In an elderly, consider TTCA with RIMN as a reliable salvage procedure for a post traumatic SA of ankle.
Dr. Gaurav Govil, Department of Orthopaedics, Max Super Speciality Hospital, Patparganj, Delhi, India. E-mail: gauravgovil@yahoo.co.in
Introduction: Posttraumatic secondary arthritis (SA) in the elderly with diabetes mellitus, osteoporosis, and neuromuscular affections has poor healing potential, leading to poor clinical and functional outcomes. Tibial talocalcaneal arthrodesis (TTCA) has been used to salvage for resultant hindfoot deformation. Retrograde intramedullary nailing (RIMN) has achieved reasonable fusion rates with improved functional outcomes.
Case Report: We report two cases of failed ankle surgery with progressive SA managed with curved RIMN to achieve TTCA. The American Orthopaedic Foot and Ankle Society Hindfoot scale, visual analog scale, radiologic assessment, and clinical examination were used to assess outcome measures. We achieved good ankle scores with pain-free independent mobilization at 4 months. At minimum 1-year follow-up, all had good hindfoot alignment, good fusion, and no implant loosening or failure.
Conclusion: Salvage TTCA with RIMN for a hindfoot SA can be a reliable technique to obtain good fusion, high satisfaction rate, and functional improvement following post-traumatic failed ankles in the elderly. The complex procedure has marked clinical improvement with the pain-free walking ability in an arthritic ankle, even with associated medical comorbidity.
Keywords: Hindfoot arthritis, hindfoot arthrodesis, tibial talocalcaneal arthrodesis, intramedullary nailing, secondary arthritis, failed ankle surgery.
Post-traumatic secondary arthritis (SA) incapacitates the elderly. A severe ankle deformity can be physically and mentally debilitating. The potential for healing in the elderly gets compounded by associated risk factors including diabetes mellitus (DM), rheumatoid arthritis, osteoporosis, neuropathy, smoking, and post-poliomyelitis residual paralysis [1, 2, 3]. Tibial talocalcaneal arthrodesis (TTCA) by retrograde intramedullary nailing (RIMN) for a failed ankle surgery presenting with SA gives reliable clinical and functional outcomes [4, 5]. However, the comorbid condition of DM, elderly age, and revision surgery are factors associated with a higher probability for failure and an eventual amputation [3]. We review the literature available to present a homogenous posttraumatic arthritic ankle group to guide management issues for the complex trauma. We report two cases of posttraumatic SA managed by RIMN fixation for TTCA with a high rate of patient satisfaction after attaining desirable clinical and functional outcomes. The compounding factors involved were DM, osteoporosis, and post-polio residual paralysis.
Case 1
A 73-year-old female slipped and fell at home and sustained an unstable subluxation of tri-malleolar fracture left ankle with an ipsilateral proximal fibular fracture (Fig. 1). She underwent ankle fixation surgery at a health-care facility elsewhere in another hospital with the fixation of medial and lateral pillars with plates, wires, and screws (Fig. 2). Her ankle was kept in support for almost 3 months with a non-weight-bearing protocol with the hope of sound union and functional recovery. However, she presented with a posttraumatic failed surgery with non-union and SA (Fig. 3).
Case 2
A 56-year-old female presented with a painful right ankle and considerable difficulty walking without pain and support for 3 months. Her right lower limb was affected by post-polio residual paralysis. She has a history of ankle fixation around 8 years back for a compound injury involving the talus and medial malleolus. She had an uneventful recovery and was ambulatory post-recovery without support. Her discomfort has increased gradually to incapacitate her to do daily routine activities without pain. She has healed scar marks along the right ankle region on the medial aspect with mild cavus deformity of the right foot. Radiographs show secondary arthritic changes with an implant in situ (Fig. 7). The acute phase reactants were normal. Poor healing potential with poor muscle mass posed challenges in the management. The surgical management included removing the implant, TTCA with RIMN, and below-knee cast application. Her postoperative period was uneventful, and no complications were noted. She progressed to the union in 14 weeks (Fig. 8). At the last follow-up of 1 year, the AOFAS ankle score improved from a preoperative score of 62–78 postoperatively. Her heel valgus was satisfactory, and she had no heel pain. She was graded as good with the clinical and functional improvement with radiological sound fusion (Fig. 9).
TTCA aims to provide a pain-free ankle with a stable hindfoot in a deformed foot [2, 6, 7]. 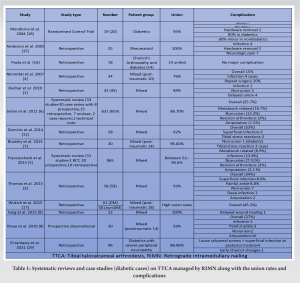
Surgeons can salvage a complex failed ankle injury with a sound ankle arthrodesis and stable fixation principles to allow an early return to pain-free walking ability with the advanced nailing procedure. The patient satisfaction rates are high with the achieved functional and clinical outcomes, and it further justifies the use of this procedure in the osteoporotic elderly.
TTCA with RIMN achieve sound fusion with a reliable satisfactory clinical and functional outcome in a failed posttraumatic arthritic ankle.
References
- 1.Budnar VM, Hepple S, Harries WG, Livingstone JA, Winson I. Tibiotalocalcaneal arthrodesis with a curved, interlocking, intramedullary nail. Foot Ankle Int 2010;31:1085-92. [Google Scholar]
- 2.Thomas AE, Guyver PM, Taylor JM, Czipri M, Talbot NJ, Sharpe IT. Tibiotalocalcaneal arthrodesis with a compressive retrograde nail: A retrospective study of 59 nails. Foot Ankle Surg 2015;21:202-5. [Google Scholar]
- 3.DeVries JG, Berlet GC, Hyer CF. Predictive risk assessment for major amputation after tibiotalocalcaneal arthrodesis. Foot Ankle Int 2013;34:846-50. [Google Scholar]
- 4.Niinimäki TT, Klemola TM, Leppilahti JI. Tibiotalocalcaneal arthrodesis with a compressive retrograde intramedullary nail: A report of 34 consecutive patients. Foot Ankle Int 2007;28:431-4. [Google Scholar]
- 5.Franceschi F, Franceschetti E, Torre G, Papalia R, Samuelsson K, Karlsson J, et al. Tibiotalocalcaneal arthrodesis using an intramedullary nail: A systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:1316-25. [Google Scholar]
- 6.Jehan S, Shakeel M, Bing AJ, Hill SO. The success of tibiotalocalcaneal arthrodesis with intramedullary nailing--a systematic review of the literature. Acta Orthop Belg 2011;77:644-51. [Google Scholar]
- 7.Brodsky JW, Verschae G, Tenenbaum S. Surgical correction of severe deformity of the ankle and hindfoot by arthrodesis using a compressing retrograde intramedullary nail. Foot Ankle Int 2014;35:360-7. [Google Scholar]
- 8.Klaue K, Wichelhaus A, Maik P, Mittlmeier T. The circular arc shaped nail for fixing the tibiotalocalcaneal arthrodesis. After clinical results. Injury 2019;50:23-31. [Google Scholar]
- 9.Fang Z, Claaßen L, Windhagen H, Daniilidis K, Stukenborg-Colsman C, Waizy H. Tibiotalocalcaneal arthrodesis using a retrograde intramedullary nail with a valgus curve. Orthop Surg 2015;7:125-31. [Google Scholar]
- 10.Mulligan RP, Adams SB Jr., Easley ME, DeOrio JK, Nunley JA 2nd. Comparison of posterior approach with intramedullary nailing versus lateral transfibular approach with fixed-angle plating for tibiotalocalcaneal arthrodesis. Foot Ankle Int 2017;38:1343-151. [Google Scholar]
- 11.Marley WD, Tucker A, McKenna S, Wong-Chung J. Pre-requisites for optimum centering of a tibiotalocalcaneal arthrodesis nail. Foot Ankle Surg 2014;20:215-20. [Google Scholar]
- 12.Belczyk R, Sung W, Wukich D. Technical tip: A simple method for proper placement of an intramedullary nail entry point for tibiotalocalcaneal or tibiocalcaneal arthrodesis. Foot Ankle J 2008;1(9):4. [Google Scholar]
- 13.Lemon M, Somayaji HS, Khaleel A, Elliott DS. Fragility fractures of the ankle: Stabilisation with an expandable calcaneotalotibial nail. J Bone Joint Surg Br 2005;87:809-13. [Google Scholar]
- 14.Ochman S, Evers J, Raschke MJ, Vordemvenne T. Retrograde nail for tibiotalocalcaneal arthrodesis as a limb salvage procedure for open distal tibia and talus fractures with severe bone loss. J Foot Ankle Surg 2012;51:675-9. [Google Scholar]
- 15.Anderson T, Linder L, Rydholm U, Montgomery F, Besjakov J, Carlsson A. Tibio-talocalcaneal arthrodesis as a primary procedure using a retrograde intramedullary nail: A retrospective study of 26 patients with rheumatoid arthritis. Acta Orthop 2005;76:580-7. [Google Scholar]
- 16.Paola LD, Volpe A, Varotto D, Postorino A, Brocco E, Senesi A, et al. Use of a retrograde nail for ankle arthrodesis in Charcot neuroarthropathy: A limb salvage procedure. Foot Ankle Int 2007;28:967-70. [Google Scholar]
- 17.Wukich DK, Mallory BR, Suder NC, Rosario BL. Tibiotalocalcaneal arthrodesis using retrograde intramedullary nail fixation: Comparison of patients with and without diabetes mellitus. J Foot Ankle Surg 2015;54:876-82. [Google Scholar]
- 18.Mendicino RW, Catanzariti AR, Saltrick KR, Dombek MF, Tullis BL, Statler TK, et al. Tibiotalocalcaneal arthrodesis with retrograde intramedullary nailing. J Foot Ankle Surg 2004;43:82-6. [Google Scholar]
- 19.El-Tantawy A, Atef A, Samy A. Trans-calcaneal retrograde nailing for secondary-displaced traumatic ankle fractures in diabetics with insensate feet: A less-invasive salvage-arthrodesis technique. Eur J Orthop Surg Traumatol 2022;32:37-46. [Google Scholar]
- 20.Gougoulias N, Oshba H, Dimitroulias A, Sakellariou A, Wee A. Ankle fractures in diabetic patients. EFORT Open Rev 2020;5:457-63. [Google Scholar]