In the case of a young active patient with severe isolated bilateral patellofemoral disease with markedly compromised anatomy, robotic patellofemoral arthroplasty may offer a bone and ligament-preserving option that better maintains the natural kinematics of the knee compared to TKA.
Dr. Nicolas S Piuzzi, Department of Orthopaedic Surgery, Cleveland Clinic, Cleveland, Ohio, United States. E-mail: piuzzin@ccf.org
Introduction: Indications for patellofemoral arthroplasty (PFA) remain under debate, with many surgeons favoring total knee arthroplasty (TKA) even in patients with limited degeneration in the tibiofemoral compartments.
Case Report: A 30-year-old man with a history of bilateral patellar instability treated in youth with multiple surgeries presented with 8+ months of recurrent bilateral knee pain. Evaluation showed bilateral severe patellofemoral arthritis with preserved medial and lateral compartments. Bilateral sequential robotic-assisted PFAs (RA-PFA) were offered as a precise approach to reconstructing patellofemoral biomechanics while minimizing bone resection to avoid compromising potential future TKA. Four months after his latest surgery, he returned to a physically demanding job, and he remains active and pain free at 1 year postoperatively.
Conclusion: RA-PFA can provide less invasive, accurate, and individualized treatment for younger patients with severe disease without compromising future conversion to TKA.
Keywords: Robotic, patellofemoral arthroplasty, trochlear dysplasia, patellar instability, patellofemoral osteoarthritis.
Indications for patellofemoral arthroplasty (PFA) remain under debate, with many surgeons favoring total knee arthroplasty (TKA) even in patients with limited degeneration in the tibiofemoral compartments [1, 2, 3, 4]. In the younger patient population, PFA may represent a less invasive option that allows potential conversion to TKA if disease progress or complications arise [3, 5, 6, 7]. While early iterations of PFA showed poor long-term outcomes, advanced in implant design, patient selection, and surgical technique have shown improved performance and longevity [1, 2, 3, 7, 8, 9, 10]. However, implant positioning and soft-tissue balancing remain crucial to minimize implant mismatch and patellar maltracking [3, 11]. In the context of severely compromised anatomy, implant positioning represents a major challenge. Robotic-assisted arthroplasty allows excellent precision in implant placement and alignment, with early published results showing promising functional outcomes [11, 12, 13, 14, 15, 16].
A 30-year-old male with a history of bilateral patellar instability treated with patellar alignment and MPFL reconstruction surgeries in childhood presented with worsening bilateral knee pain and swelling for the previous 8 months.
History
His complex history began at age 5 years, when he first developed bilateral knee discomfort and episodes of patellar instability. He was managed nonoperatively until age 13. He then had multiple surgeries in the bilateral knees at an outside institution, mostly involving soft-tissue patellar realignment and debridements. At age 16 years, he underwent right knee patellar chondral shaving, patellar realignment, and patellar tendon and medial retinaculum imbrication. A year later he underwent left knee patellar chondral shaving, patellar alignment with MPFL reconstruction, lateral retinacular lengthening, and patellar tendon imbrication. Five years later, he underwent left knee lateral meniscus debridement, extensor mechanism alignment including distal femoral trochlea osteotomy, patellar tendon imbrication, and revision MPFL reconstruction. He was then seen at age 25 years where he was noted to have stable, manageable bilateral knee pain with known severe patellofemoral dysplasia. Symptoms were minimal with certain limitations in activity. Most recently, he presented at age 30 years with pain over the anterior aspect of both knees, swelling, clicking, and grinding. Pain was refractory to conservative treatment and a corticosteroid injection. He recently started a physical job at a warehouse which exacerbated symptoms. On examination, he had a BMI of 37. Gait evaluation was antalgic to the left, with neutral knee alignment. Previous surgical incisions were well healed. He had slight bilateral knee effusions. He had tenderness to palpation over the patellar tendons, pain with patellar compression, and painful range of motion of 0–120°, with no extension lag. Knees were stable to varus/valgus, anterior/posterior stress. His hip examination was unremarkable. Knee radiographs demonstrated severe patellofemoral dysplasia and degenerative changes, with mild degeneration over the medial joint space (Fig. 1). After extensive discussion of nonsurgical and surgical options, the patient elected to undergo bilateral sequential robotic-assisted patellofemoral knee arthroplasties (RA-PFKA), addressing the left side first.
Preoperative planning
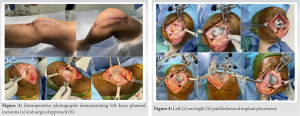
Extensive preoperative planning was undertaken to address the complex technical challenges faced by this case. Robotic-assisted PFA (RA-PFA) was chosen due to its limited invasiveness and increased precision in implant placement (Fig. 2). Planning objectives were to reconstruct the patellofemoral anatomy to allow for improved biomechanics while minimizing bone resection. A salvage plan for TKA was also created. Preoperative CT scanning was performed using the standard RA-TKA protocol (Stryker Mako, Mahwah, NJ). The resulting anatomical models demonstrated severe PF dysplasia and degeneration with relatively intact medial and lateral compartments on both knees.
PFA surgeries
After standard preparation for knee arthroplasty, old incisions were marked and the left knee was exposed using a limited anterior-midline incision (Fig. 3). A limited median para-patellar arthrotomy was made to enter the knee space through the previous scar. A large amount of normal-appearing joint fluid was encountered. The synovium was thickened, hypertrophic, and inflamed. The patella was exposed to reveal an abnormal articular surface. The trochlea demonstrated severe wear and deformity, with advanced degeneration of the patellofemoral joint. The medial and lateral tibiofemoral joints were normal and anterior cruciate ligament functional. Arrays were placed intra-incisional, the knee was registered and implant positioning planning was confirmed. Adjustments in positioning were made to allow adequate tracking and cartilage alignment. Cuts were made, and extensor mechanism realignment was performed to improve tracking. A mild lateral release was also required. A part of the old hardware over the lateral condyle was removed. The patella was resurfaced using a free-hand oscillating saw for placement of an asymmetric polyethylene implant. A burr was required to remove a metallic anchor from prior MPFL surgery. Trials were placed, showing excellent tracking, range of motion, and stability (Fig. 4). The components were cemented in place, and examination was confirmed, with satisfactory patellofemoral tracking. When closing the medial parapatellar approach, a medial plica closure was done to increase medial tension. Eight months after left PFA, the right side was approached in the same manner. Final components showed excellent tracking, range of motion, and stability (Fig. 4).
Postoperative course
Postoperatively, weight-bearing was limited to 75% body weight for the first 2 weeks. The patient was placed in an IROM knee brace, which was locked in extension for the first 4 weeks. Range of motion was then increased by 25° every 2 weeks after that.
Follow-up
At his latest follow-up, representing 2 years postoperatively from left PFA and 1 year postoperatively from right PFA, he reported no pain in the left knee and minimal pain over the right patellar tendon. He has achieved bilateral 0 to 120° knee range of motion without pain or feeling of instability. He has slight bilateral knee effusions. He continues to improve his quadriceps strength. Radiographs show slight bilateral patellar tilt, but overall well-positioned, centered patellas (Fig. 5). His patient-reported outcomes are presented in Table 1.
Isolated patellofemoral arthritis can present in younger patients with a history of childhood skeletal trauma, recurrent patellar subluxation, or trochlear dysplasia, among other pathologies [2, 4]. These patients usually maintain high-demand interests and professions and expect return to as full function as possible. They are also more likely to require revision surgery in their lifetime due to their young age if arthroplasty is to be performed [3, 5, 6, 7, 5, 8]. This case presented the complicated course of a young active man with severe isolated bilateral PF disease, with markedly compromised anatomy. In this setting, PFA offers a bone and ligament-preserving option that better maintains the natural kinematics of the knee compared to TKA. Recent research has shown RA-PFA to allow for a smaller incision, faster rehabilitation, bone stock preservation, and better implant alignment compared to TKA, ultimately providing a functional range of motion and return to high level of activity [12]. Moreover, a 2011 meta-analysis showed no significant differences in reoperation, revision, pain, or mechanical complications between second-generation PFA and TKA [7]. Studies agree that accurate implant positioning is crucial for the success of modern PFA, and recent research has shown that computer navigation and robotic assistance can reliably improve lower leg alignment, component positioning, and soft-tissue balancing compared to manual approaches [13]. This becomes even more evident in the setting of abnormal anatomies where anatomical patella-femoral landmarks are not evident. In a relevant recent study by Selvaratnam et al., RA-PFA was shown to provide close matching between preoperative planning and intraoperative implant placement, leading to improved short-term outcomes [11]. Ultimately, the decision of PFA versus TKA will be highly influenced by the severity of pathology in the medial and lateral compartments, symptomatology in these areas, and patient age, as well as surgeon preference and experience. We present a case of bilateral robotic-assisted PFA in a carefully selected young patient. Our approach allowed the patient to return to a physically demanding job without compromising potential conversion to TKA. Short-term results are promising, but longer follow-up is needed to assess long-term outcomes and implant survivorship.
RA-PFA can provide less invasive, accurate, and individualized treatment for younger patients with severe disease without compromising future conversion to TKA.
RA-PFA allows for a smaller incision, faster rehabilitation, bone stock preservation, and better implant alignment compared to TKA, ultimately providing a functional range of motion and return to high level of activity. This case presented the complicated course of a young active man with severe isolated bilateral PF disease, with markedly compromised anatomy. In this setting, PFA offers a bone and ligament-preserving option that better maintains the natural kinematics of the knee compared to TKA.
References
- 1.Strickland SM, Bird ML, Christ AB. Advances in patellofemoral arthroplasty. Curr Rev Musculoskelet Med 2018;11:221-30. [Google Scholar]
- 2.Johnson DS, Turner PG. Replacement for patellofemoral arthritis. Knee 2019;26:1166-70. [Google Scholar]
- 3.Leadbetter WB, Ragland PS, Mont MA. The appropriate use of patellofemoral arthroplasty: An analysis of reported indications, contraindications, and failures. Clin Orthop Relat Res 2005;436:91-9. [Google Scholar]
- 4.Grelsamer RP, Dejour D, Gould J. The pathophysiology of patellofemoral arthritis. Orthop Clin North Am 2008;39:269-74, v [Google Scholar]
- 5.Nicol SG, Loveridge JM, Weale AE, Ackroyd CE, Newman JH. Arthritis progression after patellofemoral joint replacement. Knee 2006;13:290-5. [Google Scholar]
- 6.Hutt J, Dodd M, Bourke H, Bell J. Outcomes of total knee replacement after patellofemoral arthroplasty. J Knee Surg 2013;26:219-23. [Google Scholar]
- 7.Dy CJ, Franco N, Ma Y, Mazumdar M, McCarthy MM, Valle AG. Complications after patello-femoral versus total knee replacement in the treatment of isolated patello-femoral osteoarthritis. A meta-analysis. Knee Surg Sports Traumatol Arthrosc 2012;20:2174-90. [Google Scholar]
- 8.Van der List JP, Chawla H, Zuiderbaan HA, Pearle AD. Survivorship and functional outcomes of patellofemoral arthroplasty: A systematic review. Knee Surg Sports Traumatol Arthrosc 2017;25:2622-31. [Google Scholar]
- 9.Cuthbert R, Tibrewal S, Tibrewal SB. Patellofemoral arthroplasty: Current concepts. J Clin Orthop Trauma 2018;9:24-8. [Google Scholar]
- 10.Lustig S. Patellofemoral arthroplasty. Orthop Traumatol Surg Res 2014;100:S35-43. [Google Scholar]
- 11.Selvaratnam V, Cattell A, Eyres KS, Toms AD, Phillips JRP, Mandalia VI. Robotic-assisted patellofemoral replacement-correlation of preoperative planning with intraoperative implant position and early clinical experience: A minimum 2-year follow-up. J Knee Surg 2022;35:731-8. [Google Scholar]
- 12.Turktas U, Piskin A, Poehling GG. Short-term outcomes of robotically assisted patello-femoral arthroplasty. Int Orthop 2016;40:919-24. [Google Scholar]
- 13.Van der List JP, Chawla H, Joskowicz L, Pearle AD. Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: A systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc 2016;24:3482-95. [Google Scholar]
- 14.Hassebrock JD, Makovicka JL, Wong M, Patel KA, Scott KL, Deckey DG, et al. Minimally invasive robotic-assisted patellofemoral arthroplasty. Arthrosc Tech 2020;9:e425-33. [Google Scholar]
- 15.Marchand RC, Sodhi N, Anis HK, Ehiorobo J, Newman JM, Taylor K, et al. One-year patient outcomes for robotic-arm-assisted versus manual total knee arthroplasty. J Knee Surg 2019;32:1063-8. [Google Scholar]
- 16.Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty 2007;22:1097-106. [Google Scholar]