Clinicians should have a high degree of suspicion for infection and its complications even if they may mimic certain well-documented paediatric disorders and a thorough investigation should be done to aid in correct management.
Dr. Swapnil Keny, Professor and Head of Department, KB Bhabha Municipal Hospital, Bandra, Mumbai, Maharashtra, India. Email: swapnilkeny@hotmail.com
Introduction: Atypical and subacute presentations of pediatric bacterial septic arthritis are difficult to diagnose due to lack of systemic manifestations and inadequate laboratory data. Furthermore, they may mimic certain well-documented pediatric disorders to confound the diagnosis and management.
Case Report: The authors present a case of an adolescent obese male with features suggestive of a slipped capital femoral epiphysis (SCFE). Further investigations revealed bacterial septic arthritis which may have contributed to the slip. He was treated with an initial debridement followed by a definitive pelvic support osteotomy (PSO) with a compensatory distal femoral varus osteotomy. At 12 months, he had a satisfactory clinical and radiological outcome.
Conclusion: Clinicians should have a high degree of suspicion for infection in patients presenting with atypical clinical or radiological signs of SCFE. A thorough investigation in such cases is a must, to aid in correct management. PSO is an effective salvage procedure in adolescents with septic hip sequelae.
Keywords: Obese adolescent male, Slipped capital femoral epiphysis, Pelvic support osteotomy, Bacterial joint infection, Ilizarov hip reconstruction, Pediatric hip infection.
Despite advances in management, understanding, and interpretation, pediatric osteoarticular infections continue to pose diagnostic challenges for clinicians [1]. Atypical and subacute presentations without systemic signs of sepsis, of bacterial septic arthritis, are well documented. They are difficult to diagnose as they have an insidious onset with minimal symptoms, lack of systemic manifestations, and show inconclusive laboratory data [2, 3, 4, 5]. This is most probably attributed to good host immunity and decreased virulence of pathogens [1, 6]. On the other hand, slipped capital femoral epiphysis (SCFE) is a disorder of the proximal femoral physis of an immature hip [7, 8]. It involves an anterosuperior displacement of the metaphysis in relation to the femoral epiphysis [9, 10]. SCFE is classically seen in obese adolescent males presenting with acute or chronic hip or knee pain [10]. We present a case of an adolescent overweight male child, previously unreported, who presented to us with history and clinical features suggestive of an SCFE but proved to be a subacute bacterial septic arthritis on further investigations. The patient’s father provided informed consent regarding data submission for research and publication.
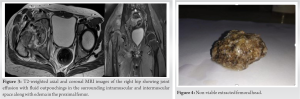
A 14-year-old adolescent male presented to us with complaints of non-traumatic right hip pain and painful limp for 1 month. The onset was insidious and gradually progressed to a stage where he was unable to bear weight on the affected limb. He remained systemically well and afebrile. He had a high pitched voice and a body mass index of 28.67 kg/m2. The patient had a Tanner’s stage of 4 which was one level below the level appropriate for his age. On examination, flexion, abduction, and internal rotation were restricted, with a 1 cm shortening on the right side. No local rise of temperature or skin discoloration was seen. Plain radiographs showed a discontinuity and a relative displacement suggestive of an SCFE (Fig. 1). Sclerotic focus at the separation site raised a suspicion which was evaluated with a CT scan of the hip. This revealed a cleavage and cortical separation at the subcapital region with lysis and fragmentation at the head-neck junction (Fig. 2).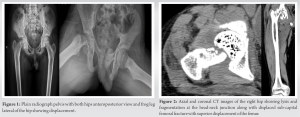

Literature Review
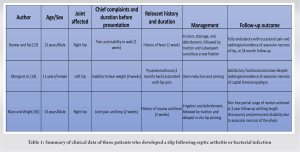
A literature search was performed with PubMed search engine of the National Library of Medicine of the Institutes of Health (http://www.ncbi.nlm.nih.gov/pubmed) using following combinations of keywords: “Slipped capital femoral epiphysis”; or “SCFE”; or “Slipped upper femoral epiphysis’” (SUFE); or ‘’SUFE” and “Subacute bacterial infection” or “Septic arthritis” or “Pediatric hip osteomyelitis”. Our search strategy was restricted to cases only involving a slip following septic arthritis or bacterial infection. We included only English-language publications with no date limitations (Table 1).
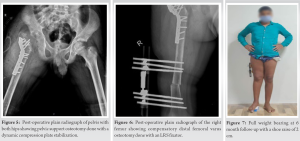
SCFE also known as SUFE is the most common hip disorder in 8–15-year-old children, involving an epiphyseal-metaphyseal separation of the proximal femur [9, 11]. The term SCFE is a misnomer, because the epiphysis is held in the acetabulum by the ligamentum teres, and it is the metaphysis which actually moves proximally and anteriorly while the epiphysis remains in the acetabulum [11, 12]. It is associated with various etiologies such as obesity, endocrine abnormalities, male sex, and steeper orientation of the proximal femoral physis [13]. Epiphyseal separation secondary to infection is known to occur around infancy, but occurrence in adolescents is very rare [14, 15]. Subacute bacterial arthritis is characterized by moderate localized bone pain and may occur without any systemic manifestation and non-contributory laboratory results [6]. Our patient presented with a coexisting infection and physeal slip. Subacute infection, leading to a secondary growth plate damage and a subsequent slip, was our initial hypothesis. An alternative hypothesis could have been the presence of a subacute hematoma following a slip, which probably got infected. It is difficult to precisely point out the sequence of events, but we feel the former scenario is more likely for several reasons. The presence of lysis and fragmentation at the physeal junction on radiographs as well as CT scan, pointed more toward an infection preceding a slip [16]. Furthermore, the relative anterosuperior orientation of the metaphysis in relation to the epiphysis, as seen in a classic SCFE, was not evident on radiographs and CT scan [12]. Another point favoring the former scenario is that a slipped epiphysis, as a complication of septic arthritis, is well documented in children of the pre-antibiotic era [17, 18]. The patient had a high-pitched voice and Tanner’s staging lower for his chronological age. The above-mentioned features are seen in adiposogenital syndrome which is commonly associated with SCFE [19]. This favored our latter hypothesis [13, 20]. The presence of an MRSA infection for a month with the child being systemically asymptomatic favored the latter hypothesis too [21]. However, we did not find any evidence of MRSA colonization on his body. MRSA is a leading cause of osteoarticular infection in children [22]. On axilla, body, and nasal nare screening, no foci of MRSA colonization were found. Despite lack of any clear source of infection or past history of admission to the hospital, a hematogenous seeding to the hip with a possibility of the child being an MRSA carrier, could be a possible explanation [23]. Treatment of chronic hip joint pathologies is a challenging task and management and in such situations is aimed at achieving a painless, stable, and functional mobile hip with minimal LLD [24, 25]. After debridement and femoral head removal in our case, we were left with a deficient/unstable hip. The most appropriate treatments for these kinds of hips, currently, are PSO and total hip replacement (THR) [26]. Young age and need for multiple revision surgeries precluded the option of a THR [26]. Furthermore, THR in a deficient hip is technically difficult with possible complications of excessive shortening, femoral or sciatic nerve palsies, post-operative dislocations, and aseptic loosening [26]. Arthrodesis was not considered due to disadvantages of chronic back pain, contralateral hip and knee pain, and loss of range of motion in the long run [27]. Hence, we planned for a PSO with Ilizarov modification (Ilizarov hip reconstruction) in a two staged manner [28]. In the first stage, we performed a proximal subtrochanteric valgus osteotomy with a DCP, 6 weeks after which a distal femur varus osteotomy was done with an LRS fixator over which lengthening was performed. The former procedure increased the contact surface area between the femur and pelvis thus preventing proximal migration of the femur. It also increased the distance between origin and insertion of abductor muscles, thereby improving abductor efficiency and hip biomechanics [29]. The latter procedure corrected the LLD and mechanical axis of the leg [28]. At 1-year follow-up, our patient had minimal leg length discrepancy with a painless complete weight bearing walk and a satisfactory outcome. After a thorough review of literature (Table 1) and to the best of our knowledge, we can say that this is perhaps the only case of a physeal slip or fracture as sequelae of a subacute bacterial infection to be managed with a PSO using the Ilizarov’s modification.
This report highlights that a pathological fracture or physeal slip secondary to a subacute infection should be kept in the differentials for a patient presenting with typical clinical features of an SCFE. Furthermore, in such cases, one needs to have a high suspicion for an alternative diagnosis when radiographs show atypical features such as sclerosis and lysis. This study shows the importance of confirmatory three dimensional imaging in adding to the diagnosis and further management, hence, reinforcing the importance of doing a thorough investigation before management for the same. This case report highlights that PSO is an effective salvage procedure in adolescents with septic hip sequelae.
Atypical and subacute presentations of pediatric bacterial septic arthritis are difficult to diagnose due to lack of systemic manifestations and inadequate laboratory data. Clinicians should have a high degree of suspicion for infection even if they may mimic certain well-documented pediatric disorders. A thorough investigation in such cases is a must, to aid in correct management. PSO is an effective salvage procedure in adolescents with septic hip sequelae.
References
- 1.Iliadis AD, Ramachandran M. Paediatric bone and joint infection. EFORT Open Rev 2017;2:7-12. [Google Scholar]
- 2.Ezra E, Cohen N, Segev E, Hayek S, Lokiec F, Keret D, et al. Primary subacute epiphyseal osteomyelitis: Role of conservative treatment. J Pediatr Orthop 2002;22:333-7. [Google Scholar]
- 3.Ezra E, Wientroub S. Primary subacute haematogenous osteomyelitis of the tarsal bones in children. J Bone Joint Surg Br 1997;79:983-6. [Google Scholar]
- 4.Gillespie WJ, Moore TE, Mayo KM. Subacute pyogenic osteomyelitis. Orthopedics 1986;9:1565-70. [Google Scholar]
- 5.Gledhill RB. Subacute osteomyelitis in children. Clin Orthop Relat Res 1973;96:57-69. [Google Scholar]
- 6.Spyropoulou V, Chargui AD, Merlini L, Samara E, Valaikaite R, Kampouroglou G, et al. Primary subacute hematogenous osteomyelitis in children: A clearer bacteriological etiology. J Child Orthop 2016;10:241-6. [Google Scholar]
- 7.Fahey JJ, O’Brien ET. Acute slipped capital femoral epiphysis: Review of the literature and report of ten cases. J Bone Joint Surg Am 1965;47:1105-27. [Google Scholar]
- 8.Novais EN, Millis MB. Slipped capital femoral epiphysis: Prevalence, pathogenesis, and natural history. Clin Orthop Relat Res 2012;470:3432-8. [Google Scholar]
- 9.Johns K, Mabrouk A, Tavarez MM. Slipped capital femoral epiphysis. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. [Google Scholar]
- 10.Harris JB, Sunil B, Ryan MK, Beauchamp G. Association of slipped capital femoral epiphysis with panhypopituitarism due to pituitary macroadenoma: A case report. J Investig Med High Impact Case Rep 2021;9:2324709621999956 . [Google Scholar]
- 11.Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD. Acute slipped capital femoral epiphysis: The importance of physeal stability. J Bone Joint Surg Am 1993;75:1134-40. [Google Scholar]
- 12.Peck D. Slipped capital femoral epiphysis: Diagnosis and management. Am Fam Physician 2010;82:258-62. [Google Scholar]
- 13.Barwar N, Rai A. Delayed slipped capital femoral epiphysis following septic arthritis of a hip: A case report. J Orthop Case Rep 2021;11:99-101. [Google Scholar]
- 14.Monga P, Jagannath CS, Verma R, Sharma VK. Complete slipping of the capital femoral epiphysis after hematogenous osteomyelitis. Can J Surg 2003;46:59-60. [Google Scholar]
- 15.Choi IH, Pizzutillo PD, Bowen JR, Dragann R, Malhis T. Sequelae and reconstruction after septic arthritis of the hip in infants. J Bone Joint Surg Am 1990;72:1150-65. [Google Scholar]
- 16.Ogden JA. Pediatric osteomyelitis and septic arthritis: The pathology of neonatal disease. Yale J Biol Med 1979;52:423-48. [Google Scholar]
- 17.Badgley CE, Yglesias L, Perham WS, Snyder CH. Study of the end results in 113 cases of septic hips. J Bone Joint Surg 1936;18:1047-61. [Google Scholar]
- 18.Green WT. Osteomyelitis in infancy. JAMA 1935;105:1835-9. [Google Scholar]
- 19.Samelis PV, Papagrigorakis E, Konstantinou AL, Lalos H, Koulouvaris P. Factors affecting outcomes of slipped capital femoral epiphysis. Cureus 2020;12:e6883. [Google Scholar]
- 20.Guzzanti V, Falciglia F, Stanitski CL. Slipped capital femoral epiphysis in skeletally immature patients. J Bone Joint Surg Br 2004;86:731-6. [Google Scholar]
- 21.Turner NA, Sharma-Kuinkel BK, Maskarinec SA, Eichenberger EM, Shah PP, Carugati M, et al. Methicillin-resistant Staphylococcus aureus: An overview of basic and clinical research. Nat Rev Microbiol 2019;17:203-18. [Google Scholar]
- 22.Kaushik A, Kest H. Pediatric methicillin-resistant Staphylococcus aureus osteoarticular infections. Microorganisms 2018;6:40. [Google Scholar]
- 23.Mollema FP, Severin JA, Nouwen JL, Ott A, Verbrugh HA, Vos MC. Successful treatment for carriage of methicillin-resistant Staphylococcus aureus and importance of follow-up. Antimicrob Agents Chemother 2010;54:4020-5. [Google Scholar]
- 24.Rozbruch SR, Paley D, Bhave A, Herzenberg JE. Ilizarov hip reconstruction for the late sequelae of infantile hip infection. J Bone Joint Surg Am 2005;87:1007-18. [Google Scholar]
- 25.Metikala S, Kurian BT, Madan SS, Fernandes JA. Pelvic support hip reconstruction with internal devices: An alternative to ilizarov hip reconstruction. Strategies Trauma Limb Reconstr 2020;15:34-40. [Google Scholar]
- 26.Pafilas D, Nayagam S. The pelvic support osteotomy: Indications and preoperative planning. Strategies Trauma Limb Reconstr 2008;3:83-92. [Google Scholar]
- 27.Umer M, Quadri TA, Rashid RH. Ilizarov hip reconstruction osteotomy - A review. Int J Surg 2018;54:351-5. [Google Scholar]
- 28.Emara KM. Pelvic support osteotomy in the treatment of patients with excision arthroplasty. Clin Orthop Relat Res 2008;466:708-13. [Google Scholar]
- 29.El-Mowafi H. Outcome of pelvic support osteotomy with the Ilizarov method in the treatment of the unstable hip joint. Acta Orthop Belg 2005;71:686-91. [Google Scholar]
- 30.Marx RG, Wright JG. Slipped capital femoral epiphysis after septic arthritis of the hip in an adolescent: Report of a case. Can J Surg 1999;42:145-8. [Google Scholar]