Timely diagnosis and management of Lisfranc fracture dislocation can reduce significant morbidity.
Dr. Sivabalaganesh Amirthalingam, Department of Orthopaedics, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India. E-mail: sivabalaganeshamirthalingam@gmail.com
Introduction: Lisfranc injury is relatively rare and is commonly missed at the initial presentation as these injuries are easily misdiagnosed as a foot sprain. We report a case of chronic foot pain following an injury which was later diagnosed to be a neglected 6 weeks old complex Lisfranc fracture dislocation.
Case Report: A 53-year-old man presented with chronic foot pain and swelling which was diagnosed to be a neglected 6-week-old homolateral type of Lisfranc injury (type A Hard castle and Meyerson). We treated him with open reduction and internal fixation (ORIF) with plates and screws and achieved excellent functional outcome at 6-month follow-up period.
Discussion: Lisfranc injuries are frequently undetected with estimates ranging from 20% to 80%. Anteroposterior, lateral, and medial oblique views of the foot should be included in the radiological workup following a thorough physical examination. Our case will aid the deficient literature and guide the young surgeons in management of such cases.
Conclusion: Given the history and nature of the injury, it can be easily missed by a beginner and the clinician must keep a high index of suspicion when treating these injuries in emergency department. To prevent the many complications linked to this kind of injury, it requires a correct diagnosis and timely treatment in the form of closed/open reduction and fixation. Delayed presentation of such cases can be treated with ORIF and good functional outcome can be achieved.
Keywords: Neglected Lisfranc injury, chronic foot pain, type a hard castle, homolateral neglected Lisfranc.
Lisfranc injury is relatively rare and it is commonly missed at the initial presentation as these injuries are easily misdiagnosed as a foot sprain [1]. A Lisfranc injury is fracture dislocation of tarsometatarsal joint and it can vary from a simple injury involving one joint in the mid foot to a complex injury involving all the mid foot joints. It is characterized by traumatic disruption of Lisfranc ligament causing disruption in the articulation of medial cuneiform and the base of second metatarsal [2]. We report a case of 53-year-old male who presented to us with chronic foot pain following an injury which was later diagnosed to be a neglected complex Lisfranc fracture.
A 53-year-old gentle man presented with alleged history of fall from a twenty-foot tree and sustained closed injury over his left foot. Following the injury, he developed pain and swelling over his left foot and he was not able to weight bear weight on the injured limb. The patient underwent native splinting for 1 month. On removing the splint after 1 month, there was persistent pain and swelling over the left foot. The patient presented to us 6 weeks following the initial injury. There was a diffuse swelling and tenderness over the left mid foot region and the foot was grossly deformed. The patient was able to perform the ankle movements but the subtalar and mid foot joint movements were painful and restricted. The neurovascular status of the lower limb was intact. Radiographs taken at the time of presentation showed a neglected homogenous lateral type of Lisfranc injury (Fig. 1a, b and c). On careful examination of the radiographs, multiple chip fractures were present in the region of base of second metatarsal indicative of fleck sign (Fig. 1a). CT of the foot was not taken at the time of presentation. Multiple radiographic views including 30° oblique (Fig. 1c) were taken to ensure that other fractures are not missed. The patient was taken up for surgery after obtaining informed consent.

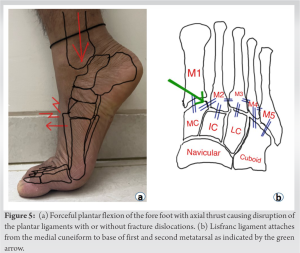
The name Lisfranc’s fracture originated from the French surgeon Jacques Lisfranc de St. Martin who first described the injury. He found midfoot injuries in the soldiers who fell from their horses with their foot “caught” in the stirrup of the horse saddle [3]. This causes forceful plantar flexion of the fore foot with axial thrust causing disruption of the plantar ligaments with or without fracture dislocations (Fig. 5a) [4]. Plantar ligaments and interosseous ligaments stabilize the tarsometatarsal joint. The second metatarsal acts as the keystone by anchoring itself between medial and lateral cuneiform [5]. The Lisfranc ligament attaches from the medial cuneiform to base of first and second metatarsal as indicated by the green arrow in (Fig. 5b) [6]. These structures all together form Lisfranc joint complex also known as the roman arch, as shown in (Fig. 5b) [7]. Lisfranc joint is a very complex joint and forms the transverse arch of the foot. The complex nature of the joint forms various fracture patterns during injury [2]. Even though the movements occurring in the tarsometatarsal ligament is limited, its stability is critical in the push off phase during walking. Normally during walking the mid foot transfers the forces generated by the calf muscles to the fore foot, leading to forward propulsion of the body. If a Lisfranc injury is left untreated, the uneven transfer of the force from mid foot to the forefoot through the unstable tarsometatarsal joint leads to collapse and flattening of the foot. This also acts as a shock absorber in the weight-bearing phase of the gait cycle [8]. These fractures tend to show a delayed presentation as they may be initially missed. In addition to being uncommon, Lisfranc injuries frequently go undetected and the estimates ranges from 20% to 80%. The incidence of misdiagnosis of a Lisfranc injury using only anteroposterior and lateral radiographs is around 20%. Using oblique view radiographs, this can be significantly reduced. Maintaining a high index of suspicion for these injuries and performing additional imaging, stress radiographs, weight-bearing radiographs, and CT scans will avoid missing these injuries [9]. In managing these injuries, Clark and Quint, in 1933, stressed the importance of adequate radiographic views to identify these fractures [10]. The continuity of medial border of second metatarsal with medial border of medial cuneiform and the continuity of medial border of fourth metatarsal with medial border of cuboids on anteroposterior view are the radiological features to assess proper reduction of these fractures. Anteroposterior, lateral, and medial oblique views should be included in the radiological workup following an a thorough physical examination [11]. Even 1 mm displacement of the second metatarsal base reduces the tarsometatarsal contact area by 13.1% [12]. Open reduction and internal fixation (ORIF) of these fracture with screws and Kirschner wire with good functional and satisfactory outcome has been emphasized in many studies [13]. A relatively similar neglected B2 type of neglected Lisfranc fracture has been treated successfully with Wagner external fixator and open reduction with screws [14]. Even delayed presentations with secondary arthritis have been treated surgically with good outcome [15, 16]. Nitinol staples have been used to treat similar fracture patterns to fuse the joint and had given good results [17]. The outcomes following conservative management vary widely; however, the conversion of conservative to surgical management rates is higher [18]. In our case, it was type A Hardcastle and Meyerson with total incongruity of the tarsometatarsal joint and displaced laterally. Since the injury was already 6 weeks old and it was difficult to reduce, excision of the base of metatarsals and arthrodesis of the tarsometatarsal joints had to be done. This did not affect the functional outcome as only negligible movement occurs in the tarsometatarsal joints.
Lisfranc injuries are commonly missed. Neglected Lisfranc fractures cause post-traumatic arthritis and chronic foot pain which causes significant morbidity. Given the history and nature of the injury, it can be easily missed by a beginner and the clinician must keep a high index of suspicion when treating these injuries in emergency department. To prevent the many consequences linked to this kind of injury, it requires a correct diagnosis and timely treatment in the form of closed/open reduction and fixation. Delayed presentation of such cases can be treated with ORIF and good functional outcome can be achieved.
Neglected Lisfranc injuries can be successfully treated with open reduction, “shortening,” arthrodesis, and internal fixation with a good outcome.
References
- 1.Burroughs KE, Reimer CD, Fields KB. Lisfranc injury of the foot: A commonly missed diagnosis. Am Fam Physician 1998;58:118-24. [Google Scholar]
- 2.Mascio A, Greco T, Maccauro G, Perisano C. Lisfranc complex injuries management and treatment: Current knowledge. Int J Physiol Pathophysiol Pharmacol 2022;14:161-70. [Google Scholar]
- 3.Fischer LP. Jacques Lisfranc de Saint-Martin (1787-1847). Hist Sci Med 2005;39:17-34. [Google Scholar]
- 4.Smith T, Ballard T, Ramanlal R, Butarbutar JC. Foot dislocation. In: StatPearls. Treasure Island: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554613 [Last accessed on 2022 Aug 08]. [Google Scholar]
- 5.Chaney DM. The Lisfranc joint. Clin Podiatr Med Surg 2010;27:547-60. [Google Scholar]
- 6.Chen J, Sagoo N, Panchbhavi VK. The Lisfranc injury: A literature review of anatomy, etiology, evaluation, and management. Foot Ankle Spec 2021;14:458-67. [Google Scholar]
- 7.Bumann H, Wonerow M. The forgotten brick: Case report of a Lisfranc injury with “pericuneiform” dislocation. Int J Foot Ankle 2021;5:57. [Google Scholar]
- 8.Dhillon S, Dhillon MS, Arumugam S, Gowda PK, Chabbra M, Kumar P. Foot biomechanics and relation to the gait cycle. J Foot Ankle Surg (Asia Pacific) 2018;5:68-72. [Google Scholar]
- 9.Moracia-Ochagavía I, Rodríguez-Merchán EC. Lisfranc fracture-dislocations: Current management. EFORT Open Rev 2019;4:430-44. [Google Scholar]
- 10.Clark DF, Quint HA. Dislocation of a single cuneiform bone. J Bone Joint Surg Am 1933;15:237-9. [Google Scholar]
- 11.Yan A, Chen SR, Ma X, Shi Z, MaCalus H. Updates on Lisfranc complex injuries. Foot Ankle Orthop 2021;6:2473011420982275 . [Google Scholar]
- 12.Yamamoto H, Furuya K, Muneta T, Ishibashi T. Neglected Lisfranc’s joint dislocation. J Orthop Trauma 1992;6:129-31. [Google Scholar]
- 13.Dayton SR, Krautmann KM, Boctor M, Tjong VK, Kadakia AR. Homolateral Lisfranc fracture/dislocation of 1st-5th metatarsals in a collegiate quarterback: A case study. Foot Ankle Orthop 2022;7:2473011421S00173 . [Google Scholar]
- 14.Kale DR, Khadabadi NA, Putti BB, Jatti RS. One month old neglected Lisfrancs fracture dislocation treated with Wagner’s external fixator and percutaneous screw fixation: A case report. J Orthop Case Rep 2014;4:42-6. [Google Scholar]
- 15.Van Rijn J, Dorleijn DM, Boetes B, Wiersma-Tuinstra S, Moonen S. Missing the Lisfranc fracture: A case report and review of the literature. J Foot Ankle Surg 2012;51:270-4. [Google Scholar]
- 16.Dharmshaktu GS. Neglected Lisfranc’s joint injury: A case report and literature review. Indian J Orthop Surg 2015;1:183-5. [Google Scholar]
- 17.Strickland CD, Dombrowsky AR, Conti MS, Irwin TA, Davis WH, Cohen BE, et al. Nitinol staple vs traditional plate osteosynthesis for primary arthrodesis of lisfranc injuries: A retrospective analysis. Foot Ankle Orthop 2022;7:2473011421S00957. [Google Scholar]
- 18.Guerreiro F, Abdelaziz A, Ponugoti N, Marsland D. Conservative management of Lisfranc injury: A systematic review. Foot Ankle Orthop 2022;7:2473011421S00680. [Google Scholar]