation according to Broström/Gould to address the instability. Our case showed that a very satisfying post-operative result can be achieved with a modification of the Broström/Gould operation, with reattachment of the ATFL to the talus instead of the fibula.
An os subfibulare can be associated with a higher risk of ankle instability. If conservative therapy fails, the Broström/Gould operation with removal of the os subfibulare shows excellent results. A modification of the surgical technique with reattachment of the ATFL to the talus can be considered if anchoring in the distal fibula is not possible.
References
- 1.Broström L. Sprained ankles. VI. Surgical treatment of ‘‘chronic’’ ligament ruptures. Acta Chir Scand 1966;243:551-65. [Google Scholar]
- 2.Launay F, Barrau K, Jouve JL, Petit P, Siméoni MC, Bollini G. Assessment of acute ankle sprain with os subfibulare in children. J Pediatr Orthop B. 2007 Jan;16(1):61-5. [Google Scholar]
- 3.Kim BS, Woo S, Kim JY, Park C. Radiologic findings for prediction of rehabilitation outcomes in patients with chronic symptomatic os subfibulare. Radiol Med 2017; 122:766-73. [Google Scholar]
- 4.Pill SG, Hatch M, Linton JM, Davidson RS. Chronic symptomatic os subfibulare in children. J Bone Joint Surg Am. 2013 Aug 21;95(16):e115(1-6). [Google Scholar]
- 5.Candan B, Torun E, Dikici R. The Prevalence of accessory ossicles, sesamoid bones, and biphalangism of the foot and ankle: A radiographic study. Foot Ankle Orthop 2022;7:1-10 [Google Scholar]
- 6.Ahn HW, Lee KB. Comparison of the modified broström procedure for chronic lateral ankle instability with and without subfibular ossicle. Am J Sports Med 2016; 44:3158-64. [Google Scholar]
- 7.Kocher MS, Fabricant PD, Nasreddine AY, Stenquist N, Kramer DE, Lee JT. Efficacy of the modified brostrom procedure for adolescent patients with chronic lateral ankle instability. J Pediatr Orthop 2015; 37(8):537-542. [Google Scholar]
- 8.Kubo M, Yasui Y, Sasahara J, Miki S, Kawano H, Miyamoto W. Simultaneous ossicle resection and lateral ligament repair give excellent clinical results with an early return to physical activity in pediatric and adolescent patients with chronic lateral ankle instability and os subfibulare. Knee Surg Sports Traumatol Arthrosc 2019;28:298-304. [Google Scholar]
- 9.Baumhauer JF, O’Brien T. Surgical considerations in the treatment of ankle instability. J Athl Train 2002;37:458-62. [Google Scholar]
- 10.Ergün S, Akgün U, Barber FA, Karahan M. The clinical and biomechanical performance of all-suture anchors: A systematic review. Arthrosc Sports Med Rehabil 2020;2:e263-75. [Google Scholar]
- 11.Mascaro TB, Swanson LE. Rehabilitation of the foot and ankle. Orthop Clin North Am 1994;25:147-60. [Google Scholar]